Translate this page into:
Lichen planus colocalising with vitiligo at photo-exposed sites: An example of locus minoris resistentiae
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, 126, Masjid Moth Hostel, AIIMS, New Delhi-110049, Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Patel V, Agarwal S, Khandpur S. Lichen planus colocalising with vitiligo at photo-exposed sites: An example of locus minoris resistentiae. Indian J Dermatol Venereol Leprol. 2024;90:565. doi: 10.25259/IJDVL_1168_2022
Dear Editor,
We report an interesting phenomenon observed in three patients with vitiligo. All three patients developed pruritic, flat-topped skin coloured to erythematous papules and plaques on their pre-existing vitiligo patches. In one patient, these lichenoid papules developed over the wrists, neck, upper back and waist, with a predilection for photo-exposed sites [Figure 1a], along with the involvement of some relatively photo-protected sites [Figures 1b and 1c], while in the other two patients, they developed exclusively over the dorsal hands [Figures 1d and 1e]. The clinical characteristics of all three patients are summarized in Table 1.

Itchy erythematous papules and plaques colocalising over pre-existing vitiligo patches on the wrists of a 58-year-old female on glimepiride and hydrochlorothiazide (patient 1).

Erythematous papules of lichen planus colocalising over pre-existing vitiligo patches on relatively photo-protected site on back of patient 1.

Close-up of colocalised lichen planus and vitiligo lesions on relatively photo-protected lesions of right lower back of patient 1.

Raised lesions of lichen planus colocalising over pre-existing vitiligo on the dorsa of hands of a 9-year-old boy (patient 2).
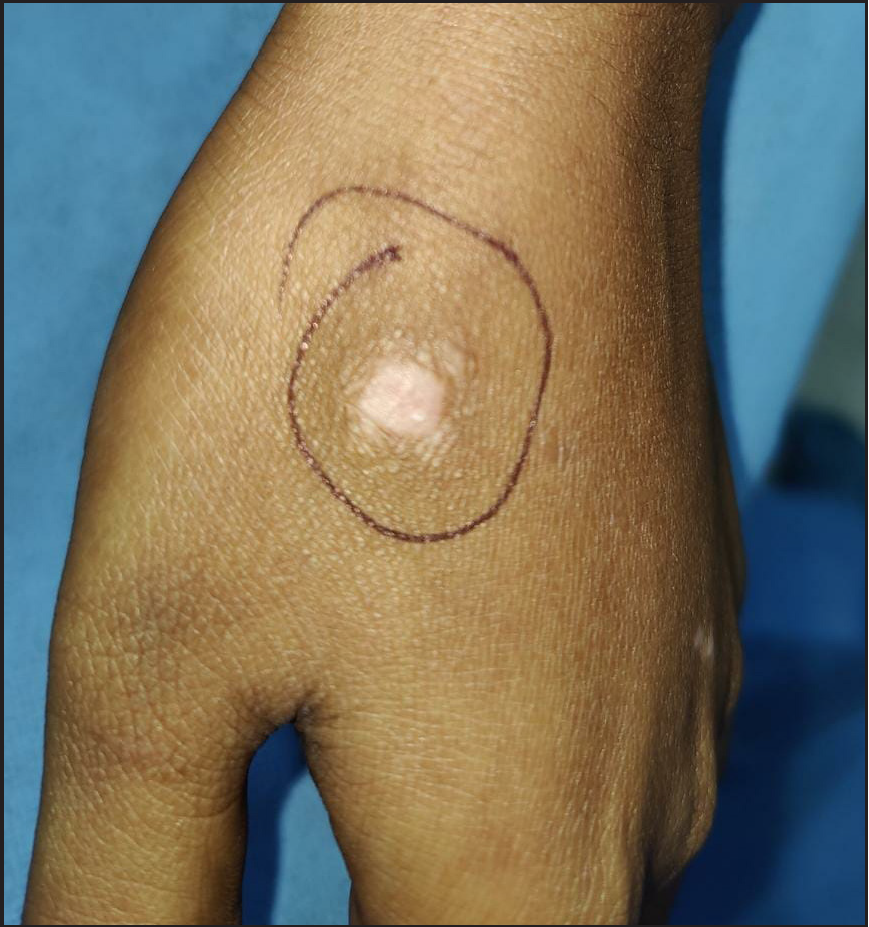
A small papule surrounded by smaller satellite papules due to lichen planus colocalising over pre-existing vitiligo on the dorsa of hands of a 21-year-old female (patient 3).
S. No.
Age, gender
Duration by which vitiligo preceded lichen planus
Sites of vitiligo
Sites of lichen planus
Symptoms and morphology
Predisposing factor(s)
1
58, female
6 years
Face, neck, distal extremities, trunk
Wrists, neck, few areas of the upper and lower back. Vitiligo patches of the chest, forearms, and legs did not develop lichen planus
Severely itchy and erythematous elevated plaques with some scaling and Wickham’s striae
On glimepiride and hydrochlorothiazide for 1.5 years
2
9, male
2 years
Dorsa of hands
Almost all macules over hand dorsa
Initially asymptomatic flat depigmented macules of vitiligo became mildly itchy and elevated, although remained depigmented
None
3
21, female
5 years
Breasts, legs, dorsa of hands and feet
All macules over hand dorsa. Lesions over other sites did not develop lichen planus
Initially asymptomatic flat depigmented macules of vitiligo became moderately itchy and elevated, although remained depigmented
None
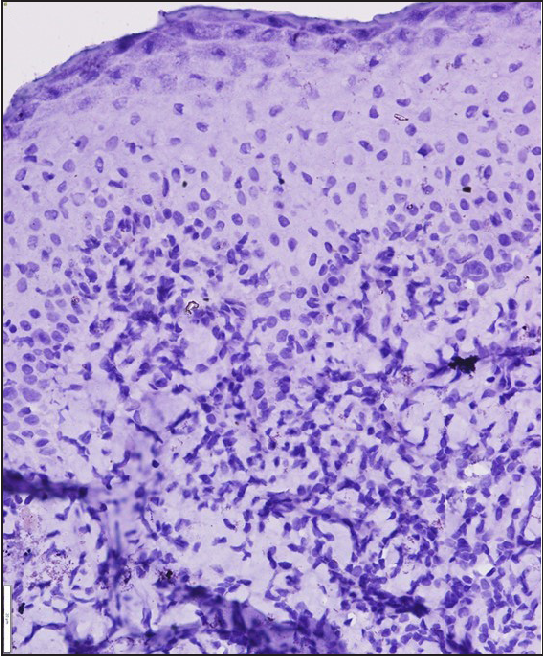
Dermoscopy of the first patient with erythematous lesions showed multiple erythematous areas with central whitish lines in a retiform and fern leaf–like branching pattern, suggestive of Wickham’s striae, surrounded by dotted and branched vessels, with a background of depigmentation without any pigmentary network. There were no dots or globules on dermoscopy [Figure 2a]. Histopathological examination in all three cases showed wedge-shaped hypergranulosis, necrotic keratinocytes in the epidermis, basal cell damage, and a dense band-like infiltrate of lymphocytes and histiocytes in the upper dermis. The features were suggestive of lichen planus (LP). There were no melanophages in the upper dermis [Figure 2b]. Special stains (Fontana-Masson and HMB 45) did not reveal any melanin [Figures 2c and 2d].
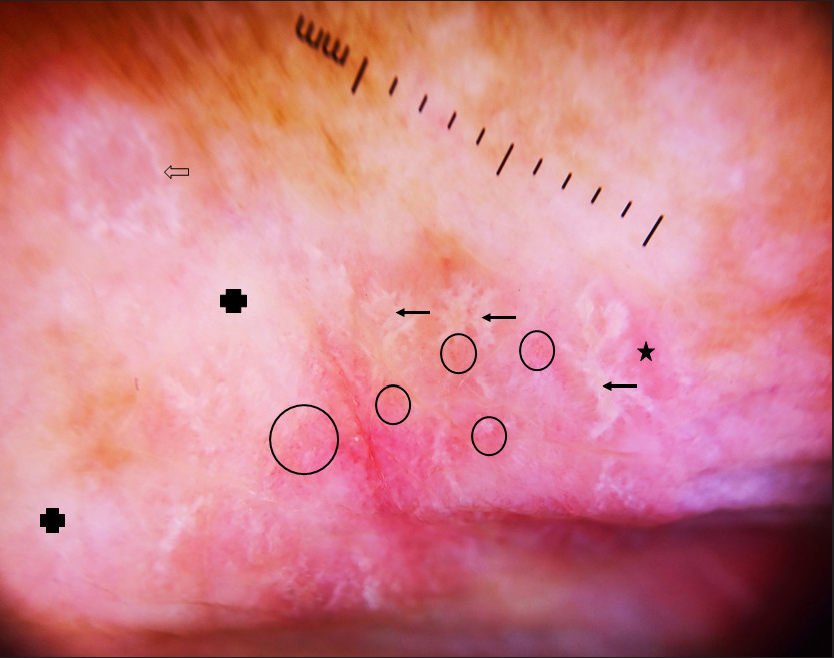
- Dermoscopy of lichen planus colocalising over vitiligo in erythematous lesions of patient 1, showing multiple erythematous areas (star) with central whitish lines in a retiform, fern leaf–like branching pattern (arrow) and annular pattern (hollow arrow), suggestive of Wickham’s striae, surrounded by dotted and branched vessels (circle), with a background of depigmentation without any pigmentary network (solid cross). There were no dots or globules (Heine Delta 20 T, 10X).
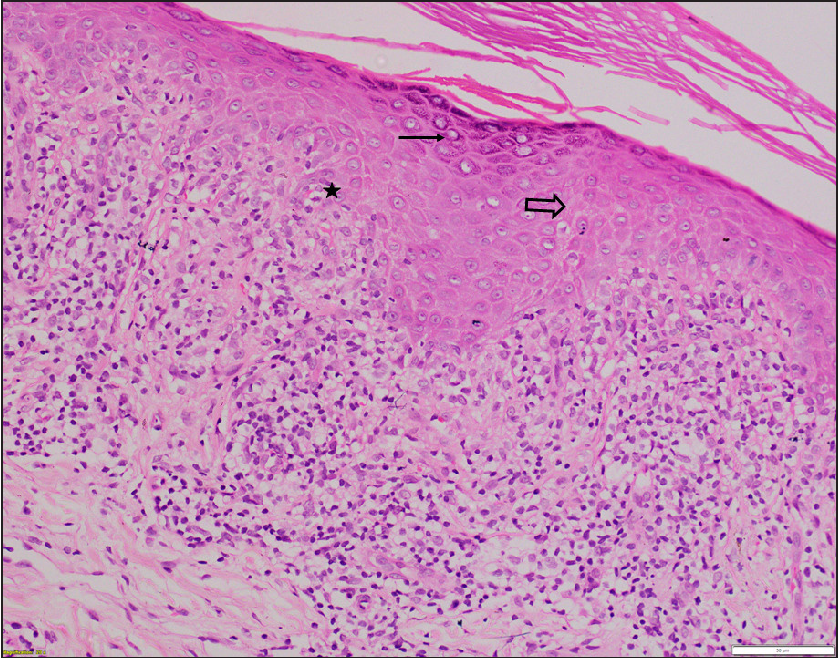
- Histopathology of lesions of patient 1 showing hyperkeratosis, wedge-shaped hypergranulosis (arrow), necrotic keratinocytes in epidermis (hollow arrow), basal cell damage (star), and a dense band-like infiltrate of lymphocytes and histiocytes in upper dermis along with few colloid bodies suggestive of lichen planus. There were no melanophages in the upper dermis (H & E, x200).
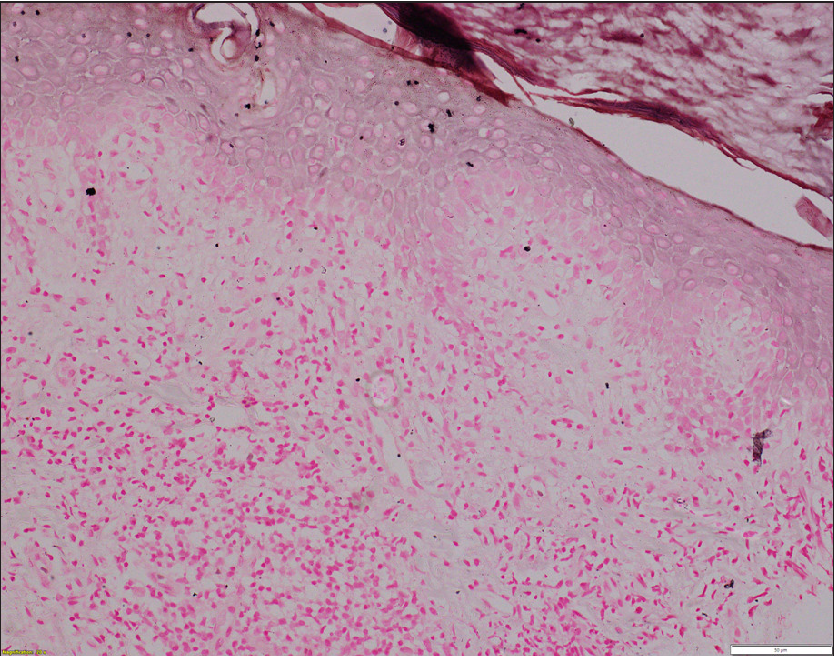
- Histopathology of lichen planus colocalising with vitiligo of patient 3. No melanin is seen (Fontana-Masson stain, x200).
- Histopathology of lichen planus colocalising with vitiligo of patient 3. No melanin is seen (HMB-45, x400).
A diagnosis of LP colocalised on vitiligo was made. The papules and plaques of lichen planus responded completely to mometasone furoate 0.1% cream applied twice daily for 2–3 months in all three patients, however the depigmented macules of vitiligo persisted in them. Itching, erythema, and elevation in the vitiligo lesions did not recur in the next one year of follow-up.
Lichen planus and vitiligo are common skin diseases. As the prevalence of both is 0.5–2% in the general population, their coexistence is not unexpected. As both are autoimmune diseases targeting the skin, with Th1 cells implicated in the pathogenesis, even an association is not hard to imagine. Early vitiligo lesions can show a mild lichenoid infiltrate, and the loss of melanocytes in vitiligo is thought to be due to a lichenoid process.1 However, the colocalization of these conditions requires a closer look.
Koebner phenomenon refers to the development of an existing skin disease on normal skin after trauma, while isotopic phenomenon refers to the development of a skin disease in areas of sequelae to a previous skin disease. Both terms are not appropriate to the phenomenon described above. The concept of locus minoris resistentiae (of which the Koebner and isotopic phenomena are examples) and Ruoco’s immunocompromised cutaneous district (ICD) are better descriptors for these cases, keeping in mind that the pre-existing vitiligo lesions constitute a pre-existing active disease rather than normal skin or sequelae of a previous resolved disease.4
In colocalised cases, usually, the vitiligo precedes the development of the lichenoid change, but simultaneous occurrence or lichen planus resolving with depigmentation can also occur.2 The lichen planus lesions are usually limited to the sites of vitiligo, but can occur over normal skin in these patients.2 Most cases are located over photo-exposed sites, however, photo-protected sites can rarely be involved.3
Various theories about this colocalization have been proposed. It is hypothesized that excessive photodamage in vitiliginous skin, which lacks the protective effect of melanocytes, incites the inflammatory response and effector T cells of lichen planus over photo-exposed sites.5 This photo-exposure may also inhibit non-specific suppressor T cells, which can lead to the development of an inflammatory response in the form of lichen planus. This “actinic damage” hypothesis provides an explanation for colocalization predominantly over photo-exposed sites and is supported by the phenomenon of development of lichenoid infiltrates in vitiligo patients after phototherapy.3 Another hypothesis involves increased expression of autoantigens of the basal layer in long-standing vitiligo cases, independent of chronic sun exposure. The role of TNF-α, an inflammatory cytokine raised in lesional and peri-lesional vitiliginous skin as well as lichen planus, has also been speculated.3
Interestingly, one of our patients was on medications (hydrochlorothiazide and glimepiride for 18 months) known to cause photo-distributed lichenoid eruptions. In her case, a triad of predisposed skin in the form of vitiligo (which lacked photoprotective effect of melanocytes), medications, and chronic sun damage could be responsible for lichen planus developing prominently over vitiligo patches in photo-exposed areas. The medications were replaced with alternatives, and the patient was given mometasone cream for 3 months with which the lesions resolved. She did not develop the lesions during the 12 months of follow-up. The other two patients responded similarly.
Other examples of lichen planus and vitiligo colocalising together with other active autoimmune disorders include the colocalization of lichen planus with subacute cutaneous lupus erythematosus, generalized morphea, lichen sclerosus, psoriasis, etc.; and colocalization of vitiligo with psoriasis, alopecia areata, subacute or discoid lupus erythematosus, etc. Immune mechanisms with or without actinic factors have been proposed to be responsible for the colocalization of these disorders with other autoimmune diseases. In such cases, usually a few lesions of the second disease develop overlying some lesions of the pre-existing extensive disease, and not all lesions colocalise. Lichen planus and vitiligo have also been reported to colocalise with non-inflammatory diseases like porokeratosis, epidermoid cysts, Becker’s naevus, verrucous epidermal naevus, etc. In such cases, usually lichen planus and/or vitiligo develop over the respective non-inflammatory diseases, and the aetiopathogenesis behind such occurrence is unclear.
Various other autoimmune and non-inflammatory diseases have been reported to colocalise. Such colocalizations exemplify a distinct subset of the immunocompromised cutaneous district (ICD) phenomenon. In many cases, if the second disease is extensive and the first was localised, then increased severity of the second limited to the sites of colocalization with the first is seen. For example, increased severity of blistering of varicella over tinea plaques. Other cited examples of ICD include the development of new skin diseases over sites with sequelae of previous skin diseases rather than over pre-existing active diseases. They include the development of new skin diseases over the sites predisposed by chronic lymphoedema (tumours like angiosarcoma, Kaposi’s sarcoma, etc., and infections/immune disorders like recurrent cellulitis), ionizing radiation (tumours), trauma/burn (tumours, infections, and immune disorders), vaccination (tumors, granulomatous disorders like granuloma annulare, and immune disorders), and varicella/herpetic infections in the past, also known as Wolf’s post-herpetic isotopic response (tumors, infections, immune disorders, and granulomatous disorders).6
In conclusion, in cases with co-existence of lichen planus with vitiligo, lichen planus usually develops on pre-existing vitiligo sites, predominantly on photo-distributed areas. Dermoscopy and histopathology show all the features of lichen planus except those suggestive of pigmentary incontinence. Sun damage in pre-disposed vitiligo patches is the most plausible mechanism, but other factors might also be involved. In such cases, other causes of photo-distributed lichenoid eruption should also be evaluated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Lichenoid inflammation in vitiligo–a clinical and histopathologic review of 210 cases. Int J Dermatol. 2008;47:663-9.
- [CrossRef] [PubMed] [Google Scholar]
- A rare colocalization of lichen planus and vitiligo. Case Rep Dermatol Med. 2015;2015:840193.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Colocalization of vitiligo and lichen planus on scrotal skin: a finding contrary to the actinic damage theory. Dermatol Basel Switz. 2006;212:390-2.
- [CrossRef] [PubMed] [Google Scholar]
- Categorization of and comments on isomorphic and isotopic skin reactions. Clin Dermatol. 2017;35:105-10.
- [CrossRef] [PubMed] [Google Scholar]
- Familial colocalization of lichen planus and vitiligo on sun exposed areas. Ann Dermatol. 2013;25:223-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The immunocompromised district: a unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-73.
- [CrossRef] [PubMed] [Google Scholar]





