Translate this page into:
Cutaneous angiosarcoma presenting as erythematous plaques and diffuse facial swelling in an elderly man
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma A, Vinay K, Parsad D, GY S, Chatterjee D. Cutaneous angiosarcoma presenting as erythematous plaques and diffuse facial swelling in an elderly man. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_439_2024
Dear Editor,
A 63-year-old previously healthy man presented for evaluation of diffuse facial swelling of 2 months duration. Cutaneous examination revealed multiple areas of ill-defined, irregularly shaped, skin coloured to erythematous plaques over the forehead and a diffuse swelling of the lower half of face [Figure 1a]. There was a noticeable droop on the right side of face which on further evaluation revealed right-sided facial nerve palsy. There was no ulceration in any of the lesions. Dermoscopic examination showed presence of surface scaling, erythematous areas of varying tones and polymorphic vessels including linear, irregular, hairpin and arborising vessels [Figure 1b]. Based on clinical and dermoscopic features, differential diagnoses considered were cutaneous angiosarcoma, intravascular B-cell lymphoma (IVBCL), Kimura disease and diffuse dermal angiomatosis (DDA). Histopathological examination of lesion on the forehead as well as cheek revealed an invasive tumour arranged in nodules, nests and fascicles. Tumour cells were seen lining the irregularly shaped vascular channels. There were foci showing definitive vasoformation by the tumour cells. Overall features were suggestive of cutaneous angiosarcoma (cAS) [Figures 2a and 2b]. The individual tumour cells were pleomorphic, polygonal to fusiform with round to oval nuclei, coarsely granular chromatin, prominen nucleoli and moderate cytoplasm. Prominent mitotic figures were noted. Immunohistochemistry (IHC) demonstrated positive staining for endothelial markers such as CD31 and CD34 [Figures 2c and 2d]. 18-Fluoro-deoxyglucose positron emission tomography (FDG-PET) scan revealed FDG avid diffuse cutaneous and subcutaneous thickening in scalp and face. Low-grade FDG avid subcentimetric to maximum size of 2.2 cm (necrotic), bilateral intraparotid, left level IB and right level II cervical lymph nodes were also seen. Patient was then started on paclitaxel chemotherapy and remains under follow-up.
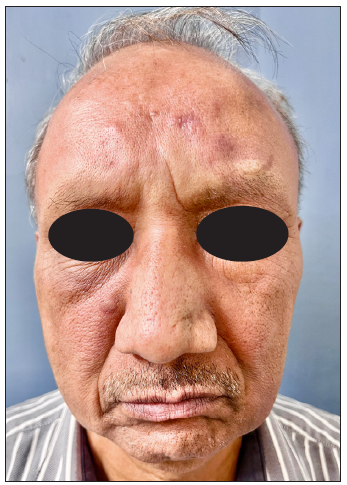
- Multiple areas of ill-defined, irregularly shaped, skin coloured to erythematous plaques over the forehead and a diffuse swelling of the face, more prominent over the lower half.
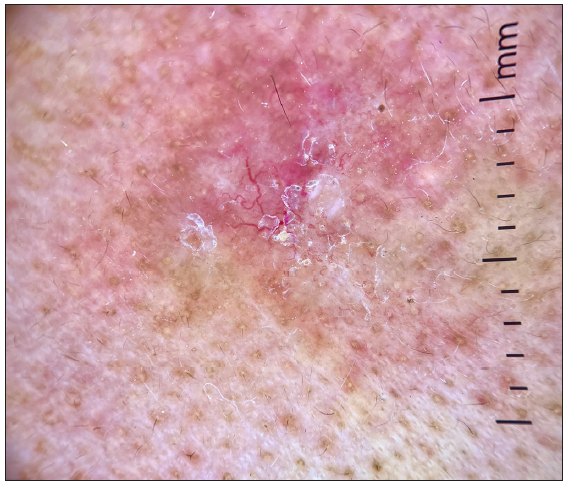
- Dermoscopic examination showed the presence of surface scaling, erythematous areas of varying tones and polymorphic vessel structures including linear, irregular, hairpin and arborising vessels (DermLite DL 4, ×10, polarised).
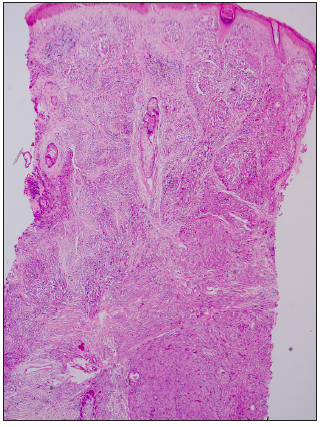
- Microphotograph showing an invasive tumour arranged in nodules, nests and fascicles. (Haematoxylin and Eosin, 40×).
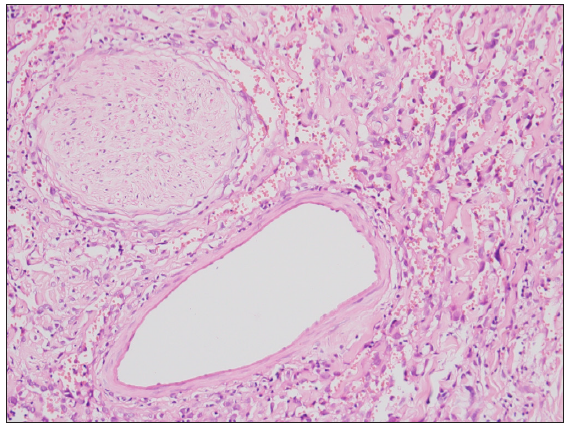
- Microphotographs displaying atypical vascular proliferation and notable mitotic activity, enlarged slit-like spaces with an abundance of RBCs and atypical cells (Haematoxylin and Eosin, 200×).
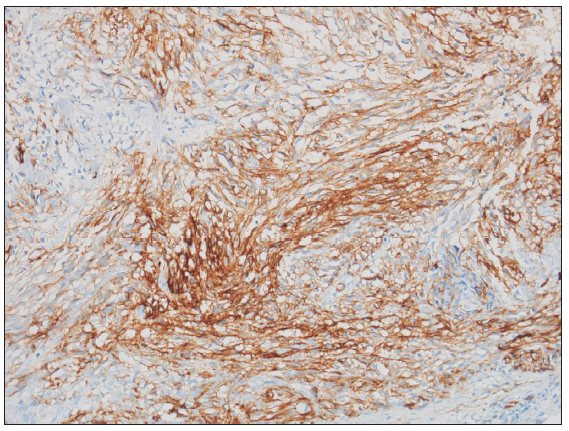
- Immunohistochemical analysis showing positive endothelial marker CD31 staining (200x).
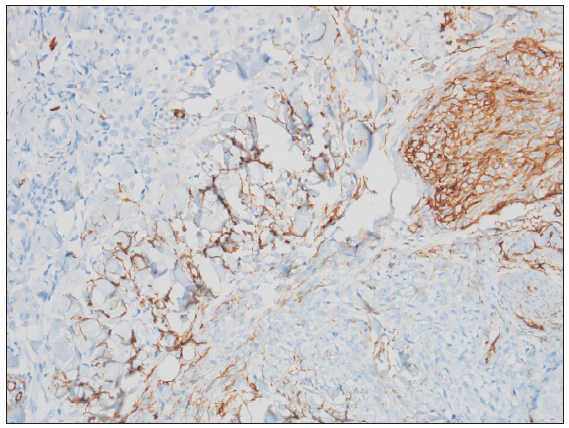
- Immunohistochemical (IHC) analysis showing positive CD34 staining (200x).
Angiosarcoma (AS) is a rare malignant endothelial cell tumour which primarily manifests in the skin, soft tissues and viscera. cAS mainly occurs in three scenarios: idiopathic, on the face, scalp and neck; associated with chronic lymphedema; post-radiation exposure. The first scenario usually affects males in the seventh to eighth decade. Clinical presentation involves localised/extensive, infiltrative, confluent purple-black/bruise-like lesions on the face, head and frontal area.1,2 As the tumours grow, oedema becomes a pertinent feature. Ambujam et al.3 reported an uncommon clinical presentation resembling a hematoma in a fast spreading, extensive AS in a dark-skinned individual. There can also be associated symptoms of nerve palsy as was seen in the present case due to infiltration of the facial nerves. AS is frequently misdiagnosed as fungal and bacterial infections, Kaposi’s sarcomas, melanomas or ulcers, leading to delay in diagnosis. On dermoscopy, AS is characterised by a combination of typical colours in vascular lesions – red, purple and blue as well as linear telangiectasias. There is hence a need for keeping a high index of suspicion, a low threshold for biopsy and need for multiple scouting biopsies for diagnosis. Importantly, in IHC, not all markers must be positive; therefore, panel diagnostics are required. Positivity rates of markers are variable; Factor VIII in 83%, CD31 in 80%, CD34 in 63% and D2-40 in 43% cases.4
IVBCL is a very close differential. This rare type of lymphoma primarily involves blood vessels, often presenting with non-specific systemic symptoms. In the skin, IVBCL manifests as violaceous papules or nodules. Histologically, it shows neoplastic lymphoid cells confined within the blood vessel lumina. IHC reveals B-cell markers such as CD20 and CD79a, none of which were seen in our patient.
Kimura disease is characterised by painless subcutaneous nodules, lymphadenopathy and peripheral eosinophilia. Unlike angiosarcoma, Kimura disease typically spares the vasculature with lymphoid follicles, eosinophilic infiltrates and fibrosis seen on histology.
Diffuse dermal angiomatosis (DDA) involves proliferation of small blood vessels within the dermis, leading to erythematous plaques or nodules. Unlike cAS, DDA lacks significant cellular atypia and shows a diffuse proliferation of capillaries without a malignant vascular component.
The pathophysiology of AS is interwoven with genetic aberrations involving TP53 mutations, environmental influences and unpredictable clinical behaviours. While wide-field radiation therapy and total surgical resection have been established as the standard of care for smaller sized and limited extent angiosarcoma, older age and comorbidities call for a safe and efficient adjuvant treatment. Data on the use and efficacy of immunotherapy (immune check-point inhibitors in particular) in cAS are limited, and biomarkers suggest a promising advancement in future treatment options.5
Our case contributes novel findings to the existing literature by documenting an unusual presentation of AS. The need for heightened clinical acumen and a low threshold for biopsy in atypical cases become apparent, underscoring the necessity for continual refinement of diagnostic algorithms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cutaneous angiosarcoma: Report of three different and typical cases admitted in a unique dermatology clinic. An Bras Dermatol. 2017;92:235-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous angiosarcoma presenting as an unusual facial bruise. Age Ageing. 2004;33:512-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma of the head, neck, and face of the elderly in type 5 skin. J Cutan Aesthet Surg. 2013;6:45-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- S1-Guideline cutaneous angiosarcomas - Update 2021. J Dtsch Dermatol Ges. 2021;19:1801-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma: A review of current evidence for treatment with checkpoint inhibitors. Front Med (Lausanne). 2023;10:1090168.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





