Translate this page into:
Darier disease responding to apremilast: Report of two cases
Corresponding author: Dr. Aikaterini Tsiogka, Department of Dermatology-Venereology, National and Kapodistrian University of Athens, Faculty of Medicine, Andreas Sygros Hospital, Athens, Greece. a.tsiogka@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Kleidona IA, Agiasofitou E, Tsiogka A, Chorti M, Gregoriou S, Stratigos A et al. Darier disease responding to apremilast: Report of two cases. Indian J Dermatol Venereol Leprol. 2024;90:240–3. doi: 10.25259/IJDVL_83_2023
Dear Editor,
Darier disease is an autosomal dominant genodermatosis with variable expression, characterised by a chronic course with exacerbations and remissions. Causative mutations have been identified in the gene ATP2A2, which encodes SERCA (SarcoEndoplasmic Reticulum Ca2+-ATPase 2), a calcium-ATPase pump, resulting in reduced concentrations of calcium in the endoplasmic reticulum.1 There is currently no cure for the disease and there is lack of efficacious treatments for the long term remission. Proposed treatment approaches include systemic and topical retinoids, immunomodulators, magnesium, penicillamine, antibiotics, doxycycline, dermabrasion, lasers, photodynamic therapy, radiotherapy, and surgical therapy. However, strong evidence is lacking.2 As the pathophysiology of the disease becomes better understood, alternative and safer agents may be tried. Herein, we present two patients with Darier disease who responded well to apremilast.
A 63-year-old woman presented with brownish-erythematous keratotic papules coalescing into crusted, greasy malodorous pruritic plaques over the neck, chest, inframammary area, abdomen, and waist. The fingernails showed ridging, longitudinal red bands and V-shaped distal splitting [Figures 1a–1c]. The patient reported a chronic course over 35 years with frequent flares leading to a significant impact on her quality of life. Histopathology revealed hyperkeratosis, acantholysis, and dyskeratotic cells with “corps ronds” in the stratum spinosum and “grains” in the stratum corneum, confirming the diagnosis of Darier disease [Figure 2]. She had received treatment with topical corticosteroids, topical calcineurin inhibitors, oral acitretin, oral isotretinoin and botulinum toxin injections to the inframammary area in the past with poor response. Due to the severity of her condition at the time of presentation and the exhaustion of existing treatment options, we decided to initiate apremilast 30 mg twice daily in addition to acitretin 10 mg on alternate days, topical methylprednisolone on skin lesions, and topical clobetasol propionate on the periungual lesions. She showed significant clinical improvement of the skin lesions and pruritus within a month and acitretin was subsequently discontinued three months after initiation of apremilast. Baseline and follow-up laboratory investigations revealed only mild anaemia which improved with iron supplementation. The patient is currently one year into therapy with apremilast and topical corticosteroids, and reports significant clearance of skin lesions and improvement of nail changes with occasional minor flare-ups but no side effects [Figures 3a–3c].
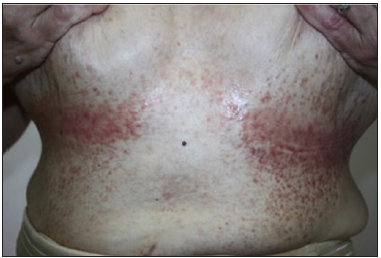
- Inframammary area showing keratotic papules with erosions.

- Chest and neck area at presentation.

- Nail changes at presentation; longitudinal red bands, ridging and dystrophic nail plate.

- Histopathological image showing dyskeratotic cells with “corps ronds” in the stratum spinosum and “grains” in the stratum corneum. (Hematoxylin–eosin staining, x400)

- Resolution of inframammary lesions after 12-month treatment with apremilast.

- Chest and neck area 12 months after apremilast initiation.

- Improvement of nail signs 12 months after apremilast initiation.
The second case was a 21-year-old man who presented with a 10-year history of red to brown hyperkeratotic papules in a seborrheic distribution involving the neck, shoulders, chest, and back [Figure 4a]. He reported frequent exacerbations and had severe pruritus, especially during the summer months. The diagnosis of Darier disease was confirmed in the past. He had been treated with topical corticosteroids, topical calcineurin inhibitors, isotretinoin, acitretin, and topical glycopyrrolate with only limited response. Therefore, we decided to initiate apremilast 30 mg twice daily while continuing acitretin 10 mg daily, along with topical methylprednisolone. The patient had significant improvement starting at 4 weeks of therapy which was sustained at 9 month follow up. Specifically, the inflammatory component and pruritus improved the most [Figure 4b]. No side effects were observed.

- Red-brown hyperkeratotic papules on the shoulders and back, at presentation.

- Improvement in lesions 7-months after the initiation of apremilast.
Apremilast is a phosphodiesterase 4 (PDE4) inhibitor approved by the US Food and Drug Administration (FDA) for treating plaque psoriasis, psoriatic arthritis, and Behçet’s disease. It elevates cyclic adenosine monophosphate (cAMP), which in turn downregulates proinflammatory and increases anti-inflammatory cytokines.3 Of note, PDE4 is predominant in controlling inflammatory cells but is also present in structural cells such as keratinocytes. Interestingly, both Ca2+ and cAMP are essential intracellular second messengers. An intriguing interplay mechanism between these two messengers’ signalling pathways might play a role in physiological processes and disease.
In the context of Darier disease, we postulate that apremilast may have a role in controlling inflammation and potentially regulating calcium homeostasis via interaction with cAMP.4 Herein, we report satisfactory response to apremilast in two patients with varied severity of Darier disease. Given the favourable safety profile of apremilast, treatment duration in these patients may be guided by its ability to control symptoms. To our knowledge, there are no prior reports of Darier disease managed with apremilast. However, there are some cases of refractory Hailey-Hailey treated with apremilast with variable responses.5 Although promising, further studies with longer follow-ups are required to confirm the efficacy of apremilast in these conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Darier’s disease: Epidemiology, pathophysiology, and management. Am J Clin Dermatol. 2003;4:97-105.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Darier disease: A review of the literature and update. Indian J Dermatol Venereol Leprol. 2021;87:14-21.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term or long-term treatments with a phosphodiesterase-4 (PDE4) inhibitor result in opposing agonist induced Ca(2+) responses in endothelial cells. Br J Pharmacol. 2008;154:82-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The PDE4 inhibitor CHF6001 affects keratinocyte proliferation via cellular redox pathways. Arch Biochem Biophys. 2020;685:108355.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of Hailey-Hailey disease effectively treated with apremilast and a review of reported cases. J Dermatol. 2021;48:1945-8.
- [CrossRef] [PubMed] [Google Scholar]





