Translate this page into:
A man with skin tumours on the right thigh
Corresponding author: Dr. Yuchong Chen, Department of Dermatologic Surgery, Shanghai Skin Disease Hospital, Shanghai, China. YuchongChen_tongji@163.com
-
Received: ,
Accepted: ,
How to cite this article: Wu L, Chen Y. A man with skin tumours on the right thigh. Indian J Dermatol Venereol Leprol. 2024;90:532-4. doi: 10.25259/IJDVL_910_2023
A 68-year-old man presented with skin lesions on his right thigh for 6 years. The patient developed a red pea-sized nodule on his right thigh 6 years ago, without experiencing any symptoms. The nodule gradually grew and was removed surgically. Four years ago, the patient presented with similar nodules in the same area, accompanied by mild itching, which were also excised surgically. After six months post-surgery, a similar nodule reappeared at the incision site, and another doctor preliminarily diagnosed it as a keloid. Physical examination showed dark red irregular exophytic nodules with a hard consistency [Figure 1a]. The lesion was mainly located within the dermis, with an ill-defined indurated base [Figure 1b]. After ineffective treatment with an intradermal corticosteroid injection, the patient presented to us, and the lesion was excised again. The histopathological and immunohistochemical results showed spindle cell tumours with SMA(+), CD99(+), Calponin(+), S-100(-), EMA(-), CK(-), Desmin(-) and Ki-67 (20%+) [Figures 2a–2d].

- Recurrent skin tumours on right thigh.
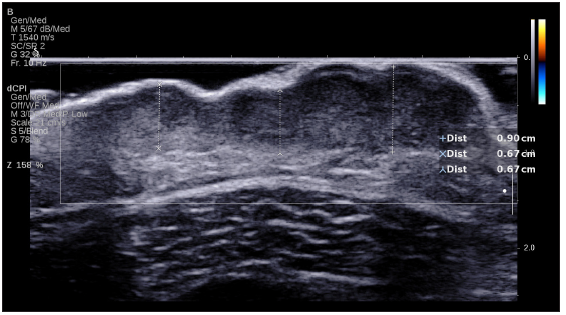
- Under ultrasound, the tumour presents with low echogenicity, primarily located within the dermis. It exhibits unclear boundaries, irregular surface protrusions, and a blurred base. Colour doppler flow imaging reveals abundant blood flow signals.
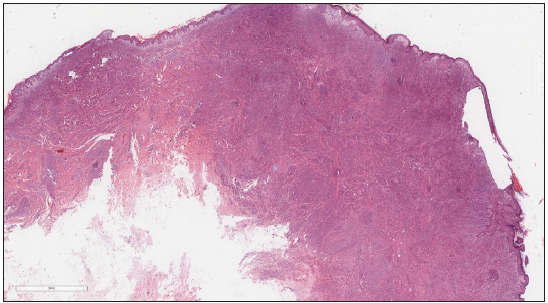
- Epithelioid and fusiform cells diffusely infiltrate from dermis to subcutaneous adipose layer, with interstitial mucoid degeneration. (Haematoxylin and Eosin, 40x).
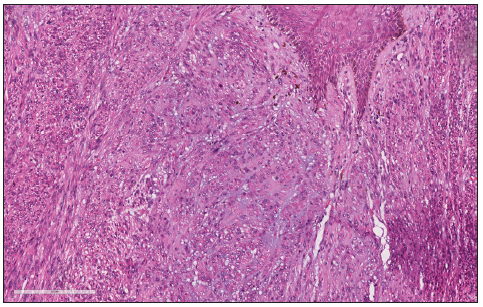
- Epithelioid cells have abundant cytoplasm, round nuclei and a vacuolar shape; fusiform cells arranged in bundles or interweaving (Haematoxylin and Eosin, 200x).
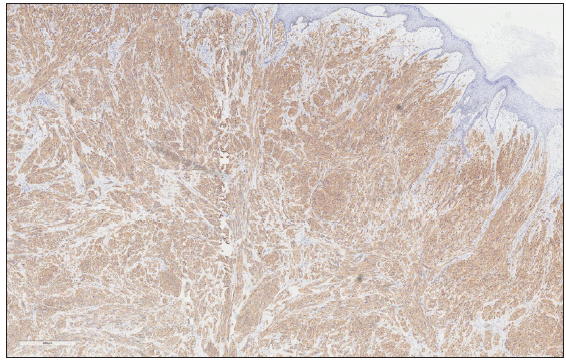
- Immunohistochemical staining of Smooth muscles actin (SMA) of tumour cells (100x).
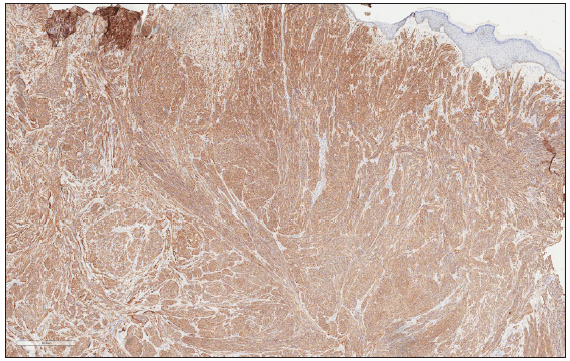
- Immunohistochemical staining of Calponin of tumour cells (100x).
Question
What is your diagnosis?
Diagnosis
Superficial cutaneous leiomyosarcoma (SCLM).
Discussion
Based on the history of recurrence, clinical manifestations and pathology, the patient was diagnosed with SCLM rather than skin leiomyoma. Both skin leiomyosarcoma and skin leiomyoma are types of smooth muscle tumours, and they express smooth muscle-specific markers such as smooth muscles actin (SMA), desmin and calponin. However, in comparison to leiomyoma, leiomyosarcoma typically displays a larger size, significant cellular atypia, a higher mitotic rate, infiltrative growth pattern, necrosis and vascular invasion.1,2
Cutaneous leiomyosarcoma is a rare malignant tumour that may be easily misdiagnosed due to its rarity and non-specific clinical manifestations.2 It is important to recognise the misleading features of this tumour. SCLM can occur in any area with hair, but it is more prone to occur in areas with a high density of hair follicles and arrector pili muscles, especially on the extensor surfaces of the lower extremities.3 The tumour in this patient occurred on the thigh, which is a predilection site. The common clinical differential diagnoses of SCLM include fibroids, persistent insect bite granulomas and cancers, among others. This patient’s tumour appeared at the surgical incision site, thus being misdiagnosed as a keloid. The most frequent symptom of SCLM is pain (80–95%), and other common symptoms include itching, feeling of heat and bleeding.3 The patient in this case had no obvious symptoms or only mild itching, which was also a factor leading to misdiagnosis.
Although surgical removal is the most effective treatment for this disease, there is still a relatively high rate of recurrence following the surgery.2 As shown by histopathology, the patient’s tumour invaded the subcutaneous adipose layer. However, chest computed tomography (CT) and abdominal ultrasound indicated that there was no tumour metastasis. To prevent a recurrence, this patient underwent expanded resection with Mohs micrographic surgery, and no recurrence has been observed so far. For primary SCLM, wide local excision, and Mohs micrographic surgery in particular, have been confirmed to be effective and recommended.1,4,5 The tumour is likely to recur due to incomplete resection. After undergoing R0 resection with 1 cm safety margins, the rate of local recurrence for SCLM is extremely low, and the occurrence of metastasis is rare.4,5 This patient experienced recurrence twice, mainly because there was no clear diagnosis in the past, which did not attract sufficient attention from the doctors and the patient. After a definite diagnosis, we suggested the patient undergo further extensive excision using the Mohs micrographic surgery; the patient has not experienced any recurrence during a 2-year follow-up. Follow-up is recommended to be conducted every six months for SCLM within the first two years after surgery.4
In this case, we aim to draw attention to two key points. First, SCLM is prone to misdiagnosis and missed diagnosis. Histopathology and immunohistochemistry (IHC) are invaluable tools for accurate diagnosis. Second, in the treatment of SCLM, wide local excision, especially Mohs micrographic surgery, is highly recommended to minimise the risk of recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Leiomyosarcoma of the skin: Clinical, histopathologic, and prognostic factors that influence outcomes. J Am Acad Dermatol. 2014;71:919-25.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Skin Sarcomas. Surg Oncol Clin N Am. 2022;31:511-25.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial cutaneous leiomyosarcoma: A rare, misleading tumor. Am J Clin Dermatol. 2008;9:185-7.
- [CrossRef] [PubMed] [Google Scholar]
- S1-guideline cutaneous and subcutaneous leiomyosarcoma. J Dtsch Dermatol Ges. 2023;21:555-63.
- [Google Scholar]
- Cutaneous mesenchymal tumors treated with Mohs micrographic surgery: A comprehensive review. Int J Dermatol. 2021;60:1334-42.
- [CrossRef] [PubMed] [Google Scholar]





