Translate this page into:
“Hypopyon” sign in dermatology
Corresponding author: Dr. Vishal Gaurav, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Danish M, Patel VM, Gaurav V. “Hypopyon” sign in dermatology. Indian J Dermatol Venereol Leprol. 2024;90:128-132. doi: 10.25259/IJDVL_654_2023
Introduction
The “hypopyon sign” is a distinctive clinical manifestation characterised by the presence of small, discrete vesicles that can be either flaccid or tense. The vesicles initially contain clear fluid which subsequently becomes turbid and eventually pustular, either due to intense neutrophilic inflammation or secondary bacterial infection, resulting in the accumulation of pus, predominantly in the lower half, of the corresponding pustules. When a patient exhibiting the hypopyon sign assumes a standing position, a unique visual characteristic becomes apparent. Within the pustule, a transverse fluid level can be observed, consisting of purulent material that settles at the bottom. This fluid level, positioned horizontally within the pustule, is specifically referred to as the hypopyon sign.1
This particular sign is commonly observed in two types of conditions: pyodermas, which are infectious skin disorders characterised by the presence of pus, and vesiculobullous disorders. Examples of the latter include pemphigus, bullous pemphigoid and linear IgA dermatosis.
The presence of the hypopyon sign serves as a valuable clinical indicator of the severity of infection and inflammation in these conditions. Its identification aids in the diagnosis and management of patients, providing crucial insights into the extent of the disease and secondary bacterial infection and the need for appropriate treatment interventions.
In this article, we aim to compile an extensive inventory of dermatological conditions that are commonly and less commonly associated with the presence of the hypopyon sign. The identified conditions have been categorised into two main groups: autoimmune/inflammatory dermatoses and infectious dermatoses. This comprehensive list aims to provide a valuable resource for a better understanding and recognition of dermatological disorders associated with the hypopyon sign.
-
Autoimmune/inflammatory dermatoses
-
Pemphigus vulgaris
Pemphigus vulgaris is characterised by flaccid vesiculobullous lesions that rapidly rupture to form painful erosions. In some cases, patients may exhibit intact blisters where a collection of pus can be observed at the base, distinctively separated from clearer fluid at the top. This characteristic separation of fluids within the blister is commonly referred to as the “hypopyon sign” [Figure 1].2
 Figure 1:
Figure 1:- A 35-year-old woman with pemphigus vulgaris showing flaccid bullae with “hypopyon” (blue arrow).
-
Pemphigus foliaceous
Pemphigus foliaceous commonly presents with itchy recurrent shallow erosions with crusting and scaling, predominantly in a seborrheic distribution. Occasionally, patients may have intact blisters that contain sterile pus and as a result of gravitational pull in dependent areas, the pus settles in the lower half of the lesion leading to the formation of a “hypopyon” [Figure 2].2
 Figure 2:
Figure 2:-
A young woman with pemphigus foliaceous showing small superficial vesicles with “hypopyon” (blue arrow).
-
IgA pemphigus
IgA pemphigus is a rare autoimmune intraepidermal blistering disorder presenting as painful and pruritic flaccid pustules on an erythematous base that quickly ruptures to form erosions that later develop crusting. Hypopyon sign has been reported in IgA pemphigus.3
-
Paraneoplastic pemphigus
Paraneoplastic pemphigus is an autoimmune blistering paraneoplastic condition characterised by severe mucositis and variable cutaneous manifestations. Hypopyon sign can be seen in paraneoplastic pemphigus due to intense inflammation.4
-
Bullous pemphigoid
Bullous pemphigoid represents a chronic autoimmune blistering disorder affecting the subepidermal layer. The cutaneous symptoms of this condition are highly diverse, encompassing both non-bullous and bullous phases. In the bullous phase, tense vesicles or bullae typically appear on urticarial plaques or unaffected skin. These fluid-filled lesions which contain clear or haemorrhagic fluid, are often accompanied by itching. It is worth noting that although rare, the presence of the hypopyon sign may accompany the bullae in some cases of bullous pemphigoid [Figure 3].2
 Figure 3:
Figure 3:-
A 40-year-old man with bullous pemphigoid showing tense bulla with “hypopyon” (blue arrow).
-
Chronic bullous disease of childhood and linear IgA disease
Chronic bullous disease of childhood is an autoimmune blistering disease that primarily affects children. Linear IgA represents an adult variant of the disease. Characteristic lesions include a cluster of jewel-like or annular arrangement of vesicles, often involving the peri-oral area. The bullae in chronic bullous disease of childhood typically contain clear fluid, although there are instances where the lower half of the blister may contain yellow fluid resulting in a distinct half-and-half appearance of the blisters.5
-
Sub-corneal pustular dermatosis
Sub-corneal pustular dermatosis, also known as Sneddon–Wilkinson syndrome, is an uncommon pustular dermatosis characterised by the presence of sterile pustules presenting in a symmetrical distribution pattern, often affecting the trunk, intertriginous areas (particularly the axillae) and flexures of the upper and lower limbs. The pustular eruption emerges as small pustules on a normal or slightly erythematous base. A distinct visual feature of these pustules is the presence of a clear demarcation line dividing them horizontally into two halves, the upper zone containing clear fluid and the lower zone containing yellowish-white turbid fluid. This gives rise to a characteristic “half-half” appearance or a “hypopyon pustule”.6 Hypopyon sign is classically described with sub-corneal pustular dermatosis.
-
Pustular psoriasis
Generalised pustular psoriasis presents with an acute eruption characterised by multiple sterile pustules on an erythematous and oedematous background accompanied by systemic features. In some cases, multiple pustules, especially those located on the back in dependent positions, exhibit a clear horizontal demarcation with pus settling in the lower portion of the pustule giving rise to a hypopyon. Although it may not be readily apparent during a clinical examination, the presence of this feature can be easily visualised using a dermoscope [Figures 4a and 4b].7
 Figure 4a:
Figure 4a:-
A 25-year-old man with pustular psoriasis showing a well-defined erythematous plaque with overlying pustules.
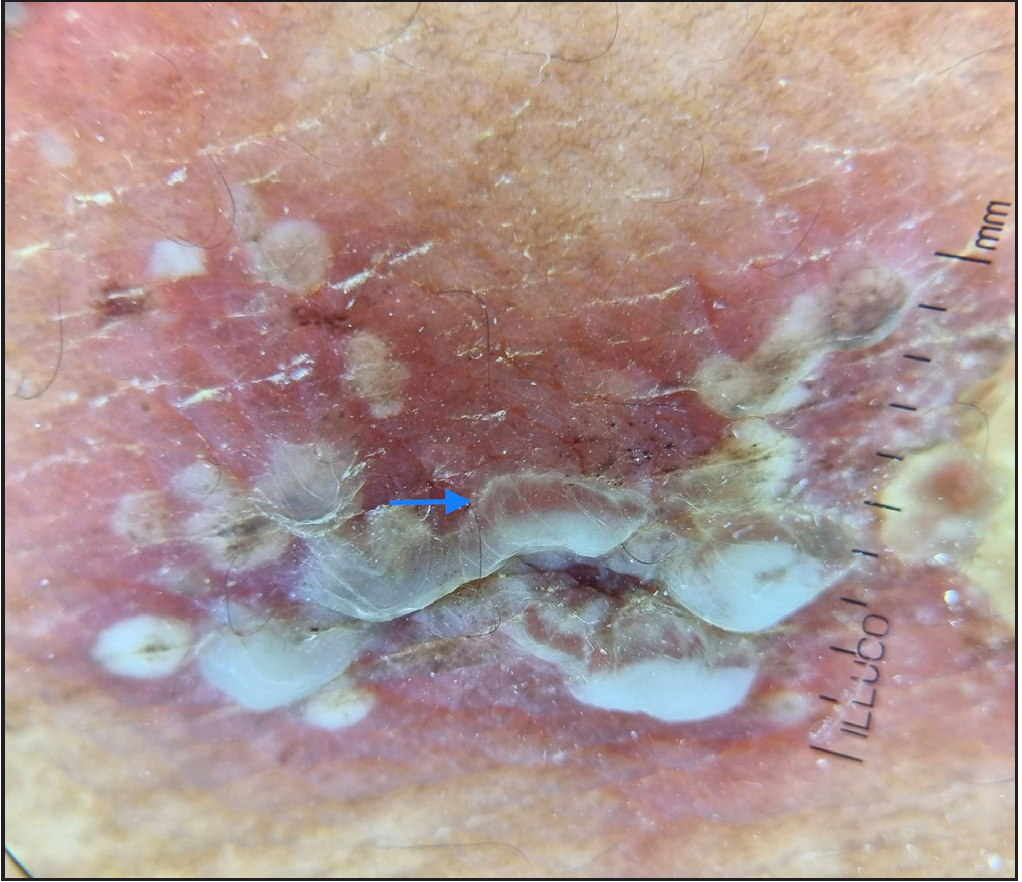 Figure 4b:
Figure 4b:- Dermoscopy showing micro-pustules with “hypopyon” (blue arrow) (10×; polarised).
-
Acute generalised exanthematous pustulosis
Acute generalised exanthematous pustulosis presents with multiple small, sterile, non-follicular pustules on an erythematous base with no or minimal mucous membrane involvement. The distribution favours the trunk and intertriginous regions. Acute generalised exanthematous pustulosis is typically pruritic. Some of the larger pustules can show settling of pus in the lower half of the lesion with a clear demarcation at the horizontal level (hypopyon sign). Similar to pustular psoriasis, these pustules may not be discernible during a clinical examination due to their small size. In such cases, the use of a dermoscope may be necessary to accurately visualise and evaluate them.8
-
-
Infections
-
Bullous impetigo
Bullous impetigo is a bacterial skin infection primarily affecting infants and children, caused by Staphylococcus aureus. It is characterised by the presence of vesicles, bullae and crusted erosions. The bullae in bullous impetigo are non-sterile and exhibit a distinct appearance with pus accumulating in the lower half of the lesion, while the upper half contains clear fluid, leading to hypopyon formation. It can also be seen in staphylococcal scalded skin syndrome [Figure 5].9
 Figure 5:
Figure 5:-
A 5-year-old girl with bullous impetigo on the face showing multiple flaccid bulla with “hypopyon” (blue arrows).
-
Varicella
Varicella-zoster virus infection, also known as chickenpox, is characterised by generalised small itchy vesicles on erythematous skin which eventually scabs over time. The most common complication is bacterial superinfection by Staphylococcus aureus and superficial skin infections. Vesicles of varicella can develop pus leading to formation of pus-filled flaccid blisters which can show a transverse fluid level due to accumulation of pus in the lower half (hypopyon sign) [Figure 6].10
 Figure 6:
Figure 6:-
A 7-year-old boy with varicella showing a vesicle with “hypopyon” (blue arrow).
-
Cutaneous candidiasis
Cutaneous candidiasis is a fungal infection caused by candida species that primarily affects the skin and mucous membranes. It presents as red, itchy rashes with satellite pustules, commonly occurring in warm and moist areas of the body, such as skin folds. These pustules have perilesional erythema. It occurs more frequently in immunocompromised individuals or neonates. In some instances, the satellite pustules may exhibit the accumulation of pus in the lower portion of the pustule, leading to the formation of a hypopyon [Figures 7a and 7b].11
 Figure 7a:
Figure 7a:-
A 4-year-old boy with cutaneous candidiasis showing small satellite pustules with peri-lesional erythema involving the neck fold.
 Figure 7b:
Figure 7b:-
A 4-year-old boy with cutaneous candidiasis showing a tiny vesicle with “hypopyon” (blue arrow).
-
-
Miscellaneous
-
Lymphangioma circumscriptum
The “red” hypopyon sign, observed through dermoscopy, is a notable characteristic of lymphangioma circumscriptum. This sign refers to the presence of red fluid or blood settled at the bottom of vesicles or lacunae, while the upper portion contains clear or pale fluid. It indicates the presence of vascular congestion or haemorrhage within the lymphatic vessels [Figures 8a and 8b]. However, the term “red hypopyon” is misleading because it describes the presence of red fluid or blood rather than the presence of pus. The red hypopyon sign aids in differentiating lymphangioma circumscriptum from other skin conditions and plays a crucial role in its diagnosis.12
 Figure 8a:
Figure 8a:-
A 20-year-old man with lymphangioma circumscriptum showing multiple clear fluid-filled vesicles with “red-hypopyon”.
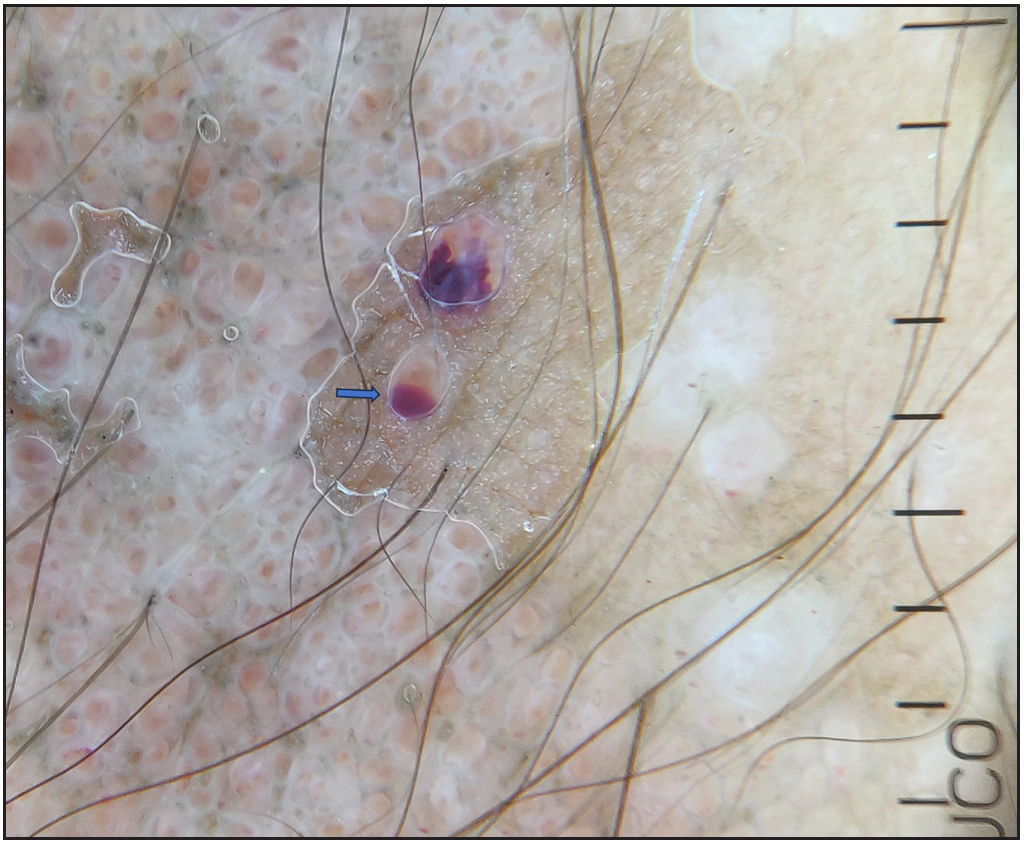 Figure 8b:
Figure 8b:- Dermoscopy showing lacunae with “red-hypopyon” (blue arrow) (10×, polarised).
-
Cutaneous angiosarcoma
Angiosarcoma is a rare malignant tumour originating from blood vessels. Cutaneous angiosarcomas can be classically present over head and neck area or, be linked to persistent lymphedema (Stewart-Treves syndrome) or radiation-induced. Dermoscopy can show “red hypopyon” in lymphedema-associated angiosarcoma, possibly indicating an underlying lymphatic stasis.13
-
Conclusion
The hypopyon sign can be observed in various conditions including autoimmune/inflammatory dermatoses such as pemphigus vulgaris, pemphigus foliaceous, bullous pemphigoid, chronic bullous disease of childhood and sub-corneal pustular dermatosis as well as infectious dermatoses like bullous impetigo and varicella. It indicates either secondary infection or intense inflammation within the blisters.
Declaration of patient consent
The authors certify that they have obtained appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Eponymous signs in dermatology. Indian Dermatol Online J. 2012;3:159-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hypopyon sign in pemphigus vulgaris and pemphigus foliaceus. Int J Dermatol. 2009;48:1100-2.
- [CrossRef] [PubMed] [Google Scholar]
- IgG/IgA pemphigus with differing regional presentations. JAAD Case Rep. 2022;28:119-22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hipopiyon belirtisi saptanan bir paraneoplastik pemfigus olgusu ve literatür incelemesi [A case of paraneoplastic pemphigus with hypopyon sign and literature review] Pam Med J. 2018;11:81.
- [Google Scholar]
- Chronic bullous disease of childhood: A case report and review of literature of bullous diseases in children. Nepal J Dermatol Venereol Leprol. 2022;20:69-75.
- [Google Scholar]
- Subcorneal pustular dermatosis: Comprehensive review and report of a case presenting during pregnancy. Int J Womens Dermatol. 2020;6:131-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Half-filled or half-empty: Conundrum of “Hypopyon Sign” in pustular psoriasis. Indian J Rheumatol. 2022;17:318-9.
- [Google Scholar]
- Pustular psoriasis and acute generalized exanthematous pustulosis. Medicina (Kaunas). 2021;57:1004.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous signs in infectious diseases. Indian J Dermatol Venereol Leprol. 2022;88:569-75.
- [CrossRef] [PubMed] [Google Scholar]
- Hypopyon sign as an unusual complication of varicella infection in a girl with atopic dermatitis. Wien Med Wochenschr. 2021;171:61-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous candidiasis: An evidence-based review of topical and systemic treatments to inform clinical practise. J Eur Acad Dermatol Venereol. 2019;33:1863-73.
- [CrossRef] [PubMed] [Google Scholar]
- Hypopyon-like features: New dermoscopic criteria in the differential diagnosis of cutaneous lymphangioma circumscriptum and haemangiomas? J Eur Acad Dermatol Venereol. 2012;26:1023-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hypopyon sign in dermatoscopy of cutaneous angiosarcoma. Australas J Dermatol. 2019;60:e366-e368.
- [CrossRef] [PubMed] [Google Scholar]






