Translate this page into:
Post pemphigus acanthomata: Revisiting an uncommon presentation of pemphigus
Corresponding author: Dr. Divya Gupta, Department of Dermatology, Dr BR Ambedkar Medical College, Gandhinagar, KG Halli, Bengaluru, India. divya_gupta@ymail.com
-
Received: ,
Accepted: ,
How to cite this article: Adithyan P, Loganathan E, Padmanabha SR, Somashekhar S, Reddy JK, Gupta D. Post pemphigus acanthomata: Revisiting an uncommon presentation of pemphigus. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_664_2024
Dear Editor,
Pemphigus refers to a group of vesiculobullous disorders characterised by the presence of multiple fluid-filled lesions affecting the skin and mucosae. After rupturing, they usually heal with hyper- or hypopigmentation.1 In some cases, verrucous lesions develop at sites of previously healed blisters, this phenomenon is called post pemphigus acanthomata (PPA).2
A 22-year-old male patient visited the dermatology outpatient department 12 months ago with complaints of multiple crusted erosions with some fluid-filled flaccid bullae over the face and trunk. Skin biopsy and direct immunofluorescence suggested pemphigus foliaceus. The serum tested positive for anti-desmoglein 1 antibody (anti dsg 1 titres = 184 U/mL). We initiated treatment with dexamethasone pulse therapy along with weekly methotrexate, which effectively controlled the disease. However, after the fourth cycle, he noticed dark elevated lesions over the site of previous erosions along with the reappearance of new superficial blisters. Cutaneous examination revealed multiple hyperpigmented verrucous plaques over the chest, abdomen, back and proximal limbs. Moist erosions with perilesional erythema and positive perilesional Nikolsky sign were seen over the face and trunk [Figures 1a-1c]. There were no other complaints and the general physical examination was unremarkable. Laboratory investigations including haematology and biochemistry panels were within normal limits. Histopathological examination of the verrucous plaque revealed hyperplastic squamous epithelium exhibiting loose hyperkeratosis, acanthosis, papillomatosis and sub-corneal blister formation with acantholytic cells suggestive of post pemphigus acanthomata [Figure 2]. Anti desmoglein-1 antibody titres were elevated [95 U/mL] which indicated a possible relapse of the underlying disease.

- Hyperpigmented verrucous plaques and superficial erosions over chest and abdomen.

- Hyperpigmented verrucous plaques and superficial erosions over the back.

- Close-up view of the acanthoma.
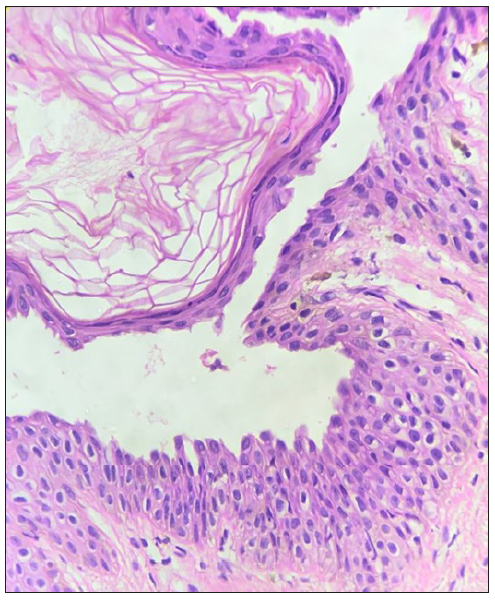
- Histopathology showing stratum corneum with loose hyperkeratosis, sub-corneal blister with acantholytic cells and irregular acanthosis. (Haematoxylin and Eosin, 400x).
PPA is a rare dermatological phenomenon and only a few case reports have been published till date. It typically develops following the resolution of pemphigus lesions, either during remission or after treatment. The trunk is commonly affected. They may arise months to years after the initial pemphigus diagnosis.1,3,4
The exact cause of PPA is unclear, but it possibly involves a complex interplay of autoimmune mechanisms, inflammatory responses, and bacterial colonisation of the skin. Another hypothesis suggests that certain autoantibodies produced during the active phase of pemphigus may continue to stimulate epidermal hyperproliferation even after disease remission, resulting in the development of acanthomata lesions.5
Clinically, PPA lesions present as raised, hyperpigmented plaques with a ‘stuck-on’ appearance, resembling warts or seborrheic keratoses. They may be asymptomatic or associated with mild itching or discomfort.
Clinically these lesions may be confused with seborrheic keratosis, post eczema acanthomata pemphigus vegetans and acantholytic acanthoma.6,7 PPA lesions usually disappear after a period whereas seborrheic keratosis and acantholytic acanthoma lesions are persistent and spontaneous resolution is uncommon. Pemphigus vegetans is characterised by flaccid blisters that erode and subsequently form fungoid vegetations or papillomatous proliferations, especially involving intertriginous areas and scalp, which can be differentiated easily from PPA lesions having truncal predilection.
Histopathologically, PPA lesions demonstrate hyperkeratosis, acanthosis, and papillomatosis along with characteristic intra-epidermal clefting and acantholytic cells. The absence of intra-epidermal clefting is a differentiating histopathological feature from seborrheic keratosis. In acantholytic acanthoma, acantholysis is seen at multiple epidermal levels with occasional focal spongiosis and a variable perivascular lymphohistiocytic infiltrate in the superficial dermis.1,7 Histopathology of pemphigus vegetans is characterised by pseudoepitheliomatous hyperplasia, with numerous eosinophils usually populating the epidermis and dermis producing both eosinophilic spongiosis and eosinophilic pustules. Supra basal split and acantholysis may be focal and not as prominent as seen in PPA.1 Positive direct immunofluorescence of the acanthomata lesions can indicate disease activity in an affected patient.
It is important to differentiate PPA from other skin lesions and provide appropriate management. This often involves close monitoring, as these lesions may resolve spontaneously over time. However, if symptomatic or cosmetically bothersome, treatment options may include topical therapies (e.g., corticosteroids, keratolytics) or systemic immunosuppressive agents, similar to those used for pemphigus vulgaris or pemphigus foliaceus. Since our patient could not afford rituximab and cyclophosphamide was contra-indicated, the case was managed by replacing methotrexate with azathioprine and close monitoring of disease activity.
While PPA typically represents a sign of remission in pemphigus, recent reports have suggested otherwise.1,3,4 In our patient, the phenomenon was accompanied by an increase in the number of blisters, the extension of erosions, the re-appearance of perilesional erythema and positive Nikolsky sign. Taken together, one may suggest that PPA can be seen anytime during the disease course, either during remission or before relapse. Our case underscores the importance of closely monitoring these patients, observing disease activity and tailoring therapy accordingly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Post pemphigus acanthomata: A sign of clinical activity? Int J Dermatol. 1997;36:194-6.
- [CrossRef] [PubMed] [Google Scholar]
- Post-pemphigus acanthomata presenting as an isolated, hyperkeratotic plaque. Dermatopathology. 2023;10:86-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Verrucous variant of pemphigus foliaceus. Clin Exp Dermatol. 2019;45:584-5.
- [CrossRef] [PubMed] [Google Scholar]
- Recalcitrant vegetative and nodular scalp lesions on the vertex in pemphigus patients: An immunocompromised district? An Bras Dermatol. 2023;98:102-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Murray Williams Warts. Indian J Dermatol Venereol and Leprol. 1997;63:107.
- [PubMed] [Google Scholar]
- Acanthomata appearing after eczema. Br J Dermatol. 1956;68:268-71.
- [CrossRef] [PubMed] [Google Scholar]





