Translate this page into:
Refractory and disfiguring facial chromoblastomycosis caused by Exophiala spinifera responsive to posaconazole in an immunocompetent patient
Corresponding author: Dr. Indukooru Subrayalu Reddy, Department of Dermatology, Apollo Hospital, Jubilee Hills, Hyderabad, India. drreddyis@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy IS, De Padua M, Gowrishankar S, Polati VR, Ratnamani MS. Refractory and disfiguring facial chromoblastomycosis caused by Exophiala spinifera responsive to posaconazole in an immunocompetent patient. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1061_2023
Dear Editor,
Chromoblastomycosis is a chronic, indolent, granulomatous disease caused by the transcutaneous inoculation of conidia and/or mycelia from several species of melanized fungi. Among the various species that can cause chromoblastomycosis, Fonsecaea pedrosi and Cladophialophora carrionii are the commonest.1 Exophiala spinifera (E. spinifera) is one of the rare species of dematiaceous fungi which more commonly causes phaeohyphomycosis and only rarely is it implicated in the causation of chromoblastomycosis. We present a patient with chromoblastomycosis caused by E. spinifera with no response to routine oral antifungals and a dramatic improvement with posaconazole.
A 26-year-old man presented with an itchy, erythematous, mildly scaly plaque involving the lower lip, angles of the mouth, and upper part of the chin for 2 years [Figure 1]. The differential diagnoses considered were lupus vulgaris, discoid lupus erythematosus, and sarcoidosis. The skin biopsy showed granulomatous inflammation with lymphocytes, few aggregates of neutrophils, and giant cells exhibiting brownish-pigmented sclerotic bodies which confirmed the diagnosis of chromoblastomycosis. A touch preparation of the skin biopsy specimen in KOH showed sclerotic bodies. The patient had already received itraconazole 200 mg/d for 2 years with no response. Hence, he was shifted to a combination of voriconazole 200 mg/d and terbinafine 500 mg/d for a period of 6 months. Despite the second-line treatment, skin lesions progressed to involve both lips and the right nasolabial area with the development of indurated, hyperpigmented, and mamillated plaques on the nose and haemorrhagic, necrotic, and crusted plaque over the right angle of the mouth with intractable itching [Figure 2]. A second biopsy done also showed a granulomatous reaction with giant cells containing thick-walled golden-brown sclerotic bodies consistent with chromoblastomycosis [Figure 3]. Fungal culture of the biopsy specimen, on Sabouraud’s dextrose agar grew moist, yeast-like mucoid colonies with black reverse [Figure 4]. Lactophenol cotton blue mount showed dark coloured, erect, multiseptate, cylindrical, spine-like conidiophores. Conidia were seen to arise apically as well as laterally at acute angles [Figure 5]. Based on the above morphological features, the isolate grown in culture was identified as E. spinifera. The patient was initiated on posaconazole 600 mg/d for 1 week followed by 300 mg/d. After 6 months, there was significant improvement. The hyperpigmented plaque on the nose and right nasolabial area healed with post-inflammatory depigmentation. The haemorrhagic and necrotic erosion over the right angle of the mouth resolved with scar formation [Figure 6]. The patient continues to take posaconazole in a 300 mg daily dose and at the end of 1 year is free of itching with complete resolution of skin lesions. The plan is to continue the same treatment for a further period of 6 months. We describe a rare case of recalcitrant chromoblastomycosis caused by Exophiala spinifera of which there are only a few case reports in the literature.2 Important diagnostic investigations essential to establish a diagnosis include KOH preparation of the skin scrapings, histopathology, fungal culture, and molecular methods. Giant cells showing pigmented structures known as sclerotic or Medlar bodies are pathognomonic for the infection.3 Colonies on culture are classically slow-growing, dark, and velvety with a black obverse, which after 2 weeks of incubation at 25°C, show suede-like aerial mycelium. Under the microscope, septate, branched, pale brown hyphae with several lateral and erect spine-like conidiophores typical of E. spinifera are observed.

- Macerated and crusted plaque with erosions over the lower lip, angles of the mouth, and chin.

- Hyperpigmented, indurated plaque over the lips, right nasolabial area. Hyperpigmented mamillated plaque over the nose and necrotic ulcer involving the right angle of the mouth.
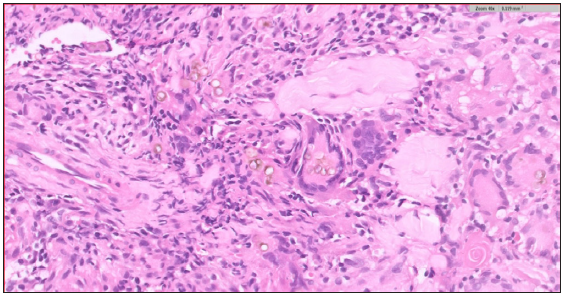
- Granulomatous inflammation with giant cells showing thick-walled golden-brown structures – medlar bodies (Haematoxylin & Eosin, 400x).
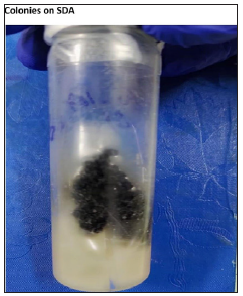
- Sabouraud’s dextrose agar, showing yeast-like mucoid colonies with black reverse.
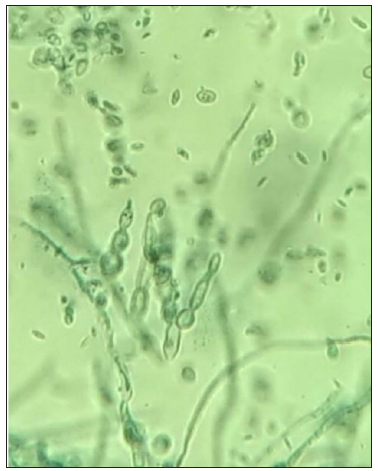
- Lactophenol cotton blue mount showing erect, multiseptate, cylindrical, spine-like conidiophores (1000x).

- The plaque on the nose, nasolabial area, lips, and necrotic ulcers over the right angle of the mouth healed with depigmentation and scarring.
Physical modalities, surgery, and oral anti-fungal drugs are recommended alone or in combination for the treatment. Itraconazole 200 mg to 400 mg daily for 8–36 months is the most commonly used regime.4 There is also a report of the successful treatment of chromoblastomycosis caused by E. spinifera with oral itraconazole and liquid nitrogen cryotherapy. Terbinafine is the second most common oral anti-fungal agent, administered for several months to years, at a dose of 250 mg to 500 mg daily5 Criado et al. reported three patients with extensive, long-standing chromomycosis due to F. pedrosi showing significant improvement with voriconazole.6 As in our patient, a significant number of patients with chromoblastomycosis do not achieve sustained long-term improvement with conventional anti-fungal drugs. A small, uncontrolled study by Negroni et al. suggested that posaconazole, a newer anti-fungal agent, is effective in recalcitrant chromoblastomycosis. Four out of six patients with chromoblastomycosis, refractory to itraconazole, terbinafine, and flucytosine, achieved complete clinical response to posaconazole 800 mg daily given in two or four divided doses for up to 12 months.7
Our case demonstrates some unusual characteristics of chromoblastomycosis, the involvement of the face with severe disfiguration, the causative agent being E. spinifera and the non-response to conventional anti-fungal agents with a remarkable clearance with posaconazole.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Chromoblastomycosis: An overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- [CrossRef] [PubMed] [Google Scholar]
- Chromomycosis caused by Exophiala spinifera. Clin Exp Dermatol. 2006;31:239-41.
- [CrossRef] [PubMed] [Google Scholar]
- Morphologic findings of deep cutaneous fungal infection. Am J Dermatopathol. 2014;36:531-56.
- [CrossRef] [PubMed] [Google Scholar]
- Itraconazole in the treatment of chromoblastomycosis due to Fonsecaea pedrosi. Int J Dermatol. 1992;31:805-12.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of chromomycosis with terbinafine: Preliminary results of an open pilot study. Br J Dermatol. 1996;134:33-6.
- [Google Scholar]
- Extensive long-standing chromomycosis due to Fonsecaea pedrosi; three cases with relevant improvement under voriconazole therapy. J Dermatol Treatment. 2011;22:167-74.
- [Google Scholar]
- Posaconazole treatment of refractory eumycetoma and chromoblastomycosis. Rev Inst Med Trop, Sao Paulo. 2005;47:339.
- [CrossRef] [PubMed] [Google Scholar]





