Translate this page into:
Platelet-rich fibrin therapy assisted split-thickness skin graft in a non-healing morphea ulcer
Corresponding author: Dr. Senkadhir Vendhan, Consultant, Department of Dermatology, Bharat Ratna Dr Babasaheb Ambedkar Memorial Hospital, Mumbai, Maharashtra, India. vendhan100@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vendhan S, Neema S, Vasudevan B, Malla P. Platelet-rich fibrin therapy assisted split-thickness skin graft in a non-healing morphea ulcer. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1173_2023
Dear Editor,
Morphea, is an uncommon inflammatory disease that affects the skin and subcutaneous tissue.1 The pathophysiology of morphea is characterised by abnormal cytokine production, vascular dysfunction and excessive collagen deposition. The ulcers caused by morphea are generally non-healing in nature and resistant to conventional medications.2 We hereby report a case of resistant ulcer that responded rapidly to platelet-rich fibrin (PRF) therapy followed by split-thickness skin grafting (STSG).
A 37-year-old woman presented to the outpatient department with a 5-year history of pain in multiple small joints of both hands with early morning stiffness lasting 45 minutes. She had an ulcer on the right leg that was initially 1 × 1 cm in size and gradually progressed to the present size of 8 × 5 cm over a year. The ulcer was located on the right shin, and was non-tender, with sloping edges and a floor covered in yellow slough. It was not fixed to underlying structures. Dermatological examination revealed hyperextension of the metacarpophalangeal joints and swan neck deformities of multiple phalangeal joints, as well as severe wasting with shiny skin of both upper and lower limbs [Figure 1]. Laboratory tests revealed 11 gm/dL haemoglobin and normocytic hypochromic anaemia. The rest of the haematological and biochemical parameters were within normal limits.
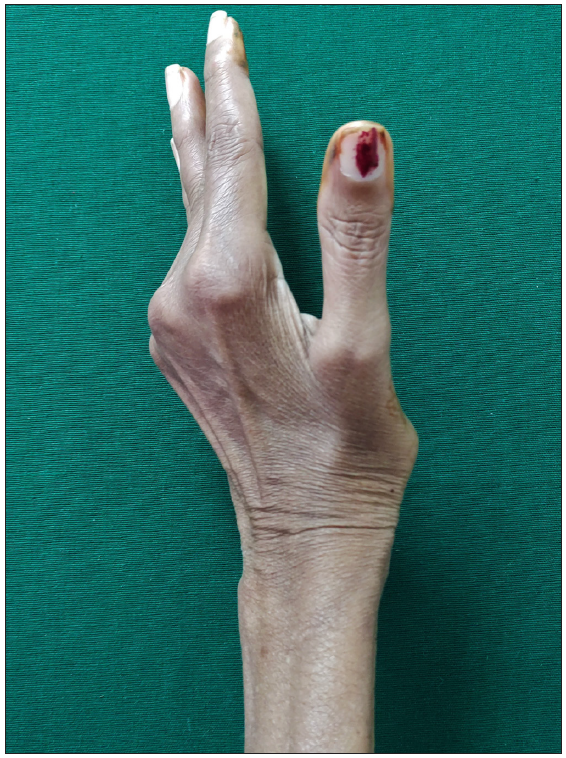
- Hyperextension of metacarpophalangeal joints with swan neck deformity of multiple small hand joints.
The antinuclear antibody level was 1:160 and the rest of the connective tissue disease serology including the extractable antinuclear antigen profile was negative. CCP was not performed. The erythrocyte sedimentation rate (ESR) was elevated. Rheumatoid factor and C-reactive protein were strongly positive. Histopathological examination of the right lower leg revealed atrophic dermis, hyalinised collagen, loss of appendageal structures, and subcutaneous fat suggestive of morphea. The patient was diagnosed with rheumatoid arthritis with morphea and was treated with oral methotrexate and sulfasalazine which resulted in improved joint symptoms but no relief from the ulcer after 6 months of treatment.
The ulcer did not respond to oral immunosuppressants, oral or topical antibiotics, collagen powder, or zinc oxide. Following this, the ulcer was treated with platelet-rich fibrin (PRF) at weekly intervals. After three sessions of PRF, the ulcer began to heal in the form of red granulation tissue. Over the ulcer site, a split-skin thickness graft was performed. After 4 weeks of a split-skin thickness graft, the patient had nearly complete resolution of the existing ulcer [Figures 2a–2c]. The patient’s 6-month follow-up revealed no relapse of the ulcer.

- Ulcer over right shin during the first visit.

- Debrided ulcer ready for platelet-rich fibrin therapy.

- Complete resolution of morphea ulcer after 3 sessions of PRF with a split-skin thickness graft.
An ulcer caused by morphea is generally considered resistant to topical treatments. A study by Kiebler et al. had used topical clobetasol ointment and topical pimecrolimus ointment in the management of ulcer caused by morphea, and it was mentioned that the ulcers took several months to heal.3 Another study by Lahouel M et al. had used topical clobetasol ointment in the management of localised bullous morphea.4 In our study, we used PRF therapy in the management of ulcer caused by morphea as PRF helps in collagen remodelling, promotes granulation tissue, and helps in better integration and acceptance of the graft. The patient’s blood sample was collected without any anticoagulant and was immediately spun in a centrifugation machine at 3,000 revolutions per minute for 10 minutes which helped in the formation of PRF scaffold matrix that contains various cytokines, platelets, leukocytes, growth factors, fibrinogen, fibronectin, vitronectin and thrombospondin-1.5 The advantage of PRF over platelet-rich plasma is that the release is slow and over a period of time making it ideal for tissue regeneration and growth stimulation.6 PRF therapy aided in the remodelling of collagen and the formation of granulation tissue, resulting in a better take-up of the split-thickness skin graft. The combination of PRF and a split-skin thickness graft improved non-healing ulcers associated with collagen vascular disorders.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- A case of extensive debilitating generalized morphea. Cureus. 2020;12:e8117.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Morphea: The 2023 update. Front Med (Lausanne). 2023;10:1108623.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leg ulcers in morphea plaques. J Dtsch Dermatol Ges. 2022;20:1365-7.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual presentation of localized bullous morphea. Dermatol Online J. 2020;26:13030.
- [PubMed] [Google Scholar]
- From platelet-rich plasma to advanced platelet-rich fibrin: Biological achievements and clinical advances in modern surgery. Eur J Dent. 2019;13:280-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leucocyte-and platelet-rich fibrin (L-PRF) as a regenerative medicine strategy for the treatment of refractory leg ulcers: A prospective cohort study. Platelets. 2018;29:468-75.
- [CrossRef] [PubMed] [Google Scholar]





