Translate this page into:
Clinical and dermoscopic improvement of angiokeratoma in a child with topical rapamycin
Corresponding author: Dr. Bahareh Abtahi-Naeini, Department of Pediatric Dermatology, Imam Hossein Children’s Hospital, Isfahan University of Medical Sciences, Isfahan-1, Isfahan, Iran. abtahi.bahareh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Farajzadeh S, Pardakhty A, Afshar K, Abtahi-Naeini B. Clinical and dermoscopic improvement of angiokeratoma in a child with topical rapamycin. Indian J Dermatol Venereol Leprol. 2024;90:136. doi: 10.25259/IJDVL_1008_2022
Dear Editor,
A 5-year-old boy presented with clinical and dermoscopic features of angiokeratoma from infancy. Cutaneous findings included a well-circumscribed non-tender plaque of 5 × 6 cm size, studded with multiple erythematous to purplish, verrucous papules on the proximal part of the thigh [Figure 1a]. Although the lesion resembled a lymphangioma, the dermoscopic feature of prominent blue-whitish veil and the red lacuna in conjunction with the dark lacuna argued for angiokeratoma [Figure 1b]. The boy’s parents refused any physical treatment due to past history of severe bleeding during pulsed dye laser (PDL) treatment. Hence topical rapamycin (sirolimus) ointment 0.04% was recommended.
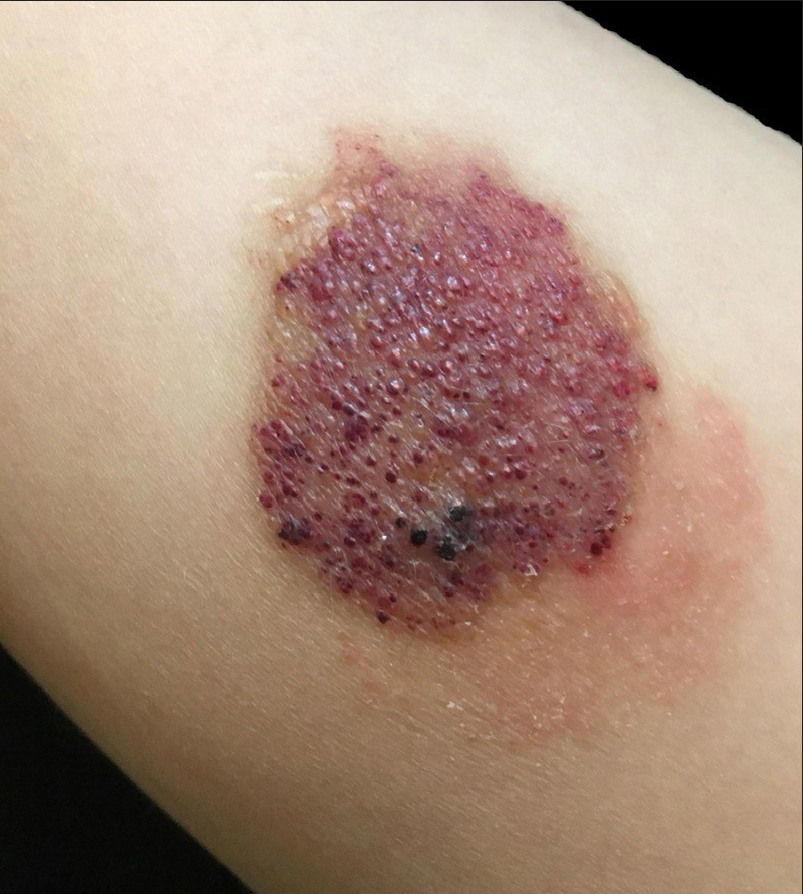
- Clinical features of the lesion before treatment.
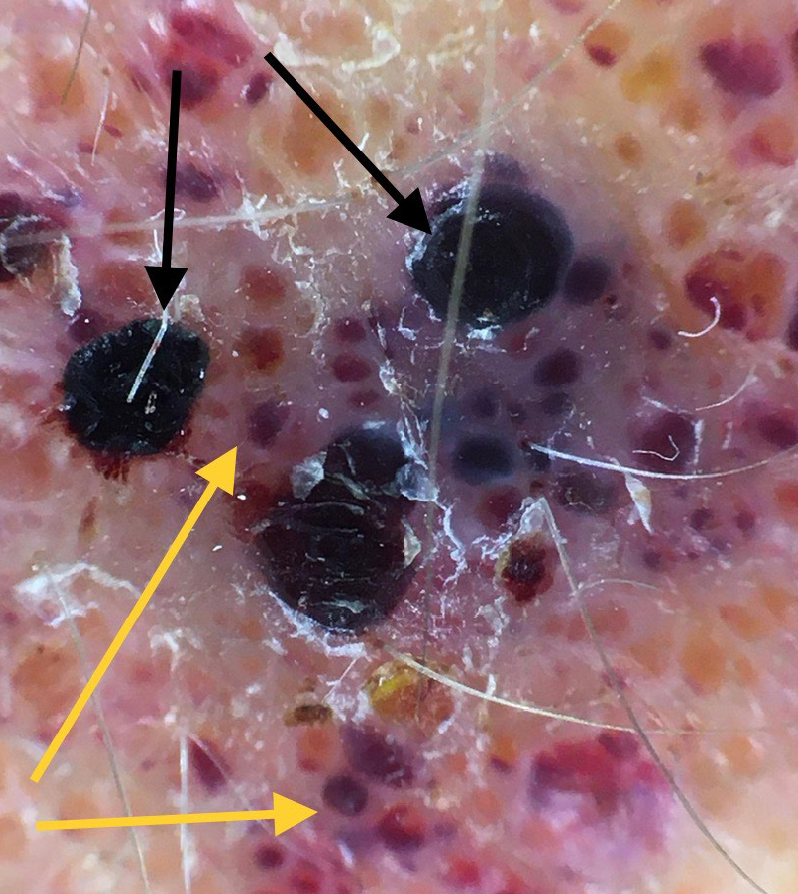
- The dermoscopic image of angiokeratoma shows the well-demarcated round red (yellow arrow) to dark (black arrow) lacuna, (80× magnification, FotoFinder video dermoscopy).
Rapamycin 0.04% ointment was prepared from 1 mg sirolimus (rapamune®) tablets ground to a fine powder with a mortar and pestle at the pharmacy. 2ml of ethanol with an exact concentration of 96 degree and 1 ml of 50 % propylene glycol were used to dissolve the active ingredient and form a paste. Eucerin was added to the paste and mixed to form an ointment. The formulation was applied twice daily as a thin layer of ointment on the surface of the affected skin.
Improvement occurred during the four-week treatment. After three months, more than 80% of the vascular component of the lesions disappeared, and the color of the lesion changed to light yellow [Figure 1c]. The vascular component regressed after treatment [Figure 1d].

- Three months after treatment with topical rapamycin.
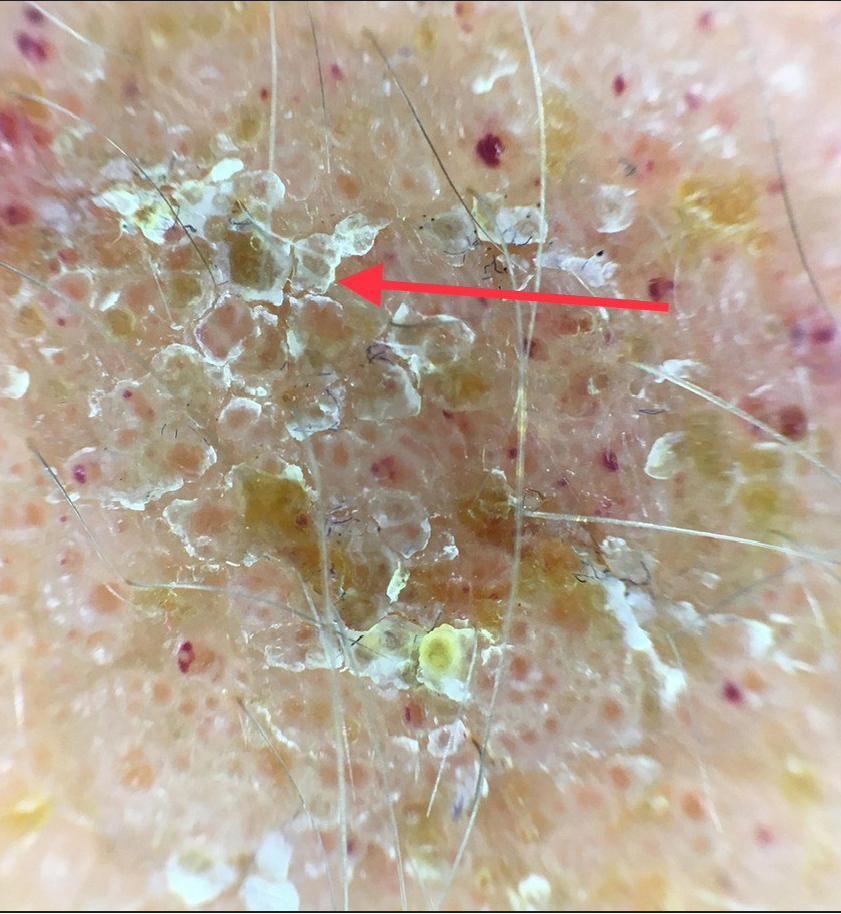
- Improvement of the vascular component and development of white-to-red scale (red arrow) after treatment (80× magnification, FotoFinder video dermoscopy).
The treatment was stopped after the disappearance of the vascular component in the lesion, and the child was followed clinically and dermoscopically for recurrences and other complications for six months. There were no any complications or recurrence in this period.
There is no standard treatment guideline or stepwise approach for the treatment of angiokeratomas. Treatment is usually difficult, especially in children. Clinical improvement of vascular lesions with topical application of rapamycin has been reported in several cases,1 suggesting that administration of the topical form of this drug may be a potentially promising option for the treatment of angiokeratoma. The mechanism of action of rapamycin is an interaction with the mammalian target of rapamycin (mTOR) signaling, which acts on the expression of vascular endothelial growth factor (VEGF). Inhibition by rapamycin halts the production of this factor and cellular proliferation, results in its efficacy on vascular proliferation.1
It seems that topical rapamycin is a promising agent for inhibiting the activity and proliferation of the vascular component. At present, there is limited recommendation for the use of topical rapamycin in the treatment of angiokeratoma. Our case provides new clinical evidence for the efficacy of topical rapamycin in treating vascular components of angiokeratoma in children [Table 1]2–5.
| No: | Author/Year | Age in years/Sex | Dermatologic manifestation/diagnosis | Previous treatment | Treatment | Clinical outcome |
|---|---|---|---|---|---|---|
| 1 | Gines F/20182 | 5/Male | Facial angiokeratoma | NA† | Topical rapamycin 0.4% once daily | After starting rapamycin significant improvement in the malar and infraorbital lesions |
| 2 | Park S/20203 | 12/Female | Multiple well-defined, erythematous to pink, hyperkeratotic, scaly papules in a linear to serpiginous pattern. The clinical and pathological findings were suggestive of APACHE.† | NA | Topical rapamycin 0.35% once daily for 5 months. | Five months after starting rapamycin, significant improvement of the lesions (flattening of some lesions, with no new lesions) |
| 3 | Park S/20203 | 3/Female | Multiple erythematous, blanchable, flat-topped, scaly papules coalescing into a plaque. The clinical and pathological findings were suggestive of APACHE. | No response to treatment with Betamethasone valerate 0.1%, and fluocinonide 0.05% | Topical rapamycin 0.2% once daily for three months, which was then increased to twice daily for five months | Five months after starting rapamycin, significant improvement of the lesions (no new lesions, reduced confluence and background erythema on dermoscopy, and flattening of prior lesions) |
| 4 | Camacho I/20204 | 18/Female | Solitary circumscribed erythematous-purplish plaque. The clinical and dermoscopy findings were suggestive of angiokeratoma. | NA | Topical sirolimus (rapamycin) 1% twice daily for four months. | Four months after starting rapamycin, significant improvement in the thickness of the lesions (lesions became flatter, slightly smaller, and lighter in color) |
| 5 | Katheryn A/20215 | 61/Male | Numerous tender lesions. The clinical and pathological findings were suggestive of angiokeratoma. | Mild response to pulsed dye laser (PDL) | Topical rapamycin (1 mg tablets compounded into a 0.25% cream) twice daily for three months. | Three months after starting rapamycin resolution of pain and tenderness . Sustained improvement in the size and number of scrotal angiokeratoma after seven months. |
| 6 | Present case | 5/Female | Well-circumscribed plaque studded with multiple erythematous to purplish verrucous papules at the proximal part of the thigh. The clinical findings were suggestive of angiokeratoma | Pulsed Dye Laser complicated with severe bleeding | Topical 0.04% rapamycin twice daily for three months. | Three months after starting rapamycin, significant improvement of the lesions (the vascular component of the lesion was cleared and the color of the lesion changed to light-yellow) |
†NA = not available
The limitation in the present case is lack of histological confirmation and a short follow up of six months. Further studies on the efficacy and safety of topical rapamycin in the treatment of cutaneous vascular lesions may establish rapamycin as an effective treatment for vascular proliferative disorders.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Efficacy and absorption of topical sirolimus for the treatment of vascular anomalies in children: A case series. Pediatr Dermatol. 2018;35:472-477.
- [CrossRef] [PubMed] [Google Scholar]
- 4CPS-143 Topical application of rapamycin 0.4% for treatment of facial angiokeratomas in a paediatric patient. European Journal of Hospital Pharmacy. 2018;25:A10-A.
- [Google Scholar]
- Use of topical rapamycin in acral pseudolymphomatous angiokeratoma of children (APACHE): A report of two cases and review of the literature. Pediatr Dermatol.. 2020;37:877-80.
- [CrossRef] [PubMed] [Google Scholar]
- Topical sirolimus for treatment of a solitary angiokeratoma. Dermatol Ther. 2020;33:e13907.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of angiokeratomas of Fordyce with topical rapamycin 0.25% cream. JAAD Case Rep. 2021;8:50-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






