Translate this page into:
Co-occurring livedoid vasculopathy and limited cutaneous systemic sclerosis associated gangrene successfully managed with alprostadil and aspirin
Corresponding author: Dr. Rahul Mahajan, Department of Dermatology, Venereology and Leprology PGIMER, Chandigarh, India. drrahulpgi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Baskaran N, Mustari A, Malhi K, Bishnoi A, De D, Handa S, et al. Co-occurring livedoid vasculopathy and limited cutaneous systemic sclerosis associated gangrene successfully managed with alprostadil and aspirin. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_89_2024
Dear Editor,
Livedoid vasculopathy is a rare vascular thrombosing disorder that presents with recurrent painful ulceration on the distal lower extremities. The association of livedoid vasculopathy with systemic sclerosis is exceedingly uncommon.1 Prostaglandin analogues, commonly used for the treatment of digital ulcers in systemic sclerosis, have been found effective for ulcers of livedoid vasculopathy in a few case reports. We report a case of systemic sclerosis–associated digital gangrene and livedoid vasculopathy with a favourable response to alprostadil, a prostaglandin E-1 agonist.
A 43-year-old man presented with a one-year history of Raynaud’s phenomenon, sclerodactyly, digital tip ulcers and pitted scars. There was binding down of skin over the hands, feet, face and neck. There were a few mat-like telangiectasias on the cheeks. The modified Rodnan skin score was 10. He also had multiple, small, well-defined ulcers with irregular borders, more prominent on the left medial malleolus, for the past six months. There were geometrical porcelain white scars with peripheral hyperpigmentation and telangiectasias, more prominent on the right medial malleolus [Figure 1]. There was painless, blackish discolouration over the distal part of the second toe of the right foot. The peripheral pulses were palpable. The patient complained of on-and-off pus discharge from ulcers and a continuous dull aching pain at the site of ulceration, which was exacerbated by touch and warm weather. There was no history of smoking, intermittent claudication, rest pain, or significant systemic symptoms.

- Multiple well-defined ulcers with irregular borders on the medial malleolar region with adherent yellowish-brown crusting on the surface.
The complete hemogram, liver and renal biochemistries and coagulation profile (prothrombin time, activated partial thromboplastin time, INR) were within the normal limits. Anti-nuclear antibodies (3+ intensity; nuclear speckled pattern on indirect immunofluorescence) and anti-topoisomerase antibodies (2+) were positive. The work-up for hypercoagulable states, including protein C, protein S, anti-thrombin Ⅲ, homocysteine, lupus anticoagulant and serum protein electrophoresis, were within the normal limits. The computed tomography (CT) chest showed limited bilateral symmetrical peripheral intralobular septal thickening with patchy ground glass opacities suggestive of interstitial lung disease. Echocardiogram, barium swallow, 24-hour urine protein and pulmonary function tests were normal. Ultrasound Doppler of the arterial and venous systems of both lower limbs demonstrated normal triphasic flow in vessels with no obvious abnormality. Skin biopsy from the ulcer margin showed fibrin thrombi occluding the lumen of small vessels in the upper and lower dermis, with a mild inflammatory infiltrate in the perivascular location consistent with livedoid vasculopathy [Figure 2].
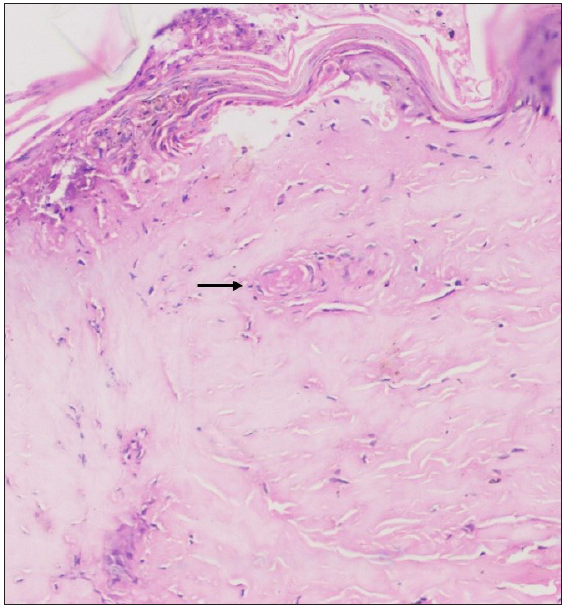
- Fibrin thrombi (black arrow) occluding the lumen of small vessels in the dermis with mild inflammatory infiltrate in the perivascular location (Haematoxylin and eosin, 200x).
The patient fulfilled the American College of Rheumatology-European League Against Rheumatism (ACR-EULAR) classification criteria for systemic sclerosis. A final diagnosis of limited cutaneous systemic sclerosis with livedoid vasculopathy and digital gangrene was reached. The patient was treated with nifedipine 20 mg/day and aspirin 75 mg/day. In view of digital gangrene, alprostadil 250 μg intravenously was administered over five days along with cold protection. Pain reduced a month after the first cycle of infusions, and the ankle ulcers started healing after that. A total of three cycles of alprostadil were administered at monthly intervals. Complete healing of ulcers with stellate scars occurred after the third cycle of alprostadil [Figure 3]. Due to the persistence of the ulcers for six months prior to treatment, the immediate symptomatic relief in pain after the first cycle of alprostadil and the complete healing of ulcers after subsequent cycles; the improvement was attributed to alprostadil. Raynaud’s phenomenon was well-controlled and gangrene of the toe also recovered. The patient has been under follow-up for 12 months after the last cycle of alprostadil and has experienced no further recurrence of ulcers.

- Complete healing of ulcers with stellate scars (black arrow) post-treatment.
Livedoid vasculopathy is a vascular hyalinising disorder characterised by the thrombosis of vessels.2 Hypercoagulability forms the cornerstone of the pathogenesis, leading to thrombosis of vessels, occlusion of cutaneous microvasculature and, subsequent ulceration of the skin. The ulcers have a predilection for the lower extremities, are characteristically small, irregular and painful and heal with classical porcelain white stellate scars termed atrophic blanche.
Vasculopathy plays an important role in the pathogenesis of systemic sclerosis. There is vascular occlusion and fibrosis due to interactions between the endothelial cells, smooth muscle cells, extracellular matrix, and mediators like endothelin. In a retrospective series by Furtado et al., at least one microvascular complication was present in 50.5% of cases with systemic sclerosis. They also found elevated D-dimer levels in 43.5% of cases and proposed it to be the cause of microvascular and macrovascular complications.3 The ulcers and gangrene associated with systemic sclerosis are more common on the fingers, though the involvement of the toes can occur. However, the association of livedoid vasculopathy with systemic sclerosis is rare.1 The presence of irregular, painful ulcers over the feet with atrophic blanche in a case of systemic sclerosis should raise the possibility of livedoid vasculopathy. A search for vascular complications, including pulmonary artery hypertension and renal crisis, should be done in such patients.3 A biopsy from the edge of the ulcer would help in establishing the diagnosis. Investigations to identify other inherited and acquired causes of thrombophilia, which would include protein C, protein S, anti-thrombin Ⅲ, homocysteine and anti-phospholipid antibodies, should be performed. Management should target the vasculopathy in addition to the standard treatment of systemic sclerosis.
Various treatment modalities for livedoid vasculopathy act by correcting coagulation abnormalities and/or controlling inflammation. Drugs acting via the coagulation pathway include anticoagulants like rivaroxaban and dabigatran, antiplatelet drugs like aspirin and fibrinolytics. Anti-inflammatory agents, including corticosteroids and immunosuppressants like azathioprine, cyclosporine, cyclophosphamide and baricitinib are also used in treatment.2
Alprostadil is a prostaglandin E1 (PGE1) agonist that causes vasodilatation by increasing cAMP production. In addition, it counteracts the vasoconstrictive effect of leukotriene D4, inhibits platelet aggregation, has cytoprotective properties, enhances fibrinolytic activity, downregulates adhesion proteins like intercellular adhesion molecule 1 and vascular cell adhesion molecule 1 (ICAM-1, VCAM-1) and E-selectin, and upregulates thrombomodulin, ultimately leading to increased vascular flow. Adverse effects with alprostadil are less common and include flushing, alterations in blood pressure and heart rate, headaches, hypokalemia, reflux and flu-like symptoms. The efficacy is comparable for most PGE1 agonists, however, alprostadil is associated with a better safety profile, a propensity to prevent new digital ulcers and lower cost.
There are previous reports of treatment of livedoid vasculopathy with prostanoids, which include four patients with PGE-1, four with beratoprost, three with iloprost and one with alprostadil-alpha.4-7 Prostanoid was chosen for treatment in our case owing to its efficacy in both Raynaud’s phenomenon and digital ulcers and livedoid vasculopathy.
In conclusion, the index case demonstrates a rare co-occurrence of livedoid vasculopathy in a man with limited cutaneous systemic sclerosis treated with alprostadil. Prostaglandin analogues are a promising treatment option for this rare co-occurrence of disorders with underlying vasculopathy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Livedoid vasculopathy: A review of pathogenesis and principles of management. Indian J Dermatol Venereol Leprol. 2016;82:478-88.
- [CrossRef] [PubMed] [Google Scholar]
- High D-dimer plasma concentration in systemic sclerosis patients: Prevalence and association with vascular complications. J Scleroderma Relat Disord. 2021;6:178-86.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Therapeutic effect of lipoprostaglandin E1 on livedoid vasculitis associated with essential cryoglobulinaemia. Br J Dermatol. 2007;157:1051-3.
- [CrossRef] [PubMed] [Google Scholar]
- Lipo-prostaglandin E1 therapy for livedo reticularis with ulceration. Acta Derm Venereol. 1997;77:246-7.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of ulcerating livedo reticularis with infusions of prostacyclin. Br J Dermatol. 1992;127:64-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of livedoid vasculopathy with alprostadil (PGE-1): Case report and review of published literature. J Eur Acad Dermatol Venereol. 2013;27:e252-4.
- [CrossRef] [PubMed] [Google Scholar]






