Atypical ulcerative cutaneous tuberculosis in a zosteriform distribution due to Mycobacterium bovis
Corresponding author: Sujay Khandpur, Department of Dermatology and Venereology, AIIMS, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma A, Sathyan A, Ramesh V, Kumari L, Ahmed J, Bala K, et al. Atypical ulcerative cutaneous tuberculosis in a zosteriform distribution due to Mycobacterium bovis. Indian J Dermatol Venereol Leprol. 2024;90:420. doi: 10.25259/IJDVL_370_2023
Dear Editor,
A 55-year-old man presented with a 6-month history of recurrent painful vesicular eruption over the left perigenital region that developed into a large, persistent, severely tender, 15 × 15 cm, well-defined, indurated, erythematous plaque involving the left inguinal area. Stellate erosions were seen on the glans penis on the same side. There were polycyclic erosions with yellowish slough overlying the plaque, as well as areas of atrophy and scarring [Figure 1a]. Tzanck smear showed acantholytic cells and multinucleated giant cells. Polymerase chain reaction (PCR) was positive for herpes simplex virus 2. The patient was diagnosed with herpes simplex in a zosteriform distribution and treated with intravenous acyclovir. However, there was minimal improvement and ulceration progressed to involve the entire plaque [Figure 1b]. Skin biopsy for histopathology showed a mixed cell granulomatous tissue reaction with many Langhans and foreign body–type giant cells [Figure 2a]. Ziehl-Neelsen staining of the tissue biopsy showed clumps of acid-fast bacilli [Figure 2b]. GeneXpert MTB/Rif as well as liquid culture (MGIT 960), confirmed the acid fast bacilli as a rifampicin-sensitive Mycobacterium tuberculosis complex. Due to atypical clinical presentation, further speciation was performed on tissue samples by PCR, which identified the organism as Mycobacterium bovis (M.bovis).

- Well-defined, ulcerated, erythematous plaque involving the left inguinal region with polycyclic erosions.

- Progression of ulceration to involve the entire plaque.
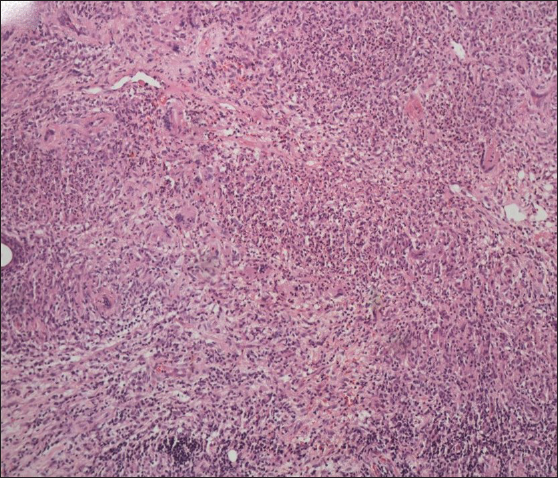
- Skin biopsy showing mixed cell granulomatous tissue reaction with multiple giant cells (Haematoxylin & Eosin, 100x).
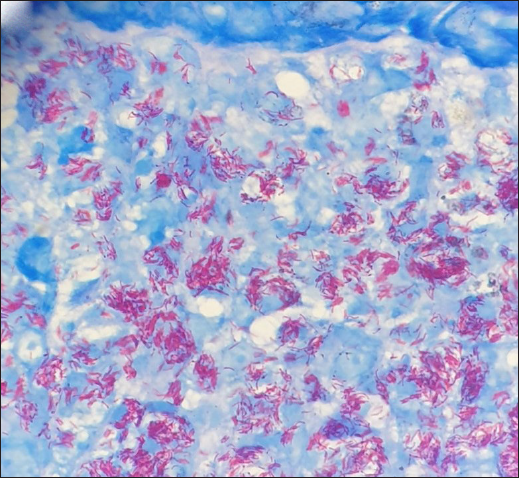
- Ziehl-Neelsen stain showing acid-fast bacilli in clusters (Ziehl-Neelsen, 1000x).
The patient gave no personal or family history of tuberculosis. There was no history of fever, loss of appetite or weight, chronic cough, traumatic inoculation, open defecation, or contact with cattle. Mantoux test was negative and a contrast-enhanced (CT) scan of the chest, abdomen and pelvis, and colonoscopy showed no abnormality. There was no history suggestive of immunosuppression. Serum ELISA for HIV was non-reactive on two occasions, six weeks apart. A primary immunodeficiency workup revealed normal immunoglobulin levels, a high CD4:CD8 ratio of 11.45 (normal: 0.6–2.4), and a low absolute CD4 count of 224 cells/cu mm (normal range: 500–1500 cells/cu mm). Neutrophil oxidative index was within normal limits. Work-up for Mendelian susceptibility for mycobacterial diseases (CD14+IFNϒR1+ levels) did not reveal any abnormalities.
Due to intrinsic resistance of M. bovis to pyrazinamide, the patient was started on isoniazid, rifampicin and ethambutol (HRE regimen of antitubercular therapy) with onset of improvement within a week and complete healing of the ulcers in six weeks [Figure 3]. Repeat CD4 and CD8 counts after one month of treatment were normal with a normal ratio.

- Complete resolution of inguinal plaque with depigmentation and scarring after 6 weeks of anti-tuberculous therapy.
Cutaneous tuberculosis occurs as a result of chronic infection by Mycobacterium tuberculosis (M.tb), M. bovis, or occasionally by the Calmette-Guerin bacillus, all of which are part of the Mycobacterium tuberculosis complex. Perianal tuberculosis may present as an abscess, fistula or ulceration and is often (57.6% cases) associated with active pulmonary tuberculosis, though 20.8% of cases may have no history or evidence of pulmonary involvement.1 Auto-inoculation from intestinal or genito-urinary tuberculosis, or exogenous inoculation may also occur. However, the ulcer in our patient did not extend to the anal orifice and there was no evidence of systemic tuberculosis or history suggestive of possible exogenous inoculation.
The primary lesion in our patient was full of acid-fast bacilli and the patient did not mount a response to the tuberculin test despite being immunocompetent. The transient decrease in CD4 count could be due to known secondary immune suppression by mycobacteria.2 The organism isolated was M. bovis which is known to be the causative agent in up to 12.6% of cases of pulmonary tuberculosis and has been reported as a cause of extra-pulmonary tuberculosis indistinguishable from M.tb.3,4 The maximum proportion of tuberculosis cases caused by M. bovis is seen in high TB-endemic areas rather than groups of farmers, dairy workers, or animal handlers.3 In a survey of 1241 cases of non-pulmonary tuberculosis from England and Wales, M.bovis infection manifested as lupus vulgaris in 15.4% and scrofuloderma in another 4.8%.4 A literature search revealed two case reports of infiltrated, well-defined scaly plaques due to M. bovis with one involving the medial thigh5,6 as in our case, but without ulceration. The recurrent vesicular lesions are most likely explained by an eczema herpeticum–like secondary infection of cutaneous tuberculosis.
This atypical case of the ulcerative form of cutaneous tuberculosis due to M.bovis in a unilateral distribution in an immunocompetent patient highlights that tuberculosis remains a great masquerader.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Perianal tuberculosis: A case report and review of the literature. World J Clin Cases. 2015;3:848-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Targeting Mycobacterium tuberculosis tumor necrosis factor alpha-downregulating genes for the development of antituberculous vaccines. mBio. 2016;7:e01023-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of zoonotic tuberculosis and associated risk factors in Central Indian populations. J Epidemiol Glob Health. 2017;7:277-83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mycobacterium bovis infection in human beings. Tuberculosis. 2001;81:71-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous tuberculosis due to Mycobacterium bovis lasting for more than 60 years. Clinical and Experimental Dermatology. 2019;34:921-92.
- [CrossRef] [PubMed] [Google Scholar]
- Long-lasting cutaneous tuberculosis owing to Mycobacterium bovis masquerading as sarcoidosis. JAAD Case Rep. 2018;5:1-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






