Translate this page into:
Vitiligo-like basal cell carcinoma: An emerging entity in young women
Corresponding author: Dr. Vicente García-Patos, Department of Dermatology, Hospital Universitari Vall d’Hebron, Barcelona, Spain. vicente.garciapatos@vallhebron.cat
-
Received: ,
Accepted: ,
How to cite this article: Gómez-Tomás A, Falguera-Mayoral M, García-Patos V, Bassas-Freixas P, Palao-Doménech R, Ferrer-Fábrega B, et al. Vitiligo-like basal cell carcinoma: An emerging entity in young women. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_672_2023
Dear Editor,
Recently, a case of basal cell carcinoma (BCC) in a young woman, 23 years old, that was initially misdiagnosed as a facial vitiligo has been reported.1 We present a similar case to further emphasise the importance of considering BCC as a possibility when evaluating solitary hypopigmented lesions resembling vitiligo in young patients.
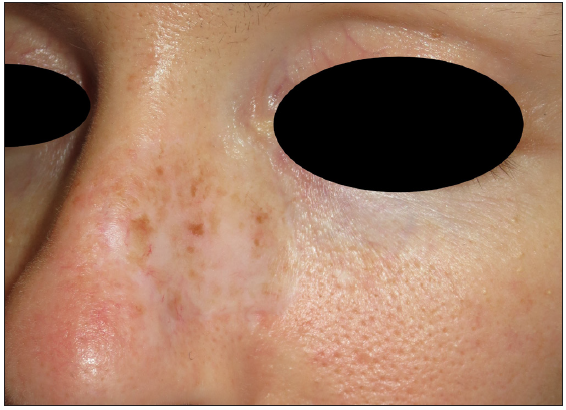
A 28-year-old woman with no other health concerns sought advice from multiple dermatologists over the past 3 years for a slowly expanding asymptomatic, hypopigmented patch, measuring 9 × 3 cm on the left side of her face, covering the left cheek and left side of the nose [Figure 1]. Physical examination revealed no additional hypopigmented or achromic lesions. The patient had no prior personal or familial history of vitiligo or other autoimmune disorders. Topical treatment for vitiligo did not result in lesion improvement. On Wood’s light examination, characteristic fluorescent findings associated with vitiligo were not observed and dermoscopic examination with Derm Lite DL200 Hybrid dermoscope revealed only a subtle effacement of follicular openings.
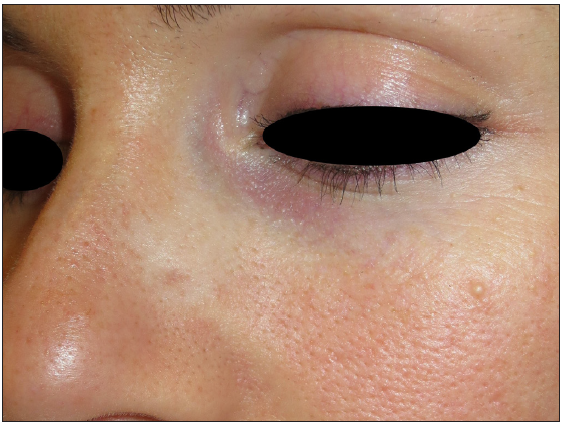
- Hypopigmented patch covering the left cheek and left side of the nose, note subtle scar due to punch biopsy.
We considered many differential diagnoses of hypopigmented lesions including pityriasis alba, naevus anemicus, naevus depigmentosus, lichen sclerosus, mycosis fungoides and tinea versicolor.2 Due to refractory behaviour and atypical presentation of the lesion, a punch biopsy was performed.
The histologic study revealed a striking neoplastic cell proliferation characterised by basal nuclei with uniform chromatin and limited cytoplasm, primarily located within the dermis, forming numerous small nodules, aligning with the diagnostic criteria for the micronodular subtype of basal cell carcinoma (BCC). These nodules extended their influence into the reticular dermis and demonstrated extensive perineural invasion [Figure 2]. Notably, a dense stromal component was identified surrounding the tumour. Within the context of the micronodular lesion, a distinct focus of infiltrative BCC was identified. The patient underwent Mohs micrographic surgery with frozen section analysis, requiring three stages to achieve clear surgical margins [Figure 3]. We encountered specific practical challenges during the surgery, such as the extent of tumour infiltration turning out to be larger than initially anticipated, and a large defect that remained after tumour removal. An autologous infraclavicular full-thickness skin graft was used to provide coverage and achieve the desired surgical outcome [Figure 4]. Given the location and perineural invasion of the tumour (54.6 µm), adjuvant treatment with iridium brachytherapy was employed (with a total dose of 60 Gy). After a three-year follow-up, the patient remained free of recurrence.
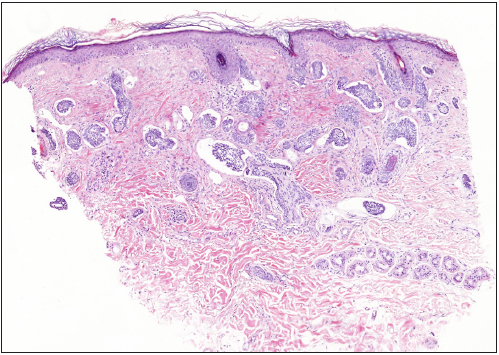
- Numerous small nodules and cords of basaloid cells infiltrating between dermal collagen bundles (Haematoxylin & Eosin; 40x).
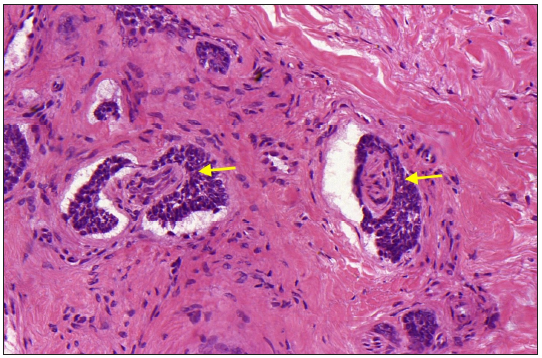
- Extensive perineural invasion is observed (yellow arrows) (Haematoxylin & Eosin; 400x).
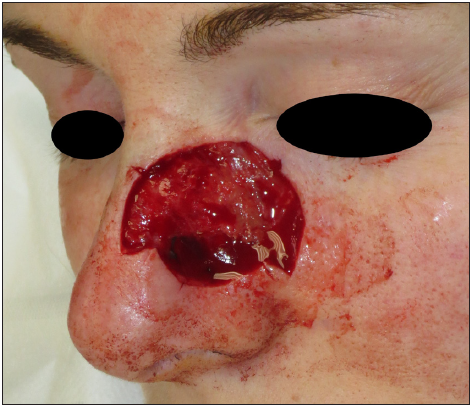
- Resulting defect after three stages of Mohs micrographic surgery.
- One-year follow-up after surgery.
The incidence of BCCs in young individuals is on the rise.3 Despite some authors suggesting that younger patients are more likely to have aggressive BCCs, others argue that there is a similar distribution of BCC subtypes across age groups.4 The authors’ clinical experience is in keeping with the former view. Additionally, while the overall incidence of BCCs is higher in men than in women, the incidence of BCCs among women under the age of 40 is higher compared to men.1 Less than 10% of BCCs correspond to the morpheaform (sclerosing, desmoplastic) or infiltrative subtypes, which are known to be more challenging to treat due to their aggressive behaviour and higher rates of local recurrence.3
Morpheaform BCCs usually present clinically as an infiltrated plaque with poorly defined borders and shiny surfaces, whilst infiltrative BCCs tend to present as a poorly defined, indurated, flat or depressed plaque with white, yellow, or pale pink colour. Both morpheaform and infiltrative subtypes are commonly found on the head and neck region.1,3
Dermoscopically, morpheaform BCC is usually associated with porcelain white areas and arborizing vessels and infiltrating BCC with arborizing vessels and ulceration.5 However, in our case only a subtle effacement of follicular openings was noted with no evidence of fibrotic beams or featureless white areas. This is particularly significant when assessing comparisons with stromal density and fibrosis in the biopsy, as such characteristics were not discernible through dermoscopy.
Histologically, thin cords with angulated ends of very few basaloid keratinocytes are seen. In the case of infiltrative BCC, basaloid cells are embedded in a classic mucinous/myxoid stroma. In morpheaform tumours, a sclerotic collagenous stroma surrounds the basaloid cords. Peripheral palisading and stromal cleft formation are not usually seen, and tumour stroma stains are positive for smooth muscle alpha-actin with immunohistochemistry.3
Given the high recurrence rates and aggressive behaviour of morpheaform and infiltrative basal cell carcinomas, it is essential to employ total margin control techniques such as Mohs micrographic surgery to ensure a complete excision in young patients with facial BCCs.
Due to the diverse range of clinical manifestations of BCC, it is crucial to maintain a high index of suspicion for malignancy in cases of hypopigmented lesions on the face, particularly when there is a loss of follicular openings. Histological confirmation can aid in early diagnosis and mitigate potential morbidity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Basal cell carcinoma masquerading as vitiligo in a young woman. J Am Acad Dermatol. Case Rep. 2020;6:584-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pityriasis alba - common disease, enigmatic entity: Up-to-date review of the literature. Pediatr Dermatol. 2015;32:786-91.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-17.
- [CrossRef] [PubMed] [Google Scholar]
- Aggressive basal cell carcinoma in young patients: Fact or fiction? Br J Plast Surg. 2000;53:393-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of basal cell carcinoma and its subtypes: A systematic review. J Am Acad Dermatol. 2021;85:653-64.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






