Translate this page into:
Focal actinic porokeratosis over nose successfully treated with topical tacrolimus
Corresponding author: Dr. Suman Patra, Department of Dermatology, AIIMS, Jodhpur, Rajasthan, India. patrohere@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar S, Patra S, Nalwa A. Focal actinic porokeratosis over nose successfully treated with topical tacrolimus. Indian J Dermatol Venereol Leprol. 2024;90:666-8. doi: 10.25259/IJDVL_880_2023
Dear Editor,
Porokeratosis is an uncommon clonal disorder of keratinisation. Classically, five clinical variants have been described: porokeratosis of Mibelli, disseminated superficial porokeratosis, disseminated superficial actinic porokeratosis (DSAP), porokeratosis palmaris et plantaris disseminata and linear porokeratosis. Medical modalities have varying success rates and surgical or ablative options are usually chosen for solitary lesions.1 We hereby report a case of facial porokeratosis with a good response to topical tacrolimus ointment 0.1%.
A 22-year-old male presented with a few asymptomatic and erythematous crusted plaques over the nose for a 6-month duration. In addition, he had iron deficiency anaemia (Hb: 6.5 g/dl) and a history of weight loss of 8 kg in the last 6 months. Four well-defined, skin coloured to erythematous annular plaques of size ranging from 1 × 1 cm to 1.5 × 2 cm with an atrophic depigmented centre, follicular plugging, and prominently raised margins with yellowish heaped-up crust over the superior margins were present bilaterally over the ala of the nose [Figures 1a and 1b]. Dermoscopy showed red dots, follicular plugging, whitish structureless areas, and a prominent raised margin [Figure 1c]. Histopathology of the lesion revealed epidermal invagination with a parakeratotic column (cornoid lamella) and underlying hypogranulosis with moderate superficial dermal inflammatory infiltrate (lymphocytic and neutrophilic) suggestive of porokeratosis [Figures 2a and 2b]. He was treated earlier with moderately potent topical corticosteroids and topical retinoids for two months with not much response. As we wanted to avoid destructive modalities owing to the risk of cosmetic disfigurement, the patient was started on topical tacrolimus ointment of 0.1% twice daily. After 8 weeks of treatment, the patient showed a good response with significant flattening of the plaques [Figure 3]. The patient is currently off treatment since 1 year with no recurrence.
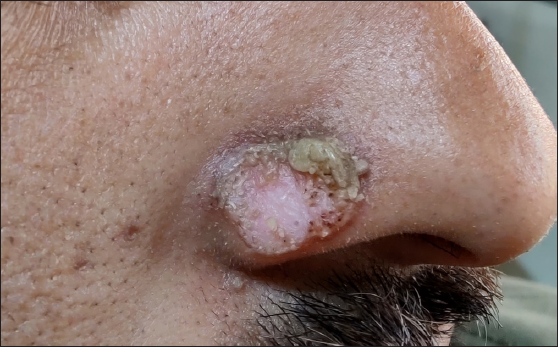
- Erythematous annular plaque with central atrophy with raised borders over the right ala.

- Three well-defined erythematous annular keratotic plaques with central atrophy and raised borders and thick yellowish heaped-up crust over the left ala.
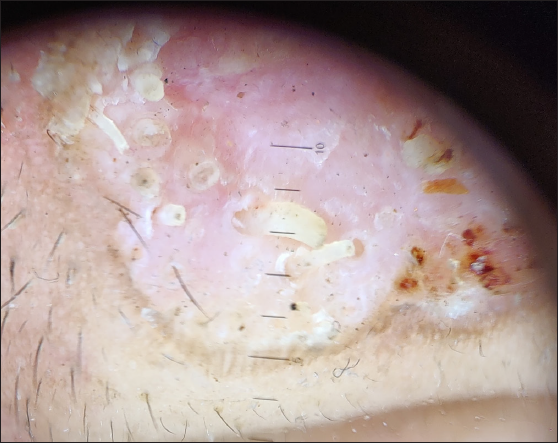
- Dermoscopy of the lesions highlighted the prominent ridge at the margin of the lesions (Heine Delta 20T, 10×).
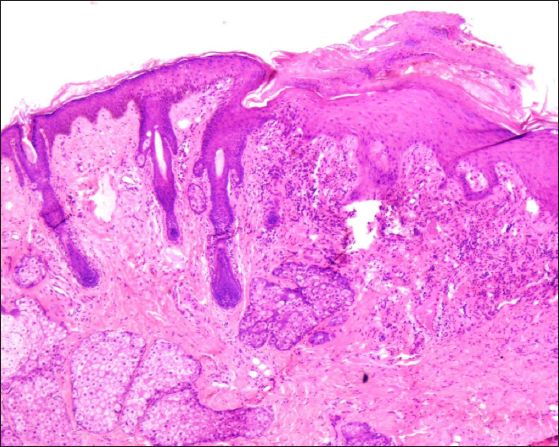
- Epidermal invagination of a parakeratotic column with underlying hypogranulosis (Haematoxylin and Eosin, 40x).
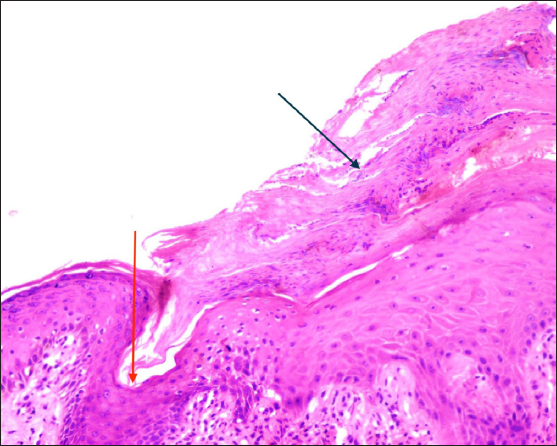
- Higher magnification showing epidermal invagination at an acute angle (red arrow) of a parakeratotic column (black arrow) with underlying hypogranulosis (Haematoxylin and Eosin, 100x).

- Significant improvement of the lesion with topical tacrolimus at 8 weeks.
Porokeratosis refers to a heterogeneous group of disorders but it retains the morphology of annular plaques across the spectrum. The extremities, trunk, and sometimes the flexors are the common sites. Facial lesions are seen concomitantly in a small percentage of DSAP patients but isolated facial porokeratosis is rare.2 It is considered as a distinct subset of porokeratosis of Mibelli related to actinic damage and is most commonly distributed over the nose and the perinasal region. Hence, it is known by other names, such as solar facial porokeratosis, localised actinic nasal porokeratosis, and localised actinic facial porokeratosis.3 The lesions are difficult to treat. The choice of treatment depends on the number, site, and size of the lesions. Ablative or surgical modalities like laser ablation, cryotherapy, dermabrasion, surgical excision, photodynamic therapy, and electrodessication are the preferred treatments of choice for solitary or localised lesions. For disseminated lesions, medical modalities, systemic retinoids, and phototherapy have been tried.1 For a localised bur large-sized lesion or lesion located at an unresectable site, various topical modalities including 5 fluorouracil, corticosteroids, retinoids, keratolytic agents, vitamin D3 analogues, 5% imiquimod, and 3% diclofenac sodium, have been tried with varying success rates.1 Facial porokeratosis is unique for its location. There is not much mention in the literature regarding the management options of facial lesions in particular. Lee et al.4 claimed mild improvement in one patient after 2 months of topical 1% pimecrolius ointment applied twice daily. Miranda et al.5 claimed slight improvement in large lesions and complete clearance in small lesions after cryotherapy in one patient. Gutierrez et al.6 used isotretinoin 20 mg once daily and topical tretinoin and salicylic acid in three patients each and claimed mild improvement in only two out of six patients. Topical and systemic retinoids are the usual modalities used with variable response. Patients must also be counselled regarding photoprotection and long-term follow-up. Tacrolimus has been used in one isolated case of porokeratosis with success.3 The mechanism of action is not clear. A low concentration of pimecrolimus has been described to enhance innate immune response.7 This might be responsible for inhibitory response to the abnormal keratinocytes. We wanted to choose a therapy with less irritant potential, considering the tolerability of the facial location. Our patient responded remarkably well to therapy with tacrolimus 0.1% ointment. Though the possibility of spontaneous resolution cannot be completely excluded, this is unlikely to happen in porokeratosis. This report highlights tacrolimus as an effective treatment option.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Treatment of porokeratosis: A systematic review. Am J Clin Dermatol. 2017;18:435-49.
- [CrossRef] [PubMed] [Google Scholar]
- Facial solar porokeratosis. Indian J Dermatol Venereol Leprol. 2016;82:337-9.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term clearance of linear porokeratosis with tacrolimus, 0.1%, ointment. JAMA Dermatol. 2014;150:194-6.
- [CrossRef] [PubMed] [Google Scholar]
- Exclusive facial porokeratosis: Histopathologically showing follicular cornoi lamellae. J Dermatol. 2011;38:1072-5.
- [CrossRef] [PubMed] [Google Scholar]
- Facial porokeratosis characterized by destructive lesions. Int J Dermatol. 2004;43:913-4.
- [CrossRef] [PubMed] [Google Scholar]
- Facial porokeratosis: A series of six patients. Aust J Dermatol. 2010;51:191-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pimecrolimus enhances TLR2/6-induced expression of antimicrobial peptides in keratinocytes. J Invest Dermatol. 2008;128:2646-54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






