Translate this page into:
Cutaneous alternariosis presenting as vasculitic ulcers
Corresponding author: Dr. Furen Zhang, Department of Dermatology, Shandong Provincial Institute of Dermatology and Venereology, Shandong Province, Jinan, Shandong, China. zhangfuren@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Cao S, Bao F, Chen S, Liu H, Zhang F. Cutaneous alternariosis presenting as vasculitic ulcers. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_831_2024
Dear Editor,
Cutaneous alternariosis is phaeohyphomycosis caused by Alternaria species. It has a broad clinical presentation spectrum with a few cases associated with diabetes. On the contrary, cutaneous vasculitis is a generic term for various types of vasculitis affecting the skin. The treatment options for these two diseases are completely different. Here, we report the first case of Alternaria alternata–induced cutaneous granuloma presenting in a vasculitis-like pattern. Dermatologists should recognize the possibility of fungal infections in diabetic or other immunosuppressed patients for accurate and early diagnosis.
A 63-year-old man presented with a 4-month history of multiple, reddish-brown, painful papules on his legs. A cutaneous examination revealed nodules and ulcerative lesions without scales that resembled vasculitis lesions on his left leg [Figure 1]. The patient was treated with cyclosporine for 1 month without any improvement. The patient’s diabetes was not well controlled, and his blood glucose level was 14.4 mmol/L (normal range: 3.9–6.1 mmol/L). A subsequent skin biopsy of the nodules revealed dermal granulomatous infiltrate with lymphocytic, neutrophilic, and multinuclear giant cells, with a positive finding of fungal spores in the dermis on a periodic acid-Schiff stain [Figure 2]. Direct microscopic examination of the scrapped material showed club-shaped conidia [Figure 3a]. The culture demonstrated brown septate hyphae and multiple darkly pigmented ovoidal conidia muriformes in groups and branched chains [Figure 3b]. A. alternata was confirmed using a quantitative polymerase chain reaction assay. Subsequently, oral itraconazole was administered at a dose of 200 mg twice daily based on in vitro antifungal susceptibility testing results using the microbroth dilution method. The patient’s lesions resolved significantly after 6 months of treatment [Supplementary figure]. The blood glucose level was normal at 5.7 mmol/L after treatment.

- Vasculitis lesions in the left leg.
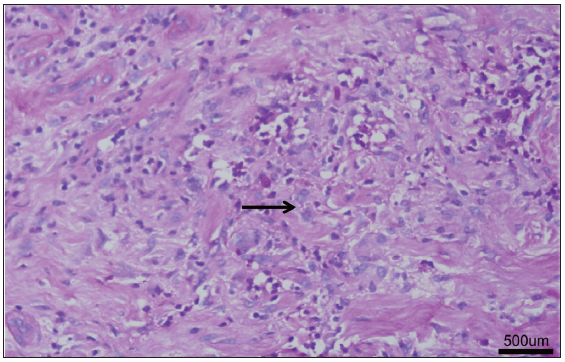
- Histopathological examination demonstrated positive fungal spores findings on the dermis based on the periodic acid-Schiff stain (Haematoxylin–eosin; bar: 500 μm).
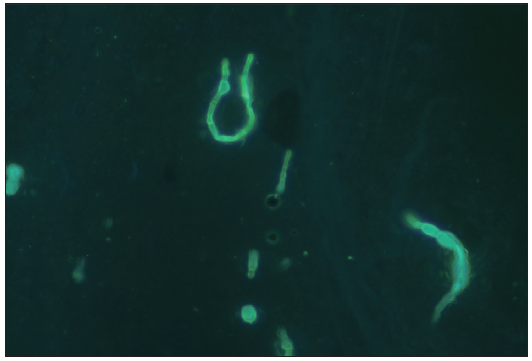
- Direct microscopic examination with fluorescent staining of the scrapped material revealed club-shaped conidia (400x).
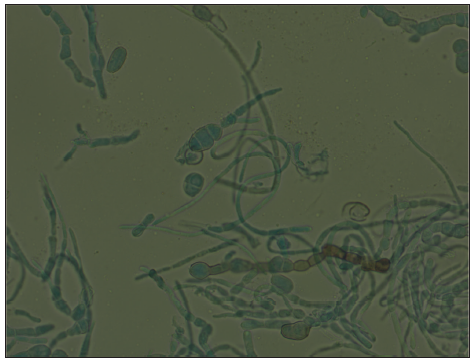
- Fungal tissue culture with lactophenol cotton blue mount showing brown septate hyphae and multiple darkly pigmented, ovoidal conidia muriformes (400x).
Alternaria species are well-known soil saprophytes and plant pathogens that are commonly found in the air, skin, nails, soil, and plants.1–3 Cutaneous alternariosis is a phaeohyphomycotic infection caused by Alternaria species with a broad spectrum of clinical presentation. The predisposing factors include immunosuppression, local wounds, or systemic diseases, such as diabetes. The clinical presentations are broad, comprising papulonodules, plaques, ulceration, subcutaneous nodules, or bullous lesions.3–5 Erythema and papulonodules are the common clinical manifestations of cutaneous alternariosis.1
However, necrotising vasculitis-like patterns in cutaneous alternariosis have not yet been reported. In the present case, the decreased immunologic state and subsequent damaged areas that were difficult to heal caused by diabetes mellitus weakened the resistance to fungal invasion, which may not occur in immunocompetent patients. Itraconazole was still effective in improving the patient’s lesions as in other reported clinical presentations of cutaneous alternariosis.
Skin disorders affect about one-third of patients with diabetes mellitus. The prevalence of pruritus and xerosis in diabetic subjects is significantly higher than that in age-matched non-diabetic subjects, especially in the lower limbs.2 The changes in the immunological system and pruritus with skin trauma increased the opportunity for fungal infection. Under these conditions, the Alternaria species can infiltrate the epidermis wounds and continue to expand into the dermis to form lesions in cases of diabetes with unusual immunological systems.
In summary, we reported a case of cutaneous alternariosis that was misdiagnosed as vasculitis due to similar clinical features. The patient denied having any local wounds, which contributed to the confusion about the diagnosis. Diabetes is a potential risk factor for this patient, who often scratched due to itching symptoms, causing local wounds on the limbs. Though the variable lesions of cutaneous alternariosis may cause misdiagnoses, the underlying disease offered important information for the diagnosis. A history of diabetes mellitus is associated with pruritus, especially on the anterior tibialis skin. Dermatologists should be aware of the possibility of fungal infections in immunosuppressed patients, including those with diabetes. Hence, it is necessary to investigate the aetiology of the disease. We recommend strengthening health education for diabetic patients and enhancing skin health management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This study was supported by the Shandong Province Taishan Scholar Project (tsqn202211345).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)–assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)–assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Cutaneous alternariosis—A case series of an increasing phaeohyphomycosis. J Eur Acad Dermatol Venereol. 2015;29:2053-54.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic generalized pruritus without primary skin lesions: A longitudinal prospective observational study. Int J Dermatol. 2019;58:273-78.
- [CrossRef] [PubMed] [Google Scholar]
- Image gallery: Cutaneous infections caused by Alternaria alternata and Mucor irregularis 1 year apart in a patient with iatrogenic Cushing syndrome. Br J Dermatol. 2016;174:e82.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual presentation of subcutaneous phaeohyphomycosis by Alternaria alternata. Ann Dermatol. 2019;31:563-66.
- [CrossRef] [PubMed] [Google Scholar]
- A case of cutaneous ulcerative alternariosis: Rare association with diabetes mellitus and unusual failure of itraconazole treatment. Clin Infect Dis. 2001;32:1178-87.
- [CrossRef] [PubMed] [Google Scholar]





