Translate this page into:
Lipodystrophia centrifugalis abdominals infantilis presenting as a giant ulceration and treatment with hydroxychloroquine and baricitinib
Corresponding author: Dr. Zigang Xu, Department of Dermatology, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Xicheng, Beijing, China. zigangxupek@163.com
-
Received: ,
Accepted: ,
How to cite this article: Zhao X, Miao C, Chen Y, Xiang X, Liu Y, Zhaoyang W, et al. Lipodystrophia centrifugalis abdominals infantilis presenting as a giant ulceration and treatment with hydroxychloroquine and baricitinib. Indian J Dermatol Venereol Leprol. 2024;90:703. doi: 10.25259/IJDVL_643_2023
Dear Editor,
Lipodystrophia centrifugalis abdominalis infantilis (LCAI) is a localised lipodystrophic disease mainly affecting young children. It’s characterised by a depression of the skin resulting from the loss of subcutaneous fat with an erythematous border involving the lower abdomen and the groin region, neck, or axilla.1 Ulceration can occur sometimes, although it is uncommon.2 Here, we describe a case of LCAI with a giant ulceration which was successfully treated with hydroxychloroquine (HCQ) and baricitinib.
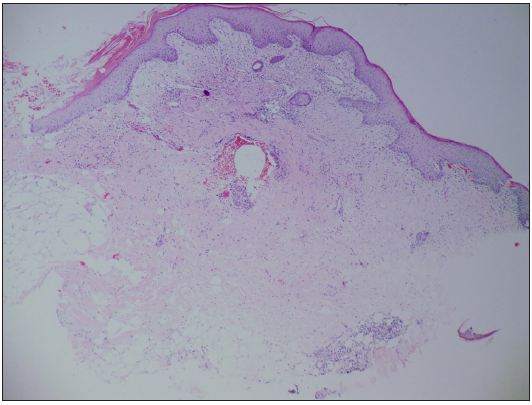
A 4-year-old boy presented with recurrent ulceration on his lower abdomen for 1.5 years. Scattered erythema initially appeared on the right lower abdomen when he was 2.5 years old. Then, the lesions gradually extended to the neighbouring region and a giant ulceration developed within it [Figure 1]. The patient had no pain and denied any systemic symptoms, including fever, fatigue, or weight loss. No abnormality was found in the systemic physical examination. Laboratory tests revealed that blood routine, liver function test, and kidney function tests were all within normal reference range. Tests for infective disease were negative, including next-generation sequencing (NGS) of microorganisms in skin lesions. Serology revealed that antinuclear antibody (ANA) and anti-dsDNA antibodies were negative.

- Giant ulceration with thick crust on the abdomen and inguinal region surrounded with infiltrated erythema.
The patient failed to respond to the treatment of antimicrobials and antifungal agents. A biopsy from the erythematous area was performed that showed small amounts of adipocytes with an inflammatory infiltrate of lymphocytes, histiocytes, and a few plasmacytes [Figures 2a and 2b]. LCAI was diagnosed. He was treated with Hydroxychloroquine (HCQ) at a dosage of 5.5 mg/(kg.d). After 4 months, the lesion had a significant improvement with rapid healing of the ulcer and necrotic crusts falling off. However, there was still an erythematous change at the border occasionally [Figure 3a]. Baricitinib was started at a dosage of 1 mg/day after obtaining informed consent from his parents. The erythema disappeared and the ulceration completely healed over 5 months of treatment with baricitinib combined with HCQ with only a residual scar [Figure 3b]. The total course of treatment for hydroxychloroquine was 14 months and for baricitinib, it was 10 months. After discontinuation of the two drugs for 6 months, the lesion didn’t reoccur [Figure 3c]. The patient is still under follow-up.
- Acute and chronic inflammatory cells were visible around the ulceration (Haematoxylin & Eosin, 50x).
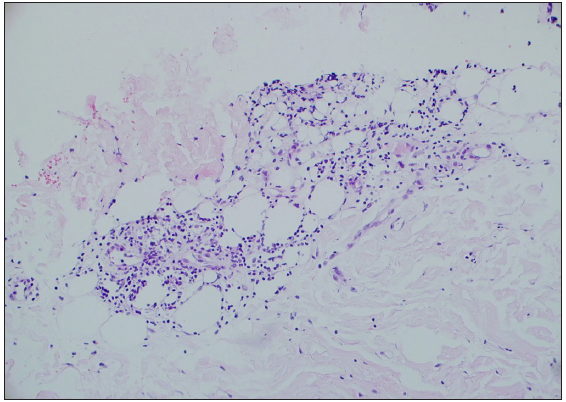
- Subcutaneous fat necrosis with an infiltrate of lymphocytes, histiocytes, and a few plasmacytes (Haematoxylin & Eosin, 200x). Lipodystrophia centrifugalis abdominals infantilis presenting as a giant ulceration and treatment with hydroxychloroquine and baricitinib

- Ulcer rapidly healing and necrotic crusts falling off after the treatment of HCQ for 4 months. But there still had an erythematous change at the border occasionally.
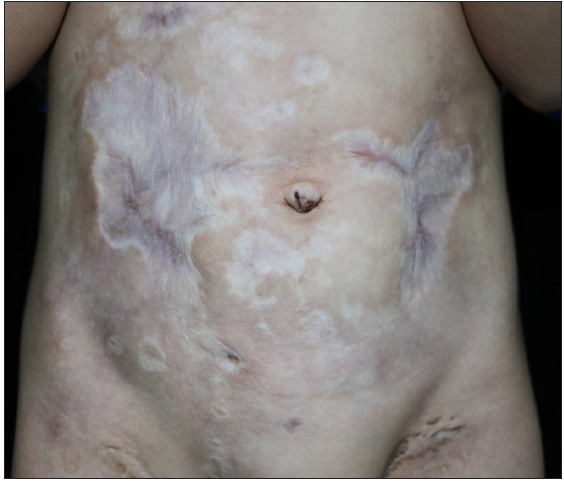
- After the treatment of baricitinib combined with HCQ for 5 months.

- After discontinuation of the two drugs for 6 months.
Ulceration is a rare skin manifestation of LCAI and only four patients have been reported to present with it,3 but such a large one has never been reported. We had considered the other diseases that can present such an ulcer [Table 1], but none of them were consistent with the condition of this patient. The etiopathogenesis of LCAI remains unknown and several probable causes have been proposed, including trauma, infection, metabolic or genetic abnormalities, apoptosis, and immunological dysfunctions.1 The principal mechanism underlying ulcer formation may be the vasculitis of the lobular vessels resulting from subcutaneous inflammation. We decided to treat with HCQ because the pathological feature of the disease was predominantly lobular panniculitis which resembled the pattern in lupus erythematosus panniculitis. The result showed it can also be a good choice for the inflammation of LCAI. Besides, baricitinib also showed an inspiring efficacy. The Janus kinase (JAK) inhibitors target and block cytokine signalling mediated by the JAK-signal transducer and activator of transcription (JAK-STAT) pathway, thereby regulating immune response and cell growth and are effective in various skin disorders such as psoriasis, atopic dermatitis, alopecia areata, and lupus erythematosus.4 The JAK1 and JAK2 inhibitor baricitinib was reported to be effective in patients with DM-associated panniculitis.5 We tried to use baricitinib on our patient and it turned out to be effective. To conclude, severe ulceration is rare in LCAI and our case indicated that HCQ combined with baricitinib might be a good approach in such giant ulcerations of LCAI.
| Disease | Differentiating features |
|---|---|
| infectious granuloma | Pathogens can be detected by culture or PCR; histopathology shows granulomatous inflammation |
| vasculitis | Histopathology shows vessel wall and peri-vascular infiltrated by inflammatory cells and vessel wall necrosis |
| lymphoma | Histopathology shows a predominantly lobular infiltrate predominantly composed of lymphocytes with atypia |
PCR: Polymerase chain reaction
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This study was supported by the Beijing Natural Science Foundation (7212037).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Lipodystrophia centrifugalis abdominalis infantilis: Statistical analysis of 168 cases. Pediatr Dermatol. 2012;29:437-41.
- [CrossRef] [PubMed] [Google Scholar]
- Lipodystrophia centrifugalis abdominalis infantilis with ulceration. Dermatol. 2000;200:280-1.
- [Google Scholar]
- Lipodystrophia centrifugalis abdominalis infantilis manifesting as recurrent skin ulcerations. Int J Dermatol. 2009;48:1113-5.
- [CrossRef] [PubMed] [Google Scholar]
- Emerging topical and systemic JAK inhibitors in dermatology. Front Immunol. 2019;10:2847.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improvement of cutaneous inflammation and panniculitis in patients with dermatomyositis by the Janus kinase inhibitor baricitinib. Br J Dermatol. 2022;187:432-5.
- [Google Scholar]





