Translate this page into:
Managing outbreak of community-onset paediatric impetigo in underserved areas of North India via teledermatology: A tertiary care centre’s experience
Corresponding author: Dr. Amit Agarwal, Department of Telemedicine, Postgraduate Institute of Medical Sciences and Research (PGIMER), Chandigarh, India. agarwal.amit1982@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vashisht KR, Gupta R, Sahu P, Mandula PP, Dash N, Eragam A, et al. Managing outbreak of community-onset paediatric impetigo in underserved areas of North India via teledermatology: A tertiary care centre’s experience. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1102_2023
Dear Editor,
This report offers a concise account of the management of an impetigo outbreak between July and September 2023 in North India’s Haryana state, utilising tele-dermatology. Specialist physicians at our tertiary care hospital oversaw the response via e-Sanjeevani 2.0, the National Telemedicine platform of the Ministry of Health and Family Welfare, Government of India.1 This is the world’s largest documented telemedicine implementation in primary healthcare, connecting referring healthcare providers (RHPs) at peripheral centres to specialists at higher centres, following a ‘Hub and Spoke’ model.1 While a large regional community outbreak occurred spanning across three months, the innovative use of telemedicine enabled timely diagnosis, treatment and enforcement of prevention strategies.
Impetigo, a contagious skin infection predominantly affecting children, often causes unpredictable and rapid outbreaks.2 The disease burden is exacerbated in remote areas with limited response capabilities, including specialist availability, influenced by loco-regional factors like large family sizes, low socioeconomic status, and overcrowding.2–4 In such scenarios, it may secondarily infect pre-existing dermatoses like scabies or eczema.4 Patients often receive suboptimal care due to delayed treatment and misdiagnosis. Timely management is important as the highly communicable nature of the disease can cause rapid community transmission, institutional outbreaks, and disruptions in school attendance.2 Left untreated, impetigo may rarely result in serious complications including abscesses, cellulitis, post-streptococcal glomerulonephritis, acute rheumatic fever, and rheumatic heart disease.3,4
Qualified specialists, including two dermatologists and two paediatricians, conducted remote virtual assessments of impetigo lesions and gathered pertinent patient details via e-Sanjeevani 2.0, a real-time telemedicine platform that offers secure audiovisual, image, and text exchange between RHPs at peripheral centres and specialist physicians at the central ‘hub’. In alignment with established clinical practice, the diagnosis of impetigo relied on clinical rather than bacteriological findings.5 Between July and September 2023, a total of 165 cases of paediatric impetigo (≤18 years) were managed via teleconsultation, accounting for nearly 23% of the total paediatric teledermatology cases consulted during this period. This marked a substantial rise compared to previous months [Figure 1]. Of the cases seen, the mean (±SD) age was 4.25 (±2.9) years, and the male-to-female ratio was 3:2. The highest impact districts were Nuh, Faridabad, and Karnal, representing 18.78%, 10.9%, and 10.3% of all cases, respectively. Following standard guidelines, 15.8% of localised cases received treatment with topical antibiotics (fusidic acid, mupirocin), while more extensive cases were prescribed concomitant oral antibiotics (amoxicillin/clavulanic acid, cephalosporins), with the choice influenced by local availability and affordability.3,5 Localised lymphadenopathy was recorded in three cases and fever in six (managed conservatively), though none were complicated enough to warrant referral. All cases received thorough counselling on hand hygiene, local wound care, isolation measures, and surface disinfection.6 The retrospective analysis, approved by the Institutional Ethics Committee, adhered to ethical guidelines and ensured patient anonymity throughout the process.

- Bar diagram illustrating the month-wise distribution of paediatric impetigo cases managed via teleconsultation in 2023, demonstrating a sharp increase during the outbreak period (July-September), with the x-axis representing affected months and the y-axis depicting the number of cases.
To better assess the impact of teleconsultations, an anonymised standardised questionnaire was administered to the RHPs in high-impact districts, after obtaining informed consent. All 18 participants reported improved capabilities in identifying, treating, and counseling paediatric impetigo cases, and that they received follow-ups of treated cases with clinical improvement. 72% of respondents reported additional impetigo cases coming to them beyond teleconsultations, 55% engaged in outreach programs like school visits/community camps encountering more cases, and 83.3% noted a gradual decrease in cases since the peak outbreak. These findings indicate an underestimated outbreak size as well as the educational value of the teleconsultation service for RHPs. It may be inferred that by enhancing their knowledge of impetigo management, the service led to improved case handling, hygiene counselling, and awareness among patient families, and consequently, a more successful containment of disease spread. Undoubtedly, it not only eliminates travel inconvenience for uncomplicated cases but also reduces the overall burden on the healthcare system.1,7
The study had limitations, including constraints in conducting remote assessments, lack of follow-up teleconsultations to evaluate therapy response or relapse, and the inability to perform cultures for methicillin-resistant Staphylococcus aureus (MRSA) or nasal colonisation. Even so, it is noteworthy that skin swabs cannot reliably differentiate infection from colonisation and hence are not essential for making a diagnosis.5 Nonetheless, with nasal colonisation known to occur in nearly 60% of impetigo cases versus 30% in the general population, telemedicine offers an avenue for implementing decolonisation strategies, potentially decreasing treatment resistance and relapse.7 Gaining insights into the varying impact levels across different districts during outbreaks aids in the strategic allocation of health resources and initiatives [Figure 2]. In summary, this report highlights the role of telemedicine in the outbreak response of highly contagious skin infections, emphasising its capacity to provide timely, accessible healthcare, in remote and resource-constrained settings, bridging gaps in distance, time, and cost.1
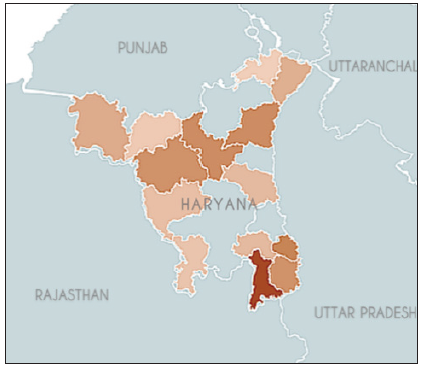
- A heatmap depicting the districts of the state of Haryana affected by the impetigo outbreak, with colour intensity reflecting the degree of impact, measured by the number of cases. Although paediatric teledermatology consultations were sought from all districts, the outbreak demonstrated varied distribution. Such visual representations, derived from teleconsultation datasets, hold potential value in directing health resource allocation and focused public initiatives.
Ethical approval
The research/study was approved by the Institutional Review Board at Institutional Ethics Committee, PGIMER, Chandigarh, number PGI/IEC/2023/EIC000523, dated 10/02/2023.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Funded by the National Health Mission, Haryana, India.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing/editing of the manuscript and no images were manipulated using AI.
References
- ESanjeevani. eSanjeevani. (Accessed December 23, 2023). https://esanjeevani.mohfw.gov.in/#/about
- Common community-acquired bacterial skin and soft-tissue infections in children: An intersociety consensus on impetigo, abscess, and cellulitis treatment. Clin Ther. 2019;41:532-51.
- [CrossRef] [PubMed] [Google Scholar]
- Emerging treatment strategies for impetigo in endemic and nonendemic settings: A systematic review. Clin Ther. 2021;43:986-1006.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric impetigo: An expert panel opinion about its main controversies. J Chemother Florence Italy. 2022;34:279-85.
- [CrossRef] [PubMed] [Google Scholar]
- Outbreak of staphylococcal bullous impetigo in a maternity ward linked to an asymptomatic healthcare worker. J Hosp Infect. 2007;67:264-70.
- [CrossRef] [PubMed] [Google Scholar]
- Staphylococcus aureus nasal colonization: An update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






