Translate this page into:
Recurrence rates after functional surgery versus amputation for nail squamous cell carcinoma not involving the bone: A systematic review
Corresponding author: Dr. Da-Guang Wang, Department of Dermatology, The First Affiliated Hospital of Nanjing Medical University, Guangzhou road, Nanjing, China. Email: wangirwin@163.com
-
Received: ,
Accepted: ,
How to cite this article: Wong H-S, Li F, Jiang J-Y, Huang S-D, Ji X, Zhu P, Wang D-G. Recurrence rates after functional surgery versus amputation for nail squamous cell carcinoma not involving the bone: A systematic review. Indian J Dermatol Venereol Leprol. 2025;91:31-9. doi: 10.25259/IJDVL_912_2023
Abstract
Background
Nail unit squamous cell carcinoma (nSCC) is a malignant subungual tumour. Although it has a low risk of metastasis and mortality, the tumour has a significant local recurrence rate. There is insufficient data to determine whether functional surgery is less effective than amputation for nSCC that does not involve the bone.
Objectives
We aimed to investigate existing data on the outcomes of functional surgery and amputation for nSCC without bone invasion.
Materials and Methods
We carried out an extensive search in PubMed, Embase, Cochrane Library, Web of Science, and Scopus for appropriate English-language academic papers, starting with the creation of individual resources until February 23, 2023. The main outcome was local recurrence. Initially, 2191 studies related to nSCC were selected. Information from every research study was retrieved and subdivided, comprising the year of publication, period, number of patients, age, gender distribution, tumour stage, type of intervention, number of recurrences, and follow-up period.
Results
Ten independent studies (319 lesions) were finally selected. Mohs micrographic surgery was the most reported surgical modality, followed by wide surgical excision and amputation. Local recurrence rates between Mohs micrographic surgery, wide surgical excision and amputation treatment were nearly identical. Other surgical methods included limited surgical excision, partial ablation, and limited excision until the clearing of margins, with recurrence rates up to 50%.
Conclusions
Given the functional impairment and psychological distress associated with phalanx amputation, functional surgery, including Mohs micrographic surgery and wide surgical excision , should be the preferred therapy for nSCC without bone involvement. Amputation should remain the preferred therapy for nSCC that involves the bone. Partial excision should be avoided. Further studies on whether Mohs micrographic surgery or wide surgical excision is a better option for nSCC not involving the bone are required.
Keywords
amputation
functional surgery
squamous cell carcinoma
systematic review
nail disease
Introduction
Nail unit squamous cell carcinoma (nSCC) represents a relatively unusual cutaneous squamous cell carcinoma variation that requires prompt diagnosis and appropriate surgical treatment. Traditionally, amputation was the standard therapy for nail unit malignancies.1 While amputation provides significant local control, it also causes remarkable physical and cosmetic damage, particularly in finger lesions. In recent years, researchers have demonstrated that functional surgery is a reliable therapeutic option that provides better function and cosmetic benefits than amputation. This is especially true in cases with nSCC without bone invasion. Functional surgery may provide successful management of minimally invasive tumours in the absence of additional negative prognostic factors. This systematic review of current studies summarises the local recurrence rates following functional surgery and amputation respectively, in nSCC without bone involvement.
Methods
Eligibility criteria for inclusion and exclusion
The goal of this systematic review was to assess whether functional surgery or amputation is the better option for nSCC not involving the bone. Thus, the primary outcome of this study was local recurrence, and the secondary outcomes were metastasis or death related to this disorder. Complete text evaluation of all accessible papers was done through the implementation of specific criteria. We did not find any randomised controlled experiments; thus, observational study designs (retrospective studies and case series) with a minimum of 5 patients with nSCC were selected. Only those studies were included which described the histopathologic diagnosis of nSCC (in situ or invasive) as well as prognostic data (average 6 months of follow-up and outcomes such as recurrence, metastasis, or death caused by the nSCC).
Squamous cell carcinoma of the nail unit was defined as squamous cell carcinoma that originated from any component of the nail unit, which comprises the nail bed, nail matrix, nail groove, nail fold, and periungual skin. Functional surgery included Mohs micrographic surgery, wide surgical excision, local surgical excision, as well as other functional surgical modalities. Results were defined as metastasis, death, local recurrence, or persistent disease as described by the studies. Disease was classified as persistent when positive margins were reported after treatment. Squamous cell carcinomas growing at other sites of the body and articles that did not differentiate between nSCC and other tumours of the nail apparatus were excluded. Repeated publications, as well as studies in which data relevant to our interests could not be extracted, were removed [Table 1].
| Parameters | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Participants | Studies include a minimum of 5 subjects who were diagnosed with localised/invasive nSCC through histopathology. |
1. Studies without histopathology confirming nSCC. 2. Data on nSCC in studies are reported as part of the overall data and cannot be isolated. |
| Interventions | Articles reporting functional surgery or amputation at any level. |
1. There are no precise details of surgical techniques. 2. Participants who did not have prior therapy or had a combination of treatments were indistinguishable from the whole sample. |
| Comparators | None | None |
| Outcomes | Any local recurrence, metastasis, or related death. |
1. Studies lacking information on recurrence. 2. Results by stage & operational procedures were unable to be isolated from the overall dataset. |
| Time | Average follow-up time of more than 6 months | Average follow-up time less than 6 months |
| Setting | Any setting | None |
| Study designs | Any study design | Review articles, letters to editors, comments, posters, abstracts only, meeting reports. |
nSCC: nail squamous cell carcinoma.
Procedures for searching the literature
We conducted a comprehensive search strategy following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) and MOOSE (Meta-analyses Of Observational Studies in Epidemiology) guidelines. A search of the literature was carried out using Pubmed, Embase, Cochrane Library, Web of Science, and Scopus from inception until February 23, 2023. The search terms used in these databases were “nail” / “nail unit” / “subungual” / “ungual” and “squamous cell carcinoma” / “epidermoid carcinoma” and “Mohs surgery” / “wide excision” / “amputation” / “local excision” / “functional” / “treatment” / “surgery” / “en bloc excision” and “recurrence” / “death” / “metastasis” / “survival.”
Study selection
The preliminary retrieved results were transferred from each database into Endnote. The results were then combined, and repetitions were discarded. The retrieved papers’ titles, abstracts, as well as publication types, were reviewed to determine whether to include them during the complete text evaluation. Articles that were not in English and non-human studies were excluded. We also excluded studies that did not focus on nSCC, as well as publications with unsuitable designs, which included review articles, commentaries, letters, and those with abstracts only.
Data extraction process
Three investigators (HS.W., F. L., and JY.J.) independently reviewed the titles and abstracts of the included publications before evaluating the complete articles for eligibility [Figure 1]. Following inclusion, the three authors (HS.W., F.L. and SD.H.) independently retrieved data on the treatment method, recurrence, and follow-up duration. Any disagreements were handled via a consensus meeting with the third investigator (DG.W.). Following inclusion, information gathered from every article was retrieved and subcategorized, encompassing the year of publication, period, number of patients, age, gender distribution, tumour stage, kind of intervention, number of recurrences, and follow-up duration.
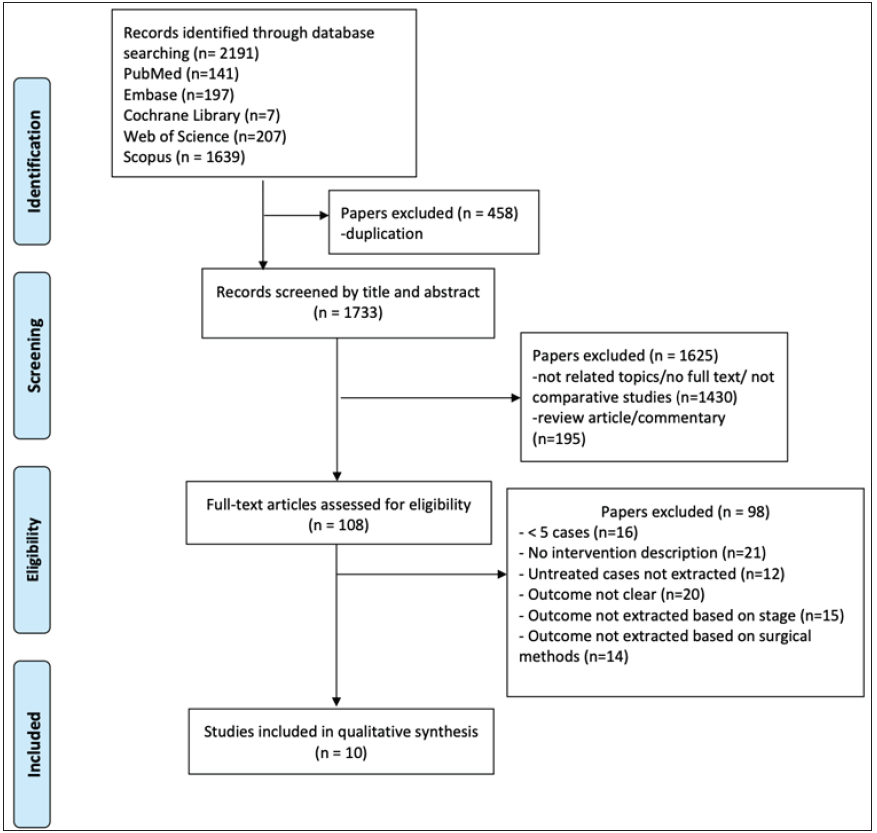
- PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart of study selection.
Risk of bias and quality assessment
The risk of a bias assessment tool for non randomised studies (RoBANS) was applied to evaluate the bias of the 10 included studies.2 As all 10 studies were retrospective and non randomised in nature, we preferred using the RoBANS tool which is designed for non randomised studies. This tool is comprised of six domains: the selection of participants, confounding variables, measurement of exposure, blinding of the outcome, incomplete outcome data, and selective reporting.
Results
Literature search and study characteristics
Figure 1 shows the systematic search procedure step by step. From a total of 2191 studies retrieved from 5 databases, we finally included 10 studies with a total of 319 lesions [Table 2]. All the included studies were non randomised and published between 1992 and 2020. Seven were retrospective studies and three were case series. Three studies came from the United States, five from Europe, and one from each Asia and Australia.3-12 All 10 investigations described the clinical and pathological characteristics of nSCC, with subungual hyperkeratosis being the most frequently reported presentation. Nail squamous cell carcinoma was suspected in about 38 cases before definite diagnosis and the remaining patients were often misdiagnosed and managed as onychomycosis and viral warts.4-6,12 Functional surgery was more commonly reported than amputation, with Mohs micrographic surgery being the most reported surgical modality. The number of studies was inadequate for comparing their outcomes based on each surgical modality.
| Article | Study Type | N | Mean Age (Range), years |
Sex F/M |
Location, Hand/Foot | Mean Time to Diagnosis (Range), mo. | Staging | Treatment Modality (N) | Mean Follow-up (Range), mo. | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| Goldminz et al., 1992, USA3 | Case series | 25 | 61 (19–94) | NR | NR | 60 (3–180) | 2is, 23I | MMS (25) | 60 (12–144) | 2/25->MMS |
| Dalle et al., 2007, France4 | Retrospective | 35 | NR (25–85) | 10/25 | 28/7 | NR (2–84) | 4is, 31I |
LSE (9) WSE (20) DA (6) |
33 (4–90) |
5/9 ->WSE 1/20 ->LSE 1/6->DA->died |
| Young et al., 2012, Australia5 | Case series | 12 (13nSCC) | 49 (32–75) | 4/8 | 13/0 | 57(18–168) | 11is, 2I | MMS (13) | 51.5 (2–120) |
1->MMS->Topical imiquimod->MMS 1->DA 1->MMS |
| Lecerf et al., 2013, Belgium6 | Retrospective | 25 (27nSCC) | 60 (21–80) | 7/18 | 26/1 | NR | 11is, 16I |
DA (2) Partial ablation (3) En bloc ablation (14) LECM (8) |
40 (4–177) |
1/2 ->NR 0/3 5/14 ->NR 2/8 ->NR |
| Wollina et al., 2015, Germany7 | Case series | 8 (9nSCC) | 60 (40–84) | 2/6 | 6/3 | 9 (NR) | 9is, 0I | MMS (9) | NR (48–60) | 2->MMS |
| Dika et al., 2015, Italy8 | Retrospective | 57 | 63 (26–89) | 18/39 | 49/8 | 30 (NR) | 7is, 50I |
MMS (43) DA (12) |
NR |
2/43->DA 0/12 |
| Tang et al., 2016, USA9 | Retrospective | 33 (39 nSCC) | 63 (33–92) | 7/26 | 36/3 | 39 (3–360) | NR |
DA (3) MMS (35) WSE (1) |
NR (5–48) |
0/3 3/35->MMS, radiotherapy, DA 0/1 |
| Topin-Ruiz et al., 2017, France10 | Retrospective | 55 | 64 (35–90) | 23/32 | 39/16 | 34 (2–182) | 6is, 49I | WSE (55) | 78 (60–134) |
1->WSE 1->WSE->DA |
| Lee et al., 2019, Korea11 | Retrospective | 17 | 61 (36–80) | 5/12 | 12/5 | 62 (4–264) |
4is, 13I |
MMS (8) LSE (4) WSE (1) DA (4) |
31 (5–75) |
0/8 2/4->LSE, NM 0/1 0/4 |
| Gou et al., 2020, USA12 | Retrospective | 40 (42 nSCC) | 61 (33–92) | 6/34 | 38/4 | 24 (1–240) | 24is,18I |
MMS (38) MMS->DA (4) |
45 (3–144) |
3/38->MMS 0/4 |
Note: N, number of cases; F, female; M, male; mo., months; NR, unreported or unextractable; LSE, limited surgical excision; WSE, wide surgical excision; DA, digital amputation; LECM, limited excision until clearing of margins; is, in situ; I, invasive; nSCC, nail unit squamous cell carcinoma; MMS, Mohs micrographic surgery.
In total, all studies included 282 individuals, 82 females, and 200 males. The average age of these patients was 60 years. The duration from the discovery of the lesions to the diagnosis of nSCC ranged from 1 to 360 months. Most (247 lesions) were on the hand, and 47 lesions were on the foot. More than one digit were affected simultaneously in 4 cases. Two of these had 3 digits affected, while the other two had 2 digits affected.5-7,12 One of them was reported to have xeroderma pigmentosum.12 While 78 lesions were reported to be in situ and 202 were invasive, 1 study did not specify the degree of invasiveness.9 Only 1 study reported distant metastasis and death.4 The duration for post-surgical follow-up ranged from 2 to 177 months. There was a 12% overall recurrence rate, with a total of 34 recurrent cases. Post-surgical outcomes for each surgical modality were described.
Risk of bias
The risk of bias assessed by RoBANS indicates that all 10 articles have an overall low risk of bias. The section on incomplete outcome data was reported high for the study by Lecerf et al. because they did not describe the mean time to diagnosis. The confounding variable was rated high in the study by Topin-Ruiz et al. due to a preference of surgical modality [Table 3].10
| Study | Selection of participants | Confounding variables | Measurement of exposure | Blinding of outcome | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Goldminz et al., 1992, USA3 | Low | Low | Low | Low | Low | Low |
| Dalle et al., 2007, France4 | Low | Low | Low | Low | Low | Low |
| Young et al., 2012, Australia5 | Low | Low | Low | Low | Low | Low |
| Lecerf et al., 2013, Belgium6 | Low | Low | Low | Low | High | Low |
| Wollina et al., 2015, Germany7 | Low | Low | Low | Low | Low | Low |
| Dika et al, 2015, Italy8 | Low | Low | Low | Low | Low | Low |
| Tang et al., 2016, USA9 | Low | Low | Low | Low | Low | Low |
| Topin-Ruiz et al., 2017, France10 | Low | High | Low | Low | Low | Low |
| Lee et al, 2019, Korea11 | Low | Low | Low | Low | Low | Low |
| Gou et al, 2020, USA12 | Low | Low | Low | Low | Low | Low |
Treatment based on surgical modality
Mohs micrographic surgery
A total of 171 nSCC lesions from 7 studies were treated by Mohs micrographic surgery [Table 4].3,5,7-9,11,12 Among these lesions, 49 lesions were in situ cases, and 48 lesions were invasive nSCC. Invasiveness for the remaining lesions could not be extracted from the whole data for 2 studies.8,9 A majority of the lesions affected the fingernails. Fifteen cases recurred, resulting in an overall reported recurrence rate of 9%. The mean duration for the recurrence of disease after Mohs micrographic surgery was 39 months. Among the recurrent cases with reported pathology, 4 cases were reported to recur as in situ nSCC, while 1 as invasive nSCC.5,7 The remaining studies did not describe the type of recurrence. Ten of the recurrent cases were treated with repeated Mohs micrographic surgery, 4 underwent amputation, and 1 underwent radiotherapy. One of the persistent (positive margins reported after treatment) cases recurred after Mohs micrographic surgery and topical imiquimod, which was later cleared after a third intervention by Mohs micrographic surgery. Meanwhile, a study treating 1 in situ and 7 invasive cases with Mohs micrographic surgery did not report any recurrences.11 None of the cases metastasized. However, the periosteal invasion was discovered in 9 cases during Mohs micrographic surgery, where 4 underwent amputation, and the remaining 5 were treated with curettage of the periosteum and close follow-up.8,12
| Article | In situ/ Invasive | Location | Treatment Modality (N) [MMS Stages] | Defect reconstruction | Recurrences | Time to recurrence (months) |
|---|---|---|---|---|---|---|
| Goldminz et al., 1992, USA3 |
is (2) I (23) |
NR | MMS (25) [NR] | SIH (25) | 2/25-> MMS | 12; 132 |
| Young et al., 2012, Australia5 |
Is (11) I (2) |
R1H (3) R3H (3) R4H (1) L2H (2) L3H (2) L4H (1) L5H (1) |
MMS (13) [1–3, mean two] |
SIH (12) primary closure (1) |
1->MMS->Topical imiquimod->MMS 1->DA 1->MMS |
13; 30; 96 |
| Wollina et al., 2015, Germany7 | is (9) | R4H (1) R2H (1) R3 (2) R5 (1) L1F (1), L5F (1) 2 NR | MMS (9) |
5STSG 3FTSG 1SIH |
2->MMS | 24; 36 |
| Dika et al., 2015, Italy8 | NR | 1st fingernail |
MMS (43) [1–4, mean, 3.2] |
Hyalofill-F+SIH | 2/43->DA | 12, 18 months |
| Tang et al., 2016, USA9 | NR |
Fingernails R3 most common |
MMS (35) | NR |
3/35->1 MMS 1->radiotherapy 1->DA |
NR |
| Lee et al., 2019, Korea11 |
is (1) I (7) |
R1H (2) R2H(1) R4H(2) L1H (1) L3F (1) R5F (1) |
MMS (8) | NR | 0/8 | 0 |
| Gou et al., 2020, USA12 |
is (26) I (16) |
H (38/42) |
MMS (38) MMS->DA (4) [1–4, mean 1.8] |
19 FTSG, 10SIH, 3STSG, 4 DA, 1nail bed graft, 1NR (2 patients had extensive and continued tobacco use, and the other 2 had exposure of the periosteum.) |
3/38->MMS 0/4 |
5; 8; 79 |
is: in situ; I: invasive; R: right; L: left; H: hand; F: feet; NR: not reported; WSE: wide surgical excision; DA: digital amputation; FTSG: full-thickness skin graft; SIH: secondary intention healing; MMS: Mohs micrographic surgery; STSG: split-thickness skin graft
Following Mohs micrographic surgery, 30 cases were closed by skin grafts, 1 by primary closure, 91 by secondary intention healing, and 1 by splint nail bed graft. Four cases further underwent phalanx amputation because of prolonged smoking history and periosteum exposure.12 Reconstruction data were unavailable for 44 lesions. Of the skin grafts, 22 were full-thickness skin grafts (FTSG) and 8 were split-thickness skin grafts (STSG). In one study the defects were repaired with hyaluronic acid followed by secondary intention healing; 60% of these patients reported subsequent nail dystrophy.8 The number of stages required for histological clearance was described in 3 studies, with an average of 2 stages, ranging from one to four stages of Mohs micrographic surgery.5,8,12 Only 1 study described the number of tissue sections required, with an average of 4 sections.5 One study reported discovering 5 cases of periosteal invasion during Mohs micrographic surgery although X-rays did not show any abnormalities.8 Post-surgical cosmetic and functional evaluations after Mohs micrographic surgery were reported in 1 study, with an overall high satisfaction rate.5 Dysesthesia was reported in 3 cases as the most common late complication in another study.12
Wide surgical excision
Five studies evaluated the outcome of wide surgical excision for nSCC not involving the bone, representing 91 lesions [Table 5].4,6,9-11 The fingernails were the most common site affected. Depth of invasion was described in 4 studies, with 14 in situ cases and 74 invasive cases. Two cases were described as microinvasive because of the difficulty in determining tumour cells invasion of the papillary dermis.6 One report used the term ‘en bloc ablation’, which specified the excision of a nail unit with 6-mm margins.6 This study also included a case of polydactylous nSCC which affected 3 digits simultaneously.
| Article | In situ/ Invasive | Location | Treatment Modality (N) | Defect reconstruction | Recurrences | Time to recurrence (months) |
|---|---|---|---|---|---|---|
| Dalle et al., 2007, France4 |
is (3) I (17) |
R1H(7) R2H(2) R4H(2) L1H(3) L2H(2) L5H(1) R1F(2) L1F(1) |
WSE (20) | FTSG (20) | 1/20 ->LSE | 36 |
| Lecerf et al., 2013, Belgium6 |
is (5) Microinvasive (2) I (7) |
R1H(2) R2H(2) R3H(1) R4H(3) L1H(1) L2H(2) L3H(1) L5H(1) R1F(1) |
En bloc ablation with 6-mm margins (14) | NR | 5/14 ->NR | 36; 58; 58; 46; 8 |
| Tang et al., 2016, USA9 | NR | NR | WSE (1) | NR | 0/1 | |
| Topin-Ruiz et al., 2017, France10 |
is (6) I (49) |
L1H(12) R1H(11) R1F(8) |
WSE (55) | FTSG (55) |
2/55 1->WSE 1->WSE ->5 months ->DA |
7; 8 |
| Lee et al., 2019, Korea11 | I (1) | L1H (1) | WSE (1) | NR | 0/1 |
is: in situ; I: invasive; R: right; L: left; H: hand; F: feet; NR: not reported; WSE: wide surgical excision; DA: digital amputation; FTSG: full-thickness skin graft
In two studies FTSG was performed after wide surgical excision, while the other 3 studies did not mention the reconstruction method.4,10 There was a 9% recurrence rate following wide surgical excision, with 8 cases recurring after an average of 32 months after the first surgery.4,6,10 Six of these cases had clear histological margins reported after the initial surgery, 1 did not have clear margins, and margins were not mentioned in 1 case. Five of the recurrent cases were invasive nSCC, 1 was microinvasive, and 2 were in situ nSCC. One of the relapses occurred adjacent to the graft and was treated with local surgical excision.4 Another 2 recurrent cases were further treated by wide surgical excision, in which 1 persistent disease later underwent amputation.10 One study did not mention the treatment after recurrence.6 Post-surgical patient satisfaction was assessed only in 1 study, with overall high satisfaction.10
Digital amputation
A total of 6 studies with 31 cases reported amputation performed [Table 6].4,6,8,9,11,12 Two of the cases were in situ nSCC, while 14 were invasive, and one study did not describe invasiveness.9 Fingernails were the most common site. Six cases were reported as partial amputation, whereas 4 cases were initial Mohs micrographic surgery cases that failed to obtain clear margins.4,12 Recurrences were seen in 2 cases of amputation, with a recurrence rate of 6%.4,6 One of the patients died after metastasis to the lungs. This was an in situ nSCC that recurred at the stub 2 months after initial partial amputation and the patient subsequently underwent complete amputation.4 Another case recurred 19 months later but the treatment for recurrence was not described.6 Amputations were usually performed in bone-invasive cases that were evidenced from radiology, however, 2 cases of amputation were performed because of patient preference and treatment convenience.6
| Article | In situ/ Invasive | Location | Treatment Modality (N) | Recurrences | Time to recurrence (months) |
|---|---|---|---|---|---|
| Dalle et al., 2007, France4 |
is (1) I (5) |
R1H(1); R4H(1); L1H(1); L2H(1); L3H(1); L1F(1) | DA (6) | 1/6->DA->died | 2 |
| Lecerf et al., 2013, Belgium6 |
is (1) I (1) |
R2H(1) L2H(1) |
DA (2) | 1/2 ->NR | 19 |
| Dika et al., 2015, Italy8 | NR | NR | DA (12) | 0/12 | NR |
| Tang et al., 2016, USA9 | NR | NR | DA (3) | 0/3 | |
| Lee et al., 2019, Korea11 | I (4) | L1H(1); L4H(1); R5F(2) | DA (4) | 0/4 | |
| Gou et al., 2020, USA12 | NR | NR | MMS->DA (4) | 0/4 |
is: in situ; I: invasive; R: right; L: left; H: hand; F: feet; NR: not reported; DA: digital amputation; MMS: Mohs micrographic surgery
Other surgical modalities
Three studies described three alternative methods of functional surgery that cannot be included in wide surgical excision or Mohs micrographic surgery [Table 7].4,6,11 Eight cases with in situ nSCC were treated by limited excision until clearing of margins (LECM). The authors described the complete excision of the defect and obtaining clear margins by evaluating the lateral and deep margins.6 Two of the cases after LECM recurred after 19 and 14 months after clear marginal excision, further treatment was not described. Partial ablation was described in 3 cases, and no recurrences were reported.6 Seven of the 13 cases that were treated by local surgical excision relapsed after an average of 17 months, giving a recurrence rate of 54%.4,11 Five of the cases underwent wide surgical excision, 1 repeated local surgical excision, and 1 was not reported.
| Article | In situ/ Invasive | Location | Treatment Modality (N) | Recurrences | Time to recurrence (months) |
|---|---|---|---|---|---|
| Lecerf et al., 2013, Belgium6 |
LECM: is (5) I (3) Partial ablation: I (3) |
LECM: R3H(2); R4H(1); L1H(2); L2H(2); L3H(1) Partial ablation: R1H(1); R3H(1); L1H(1) |
LECM (8) Partial ablation (3) |
2/8 ->NR 0/3 |
14 19 |
| Dalle et al., 2007, France4 | I (9) | R1H(1); R2H(1); R3H(1); L1H(2); L3H(1); L5H(1); R1F(1); L1F(1) | LSE (9) | 5/9 ->WSE | 6; 36; 6; 16; 7 |
| Lee et al., 2019, Korea11 |
is (3) I (1) |
R5H(1); L2H(1); L3H(1); R1F(1) | LSE (4) | 2/4->1 LSE, 1 NR | 43; 4 |
LECM: limited excision until clearance of margin; NR: not reported; is: in situ; I: invasive; R: right; L: left; H: hand; F: feet; WSE: wide surgical excision; LSE: limited surgical excision
Discussion
The nail apparatus has a rather complex anatomical structure. A good understanding of its structure is required to diagnose and manage entities involving this organ. Malignant nail tumours are typically rare with nSCC being the most common carcinoma reported. When nSCC is present, the nail unit might appear in a variety of clinical presentations. Despite being the most prevalent malignant subungual tumour, nSCC is frequently misdiagnosed as an innocuous condition like onychomycosis, verruca vulgaris, or trauma-induced nail dystrophy.13 Middle-aged males are more likely to be affected, and the hand is the most commonly reported area.4 A high level of suspicion is therefore required when addressing a nail condition to avoid a delay in diagnosis, which may complicate therapy and significantly affect the prognosis. While metastasis and mortality are uncommon in nSCC, early biopsies of chronic non-healing and persistent lesions may merit a better prognosis.4 Clinicians in practice should therefore be aware of benign-presenting nail lesions that do not improve with appropriate management and should suggest that patients undergo nail biopsies when applicable.
Functional procedures, such as Mohs micrographic surgery and wide surgical excision, were routinely tested to establish the best first-line treatment for nSCC. However, the existing research does not recommend a specific therapeutic strategy as the first line of therapy. Studies conducted over the last decade have shown that more conservative approaches for nSCC management are preferable to traditional amputation. These authors believe that traditional amputations may result in functional problems, undesirable cosmetic results, and possibly psychological distress. This is particularly noticeable in the amputation of the thumb, which accounts for about 40% of the hand’s normal function.14 Further, the patient may experience loss of sensation at the amputated site, unusual pains, excessive sensitivity, and difficulties when gripping small items, which may interfere with daily tasks.8,15
Mohs micrographic surgery has the advantage of eliminating the tumour with histological confirmation of the actual extent of malignancy, as well as removing the diseased tissue while preserving its normal structure.3,12,16 Preserving the viable tissues of the finger to the greatest extent feasible is critical for a functioning digit.8 However, imaging methods typically fail to detect the depth of nSCC invasion. Mohs micrographic surgery can detect periosteal invasion and accurately differentiate bone invasion from inflammation or compression.8,12 In general, Mohs micrographic surgery is an outstanding option for tumour removal, but it is somewhat more complicated and demanding, it also requires a skilled and certified Mohs surgeon.17
Because Mohs micrographic surgery is too difficult to perform on the nail apparatus due to its unique anatomical structure, a few studies have highlighted the utility of the wide surgical excision method for nSCC.4,6,10,15 Flores et al. discovered that wide surgical excision with a margin of 5 mm was correlated with a reduced recurrence rate and gave greater functional and aesthetic advantages than amputation.15 Surgical wounds may be left to heal by secondary intention, or with fillers, full-thickness skin grafts or skin flaps, and all have favourable outcomes.10,18 Surgical procedures for wide surgical excision are more time-efficient and have been correlated with high patient satisfaction, successful recovery, and effective local disease control.15 On the other hand, wide surgical excision removes more viable tissues, causing poor functional and aesthetic outcomes for smaller tumours where the nail unit might potentially be partially retained.11 The extent of the tumour generally remains unknown until the procedure is completed; hence, the margin of resection as well as the best time to do reconstruction are uncertain. Nevertheless, late recurrence of nSCC is frequent after both types of surgical procedures which had completely removed the carcinoma.6
Consistent with previous studies, this review also showed a male predominance around the age of 60. Lesions were mainly on fingernails. Our systematic review shows that functional surgery of the nail unit is an effective alternative to amputation in nSCC that does not involve the bone. In this study, we included Mohs micrographic surgery, wide surgical excision, and local surgical excision in our understanding of functional surgery. Unlike Mohs micrographic surgery and wide surgical excision, local surgical excision has a relatively high recurrence rate.4,11 This could be a result of tumour clearance being insufficient. As such, we do not think it is a desirable treatment for nSCC lesions because it only removes the portion of the tumour observable by the naked eye.4,11
Regardless of the surgical type, attaining histological clearance should be the gold standard of treatment for nSCC, whether it involves the bone or not. To achieve complete excision, a thorough histologic assessment of the surgical margins is required in all instances. In our opinion, efficient treatment is determined by the total elimination of the tumour rather than by an aggressive surgical approach. Simultaneously, the surgical technique should be sufficient to ensure total tumour excision while preserving the normal function of the finger or toe. This suggests that wide surgical excision and Mohs micrographic surgery should be desirable options for a significant number of nSCC patients since both have been associated with low recurrence rates.17 Further prospective studies comparing these two techniques are necessary to determine whether Mohs micrographic surgery or wide surgical excision is the preferable intervention for nSCC that does not involve the bone.
Limitations
There are several drawbacks in this review. First, only retrospective observational studies were evaluated in this analysis; hence, there may be missing data such as those caused by recall bias. Second, the number of studies may be too small for a meta-analysis. Third, the follow-up period in the recruited studies was modest, perhaps underestimating the probability of recurrence of this slow-growing neoplasm. Because of the distinctive nail structure and the associated difficulty in achieving clear surgical margins, functional surgery is more complicated than amputation. As a result, surgeons with minimal nail surgery experience may be limited in their use of functional surgery. Despite these limitations, given the rarity of nSCC and the lack of controlled trials, this review might be informative for clinicians who are treating patients with this carcinoma, and may help in planning bigger trials.
Conclusion
There is no consensus on the surgical management of nSCC that does not involve the bone. The recurrence rates of functional surgery and amputation do not differ significantly, as seen in our review. To reduce severe functional limitations and psychological discomfort following amputation, functional surgery should be considered as a first-line therapy for those without bone involvement. When functional surgery fails to establish clean margins, amputation should be considered as a last option. To date, only small cohorts or case reports dealing with this nail neoplasm have been published. Further research comparing these two procedures with large sample sizes is required to give firm evidence on whether Mohs micrographic surgery or wide surgical excision is a better surgical alternative.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408-14.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs micrographic surgery of the nail unit. J Dermatol Surg Oncol. 1992;18:721-6.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma of the nail apparatus: Clinicopathological study of 35 cases. Br J Dermatol. 2007;156:871-4.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs’ micrographic surgery as treatment for squamous dysplasia of the nail unit. Australas J Dermatol. 2012;53:123-7.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermato. 2013;69:253-U199.
- [CrossRef] [PubMed] [Google Scholar]
- Bowen’s disease of the nail apparatus: A series of 8 patients and a literature review. Wien Med Wochenschr. 2015;165:401-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs surgery for squamous cell carcinoma of the nail unit: 10 years of experience. Dermatol Surg. 2015;41:1015-9.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study of nail squamous cell carcinoma at 2 institutions. Dermatol Surg. 2016;42:S8-S17.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of subungual squamous cell carcinoma by wide excision of the nail unit and skin graft reconstruction an evaluation of treatment efficiency and outcomes. JAMA Dermatol. 2017;153:442-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Squamous cell carcinoma of the nail unit: A retrospective review of 19 cases in Asia and comparative review of western literature. Int J Dermatol. 2019;58:428-32.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs micrographic surgery as the standard of care for nail unit squamous cell carcinoma. Dermatol Surg. 2020;46:725-32.
- [CrossRef] [PubMed] [Google Scholar]
- Subungual squamous cell carcinoma masquerading as chronic common infection. J Med Assoc Thai. 2010;93:248-51.
- [PubMed] [Google Scholar]
- Anatomy, physiology, and functional restoration of the thumb. Ann PlastSurg. 1996;36:180-91.
- [CrossRef] [PubMed] [Google Scholar]
- Functional surgery for malignant subungual tumors: A case series and literature review. Actas Dermosifiliogr (Engl Ed). 2018;109:712-21.
- [CrossRef] [PubMed] [Google Scholar]
- Micrographic surgery for subungual squamous cell carcinoma. Br J PlastSurg. 1996;49:414-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment options and outcomes for squamous cell carcinoma of the nail unit: A systematic review. Dermatol Surg. 2022;48:267-73.
- [CrossRef] [PubMed] [Google Scholar]
- Full-thickness skin graft after nail complex resection for malignant tumors. Tech Hand Up Extrem Surg. 2011;15:84-6.
- [CrossRef] [PubMed] [Google Scholar]






