Translate this page into:
Inadvertent intra-arterial injection: Cutaneous complications and management
Corresponding author: Dr. Swastika Suvirya, Department of Dermatology, Venereology and Leprosy, King George’s Medical University, Lucknow, Uttar Pradesh, India. swastika.p@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pathania S, Rai A, Kumar S, Tyagi V, Agrawal T, Suvirya S. Inadvertent intra-arterial injection: Cutaneous complications and management. Indian J Dermatol Venereol Leprol. 2024;90:496-8. doi: 10.25259/IJDVL_1051_2022
Dear Editor,
One of the serious complications of intra-muscular (IM) injectable treatment is iatrogenic intra-arterial injection of the drug. Acute limb ischemia is one of the devastating sequelae following inadvertent intra-arterial injection of many drugs. This complication is relatively rare with an incidence of 1 in 3400–56000.1
A 24-year-old man presented to the dermatology outpatient department with complaints of erythematous lesions over the right forearm, along with bluish discolouration of the ring and little finger associated with pain and swelling in the same limb for last 5–6 days, following IM injection on the medial aspect of elbow by a quack. Past history was non-contributory for any connective tissue disorder, peripheral vascular disease, previous trauma or intravenous (IV) drug abuse. On examination, ill-defined, discrete, non-palpable, purpuric lesions were present on the medial aspect of the right forearm, with underlying swelling over the whole forearm along with bluish discolouration of the fourth and fifth digits of the same hand [Figure 1a]. Only radial artery was palpable. Sensations were decreased over the ring and little fingers and the medial half of the palm. On performing the Allen test, there was a significant delay in regaining vascularity of the hand. The above findings were suggestive of some vascular compromise in the territory of the ulnar artery. His coagulation profile and pro-coagulant work-up were normal. X-ray neck was non-contributory. Colour Doppler showed monophasic flow in the right ulnar artery. Right ulnar sensory neuropathy was found on nerve conduction study. CT angiography revealed markedly attenuated palmar digital branch of common palmar digital artery of the fourth and fifth digits of the right hand [Figure 2]. The patient was given oral anticoagulants for 4 weeks. A week later, the erythematous lesions completely subsided, but the bluish discolouration of fingers persisted [Figure 1b]. Three weeks later, the patient developed gangrene over the tip of the ring and little fingers with a clear line of demarcation between affected and non-affected parts of the fourth and fifth digits [Figure 1c], which was shed off and replaced by scar tissue in the next 6 weeks [Figure 1d].
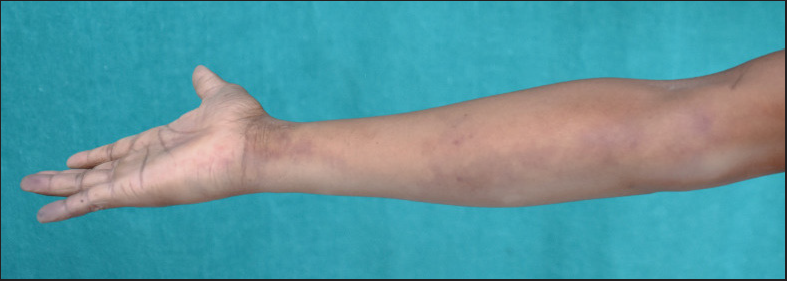
- Multiple discrete purpuric lesions, with swelling on the medial aspect of the forearm along with bluish discolouration of the fourth and fifth digits.

- Disappearance of the purpuric lesions but persistence of bluish discolouration of the fourth and fifth digits.

- Palmar aspect of the hand showing dry gangrene on tips of the fourth and fifth digits with a clear line of demarcation.

- Digits after healing with scar tissue.
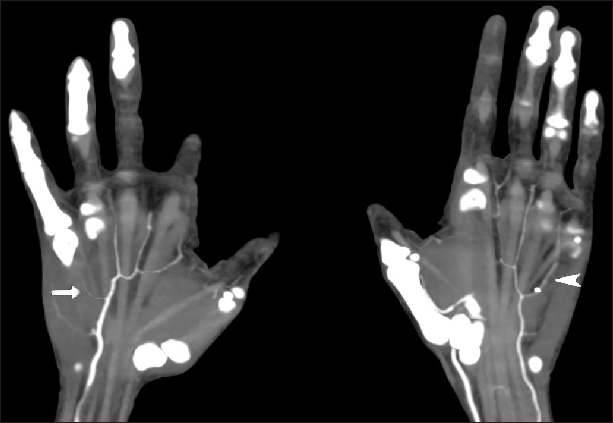
- Coronal CT angio arterial phase image of bilateral hands showing severe luminal narrowing of the common palmar digital artery supplying the fourth and fifth digits of the right hand (arrow head) as compared to the normal common palmar digital artery supplying the fourth and fifth digits of the left hand (arrow head).
IM injection is a technique of injecting a drug directly into the muscle to improve its efficacy and for rapid onset of action. As compared to an IV injection, it is easy to administer and is the most frequently performed medical procedure.2 Intra-arterial cannulation can rarely occur if proper guidelines for IM injection have not been adhered to. We are reporting a case of accidental intra-arterial injection, with isolated ulnar artery involvement leading to gangrene of the fingertips of the fourth and fifth digits and sensory neuropathy of the ulnar nerve.
In our case, intra-arterial cannulation occurred while attempting IM injection (Diclofenac) on the medial aspect of the forearm, which is not an ideal site for IM injection. The deltoid, ventrogluteal and vastus lateralis are ideal muscles for IM injection as these are present at a safer distance from major vessels and nerves, while having sufficient bulk to accommodate the volume of the drug administered. This usually happens when Benzyl alcohol-based preparations of diclofenac are administered by IV/intra-arterial route. So, it is equally essential to have knowledge about the composition of the drug and the route of administering the same.3
Dermatological findings like bluish discoloration of the digits, presence of purpurae with prior history of any injectable can help in clinching the diagnosis. There are very few case reports of such a clinical presentation, particularly the presence of purpura.4
One of the important differential diagnoses of this condition is Nicolau syndrome, in which ulceration and necrosis are usually present at the site of injection. But in the present case, the gangrenous changes were seen at a distant site. There are no exact treatment guidelines to manage this condition. Both conservative and surgical modalities (embolectomies/fasiotomies) have been tried with variable success rate.5 Conservative management includes drugs like opiods, corticosteroids and anticoagulants, and vasodilators such as reserpine, iloprost and papaverine, hyperbaric oxygen and regional nerve blocks.
From this case report, we want to convey that there should be more emphasis on strengthening of institutional set-ups and appropriate training of all healthcare providers. Adequate knowledge about the composition of the drug, the route of administering the medication and early identification of signs and symptoms of accidental intra-arterial drug administration can help in preventing this dreaded complication and reduce patient morbidity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Inadvertent intraarterial injection leading to gangrene: A rare but devastating postoperative complication. J Obstet Gynaecol India. 2012;62:56-8.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of vibration stimulation on intramuscular injection pain and patient satisfaction: Single–blind, randomised controlled study. J Clin Nurs. 2021;30:1615-22.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence, significance, and management of accidental intra-arterial injection: A narrative review. Can J Anaesth. 2019;66:576-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Localized retiform purport after accidental intra-arterial injection of polidocanol. Acta Derm Venereol. 2005;85:372-3.
- [CrossRef] [PubMed] [Google Scholar]
- Accidental intra-arterial injection: A case report, new treatment modalities, and a review of the literature. J Oral Maxillofacial Surg. 2006;64:965-8.
- [CrossRef] [PubMed] [Google Scholar]





