Translate this page into:
Management of leukocytosis in erythroderma
Corresponding author: Dr. Meghashree G, Department of Dermatology, Kanachur Institute of Medical Sciences, Deralakatte, Mangaluru, India. megha91leo@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Surve RR, Shenoi SD, Meghashree G, Varsha GVM, Zoya A. Management of leukocytosis in erythroderma. Indian J Dermatol Venereol Leprol. 2025;91:S41-S42. doi: 10.25259/IJDVL_567_2023
Dear Editor,
Erythroderma or exfoliative dermatitis is diffuse inflammation causing redness and scaling of more than 90% of body surface area secondary to preexisting dermatoses, drugs, malignancies, etc.1 Erythrodermic patients often present with leukocytosis and fever. Due to defective barrier function, patients are prone to getting infections. Hence, it is important to differentiate patients of erythroderma with infections from those without.
We report a 60-year-old man, who presented with an erythroderma of six months’ duration. The patient also complained of intermittent low-grade fever, not associated with chills for five days. There was a history of recurrent itchy vesicular lesions over palms associated with exposure to carrom powder. These occurred every one or two years for the last 15 years. These lesions used to subside on applying topical medications and were suggestive of irritant contact dermatitis. On examination, there was generalised erythema and scaling with sparing of the nose and lichenification over the lower limbs. Bilateral palms and soles showed keratoderma with deep fissures. Histopathology showed features suggestive of dermatitis. Haematological investigations showed leukocytosis and anaemia with a white blood cell count of 16,890 cells/mm3 and haemoglobin of 11.10 g/dl. Peripheral smear showed normocytic hypochromic anaemia with eosinophilia with an absolute eosinophil count of 3800 cells/mm3. Total differential count was: neutrophils 45%, lymphocytes 31%, eosinophils 20% and monocytes 4%. A diagnosis of erythroderma secondary to eczema was made. Body temperature was 99°F. Patient was treated with antihistamines along with topical steroid creams and emollients. After a day of fever free interval, an intramuscular injection of triamcinolone acetonide 40 mg was given to reduce the inflammation and initial control of the disease. On the next day, white blood cell count increased to 18,820 cells/mm3 with a differential count of neutrophils 58.4%, lymphocytes 22.4%, eosinophils 5.3%, monocytes 13.5%, and basophils 0.4%. The patient remained afebrile and the chest X-ray was normal. The patient was detected with diabetes on routine work-up. Hence to substitute steroids, cyclosporine was considered and a physician’s opinion was sought. Given leukocytosis, sepsis work-up was advised but due to financial constraints, it was withheld. The physician advised to start cyclosporine under the cover of oral antibiotics, hence empirical antibiotic therapy was given considering the risk-benefit ratio. The patient improved over two months with cyclosporine and no other side effects were noted.
In erythroderma, apart from scaling, erythema and pruritus, there can be malaise and fever. Chronic inflammation may lead to mild anaemia, leukocytosis, and eosinophilia.2 Erythrocyte sedimentation rate and serum Immunoglobulin E may be raised in patients with pre-existing chronic inflammatory dermatosis. Fever and leukocytosis often prompt one to start prophylactic antibiotics and sometimes even broad-spectrum antibiotics like piperacillin-tazobactam. However, due to the increasing incidence of antibiotic resistance and the high cost, we have to be cautious while prescribing them in patients of erythroderma.
An erythrodermic patient with leukocytosis (<30,000 cells/mm3) should be thoroughly screened for infection by various tests including chest X-ray, serum procalcitonin levels, blood culture, urine culture, and sputum culture. If positive, a suitable antibiotic should be started [Figure 1]. Peripheral smear is an indispensable test where toxic granules and shift to the left in neutrophils will be noted in infections and atypical cells will be seen in myeloproliferative diseases. However, physiological variations should always be ruled out, in special situations such as in newborns or pregnant patients, chronic smokers, patients who have undergone splenectomy, or patients on certain drugs like steroids.3,4 Patients on steroids can develop leukocytosis with increased polymorphonuclear cell levels, increased monocytes, and decreased eosinophils. Leukocytosis induced by steroids will not show a shift to the left or toxic granules as seen with infection.5,6 For an erythrodermic patient with leukocytosis of >30,000 cells/mm3, a history regarding weight loss, anorexia, and bleeding with a thorough evaluation for leukaemia or cutaneous T cell lymphoma is mandatory.3,6 Ultrasonography is done to check for organomegaly. Peripheral smear will aid in diagnosing Sezary syndrome and myeloproliferative disease, showing Sezary cells and blast cells, respectively. [Figure 1]. Sezary cells have characteristic convoluted to cerebriform nuclei with mildly condensed chromatin and inconspicuous nucleoli with more than 1000/mm3 cells noted in peripheral smear. CD4+ lymphocytosis with increased CD4:CD8 ratio >10:1 is also noted.
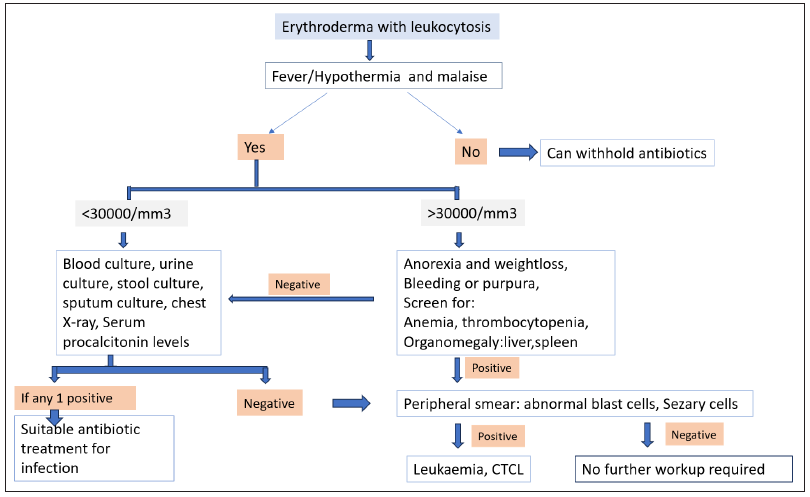
- Evaluation of erythrodermic patients with leukocytosis. (CTCL: Cutaneous T-Cell lymphoma)
Hence, in the case of erythroderma with low-grade fever and leukocytosis, empiric antibiotics should be discouraged. Antibiotics should be started only if there is definite evidence of infection based on the clinical and laboratory findings. There has been no focus in dermatology literature about the management of erythroderma patients presenting with fever and leukocytosis, hence we wanted to highlight the same. We suggest the following flowchart for the management of leukocytosis in an erythrodermic patient. However, this needs to be validated by further studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Erythroderma – A clinico-etiologic study of 90 patients. Int J Dermatol. 1998;37:104-7.
- [CrossRef] [PubMed] [Google Scholar]
- Leukocytosis: Basics of clinical assessment. Am Fam Physician. 2000;62:2053-60.
- [PubMed] [Google Scholar]
- Hematology: Basic principles and practice (6th ed). Philadelphia, Pa.: Elsevier/Saunders; 2013. p. :164-20.
- Prednisone-induced leukocytosis. Influence of dosage, method and duration of administration on the degree of leukocytosis. Am J Med. 1981;71:773-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of patients with leukocytosis. Am Fam Physician. 2015;92:1004-11.
- [PubMed] [Google Scholar]





