Translate this page into:
Outcome measures in chronic urticaria: A comprehensive review
Corresponding author: Dr. Muthu Sendhil Kumaran, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India, drsen2017@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shah S, Gupta M, Bishnoi A, Parsad D, Kumaran MS. Outcome measures in chronic urticaria: A comprehensive review. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_523_2024
Abstract
Chronic urticaria, characterised by pruritic wheals, angioedema or both significantly impacts individuals’ quality of life. This review article examines the patient-reported outcome measures (PROMs) in chronic urticaria assessment, aiming to enhance understanding and management of this condition The review categorises PROMs into urticaria-specific and angioedema-specific tools. Urticaria-specific PROMs such as the Urticaria Activity Score (UAS), Urticaria Control Test (UCT), Chronic Urticaria Quality of Life Questionnaire (CU-QoL) and Urticaria Severity Score (USS) focus on disease activity, control, severity and quality of life. Angioedema-specific tools include the Angioedema Activity Score (AAS), Angioedema Control Test (AECT) and Angioedema Quality of Life Questionnaire (AE-QoL), assessing disease activity, control and quality of life specific to angioedema. Non-specific PROMs like the Dermatology Life Quality Index (DLQI) provide a broader assessment of health-related quality of life across dermatological conditions. Newer developments include disease-specific PROMs like the Cold Urticaria Activity Score (ColdUAS), CholU-QoL for chronic inducible urticarias and the Urticaria Activity and Impact Measure (U-AIM) for retrospective patient-reported outcome assessment. Additionally, the review discusses the integration of smartphone applications and artificial intelligence (AI) tools like Convolutional Neural Networks (CNNs) in automating PROMs, showing promise in improving chronic urticaria management. Despite the progress made in PROMs, ongoing challenges such as limited data on specific populations and languages underscore the need for continued research and standardised PROM usage across clinical settings. This approach can significantly enhance patient management and contribute to a more holistic and effective strategy for addressing chronic urticaria.
Keywords
Angioedema
Patient-reported outcome measures
PROM
Urticaria
Introduction
A substantial percentage of people suffer from chronic urticaria, which is characterised by pruritic wheals, angioedema or both. Its prevalence varies between 0.5% and 1%.1 The affected age range for chronic spontaneous urticaria (CSU) is mostly 20–40 years, and it often lasts for an average of 3–5 years. Beyond physical symptoms, chronic urticaria sufferers have to deal with negative consequences that affect their day-to-day functioning, like erratic nature of symptoms, unpredictable nature of attacks, sleep disturbances, social isolation and financial strain.2 [Figure 1] Physician-reported outcome measures are not possible in CSU, since the diagnosis is usually based on history and pictures. Easily accessible biomarkers that complement clinical markers, such as patient-reported outcome measures (PROMs), are lacking in urticaria. Therefore, all treatments are essentially evaluated against the patient reported outcome measures. This emphasises the need for instruments that can gauge the total impact of illness on quality of life in patients with CSU and evaluate efficacy of treatment from the viewpoint of the patient. Within this framework, PROMs have become useful tools for assessing the subjective experiences and viewpoints of people who have chronic urticaria.3 This review highlights several recent advancements in the management and assessment of chronic urticaria like artificial intelligence, smartphone applications and newer PROMs. Here, we summarise the recommended PROMs of chronic urticaria which will help the physician in day-to-day urticaria assessment.
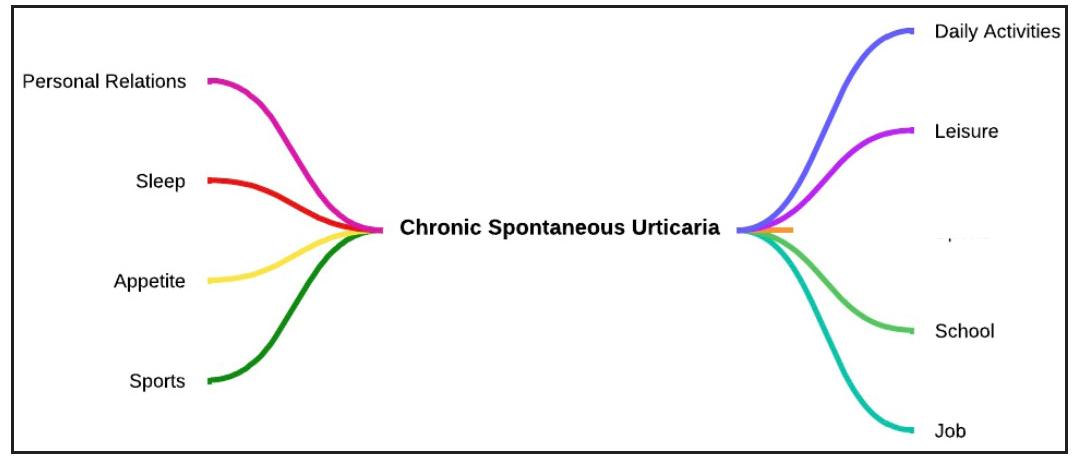
- Impact of chronic urticaria: Persistent hives and itching disrupt sleep, daily activities, work/school attendance, leisure, sports, and may affect income.
Methods
A literature search for published data on PROMs for Angioedema (AE), hereditary angioedema (HAE), and chronic spontaneous urticaria was conducted in PubMed. The search utilised the terms ‘hereditary angioedema’, ‘angioedema’, ‘HAE’, ‘urticaria’, ‘chronic spontaneous urticaria’, ‘chronic inducible urticaria’ and ‘oedema’, both alone and in combination with ‘patient-reported outcomes’, ‘PROMs’, ‘PROM’, ‘health-related quality of life’ and ‘HRQoL’. The search identified 78 different articles. All articles with non-validated PROMs were excluded. The search yielded 11 urticaria or angioedema-specific PROMs and one non-specific PROM discussed in this review. Among the non-specific PROMs, we only included Dermatology Life Quality Index as it is the most common non-specific PROM used in clinical practice and excluded other non-specific PROMs. The last date of search was 20 March 2024.
PROMs in clinical practice
Patient-reported outcome measures are surveys or other tools designed to gauge how a patient’s quality of life is affected by their overall health or a particular condition from their point of view. Developers interview patients to identify the most significant symptoms influencing their quality of life as well as the most effective method to phrase questions to capture those symptoms, their intensity and the degree to which they interfere with daily activities in order to design disease-specific PROM instruments.
In clinical practice, six distinct PROMs are now used to assess different features of CSU and related angioedema. Urticaria Activity Score (UAS), Urticaria Control Test (UCT), Chronic Urticaria Quality of Life Questionnaire (CU-QoL) and Urticaria Severity Score (USS) are the four PROMs that focus on urticaria. Angioedema is also the focus of three PROMs: Angioedema Activity Score (AAS), Angioedema Control Test (AECT) and the Angioedema Quality of Life Questionnaire (AE-QoL).4 Other non-specific PROMs include Dermatology Life Quality Index (DLQI) and its childhood variant (CDLQI) and Family Dermatology Life Quality Index (FDLQI).
Summary of PROMs in chronic urticaria is provided in Table 1. The advantages and disadvantages of various PROMs are discussed in Table 2.
| Patient centric assessment tool | Evaluated areas | Scoring method | Scoring range | Assessment type | Insights | Minimal clinically important difference | Available from |
|---|---|---|---|---|---|---|---|
| Urticaria Activity Score (UAS) | Itching and wheals | Scoring ranges from 0 to 3 for each question | 0 to 42 points | Diary-based Prospective | Scores ≤6 signify minimal disease activity; scores ≥28 indicate severe urticaria. | 7 | https://www.dermallergy.com/resources/csu-library/uas7-pro-calculator |
| Urticaria Control Test (UCT) | Disease control | Each question is rated on a scale of 0 to 3 | 0 to 16 points | Questionnaire Retrospective | A score of ≥12 suggests effective disease control. | 3 | https://survey.urtikaria.net/ |
| Urticaria Severity Score (USS) | Impact on quality of life, duration of itch and swelling, medication | Scores range from 0 to 7 for 10 questions; one question (corticosteroid) has double weight; Two questions are scored 0–8 | 0–93 points | 11-Item questionnaire | Higher scores indicate a more significant impact on quality of life. | - | https://www.annallergy.org/article/S1081-1206(10)60120-2/abstract |
| Urticaria Activity and Impact Measure | CSU activity and impact during the previous seven days. |
Each item scored from 0 to 4 Proxy UAS7 – 0–42 |
0–74 | Nine-item questionnaire | The U-AIM represents a practical, retrospective tool to assess disease activity and effect of CSU that does not require daily assessments. | 0.8 | https://www.annallergy.org/action/showPdf?pii=S1081-1206%2818%2930210-2 |
| Chronic Urticaria Quality of Life Questionnaire (CU-Q2oL) | pruritus, swelling, daily life, sleep, appearance, limitations | Each question is rated on a scale of 1–5 | 23–115 points | 23-Item Assessment | Higher scores reflect a more pronounced negative impact on health-related quality of life. | 15 | https://survey.urtikaria.net/ |
| Cold Urticaria Activity Score | Frequency and severity of the signs (wheals and/or angioedema), (2) frequency and severity of the symptoms (e.g. itch and burn), (3) exposure to specific triggers and (4) avoidance of these triggers | Recall period for each item is the last 24 hours. Four-point Likert scale with answer options “No” “mild,” “moderate,” “severe” (for questions 1–3); “partially” and “completely” for question 4. | Exact score calculation is under development | Recall period for each item is the last 24 h | ColdUAS will help to determine and monitor disease activity in routine clinical practice and ColdU management, including treatment, which is currently difficult. | - | https://onlinelibrary.wiley.com/doi/full/10.1111/all.15310 |
| Cholinergic Urticaria Quality of life | 5 domains - “symptoms”, “functional life”, “social interaction”, “therapy”, “emotions” | Each CholU-QoL item was scored from 0 to 4 points | 100 points | 25-item questionnaire | CholU-QoL is the first instrument with excellent validity and reliability for the assessment of disease-specific QoL impairment in patients with CholU, which may be used as an index instrument to measure the overall CholU-related QoL impairment. | - | https://survey.urtikaria.net/ |
| Angioedema Activity Score (AAS) | Physical discomfort, daily activities, cosmetic impact, global severity | Scores range from 0 to 3 for each question | 0–15 points | Five-Question Assessment | Elevated scores indicate higher disease activity. | - | https://moxie-gmbh.de/products/aas |
| Angioedema Quality of Life Questionnaire (AE-QoL) | Functioning, fatigue/mood, fears/shame, food | Each question is rated on a scale of 0–5 | 0–85 points | 17-Item Evaluation | Higher scores suggest a greater impact on overall quality of life. | 6 | https://survey.urtikaria.net/ |
| Angioedema Control Test | Quality of life, symptoms, therapy | 3 | https://survey.urtikaria.net/ | ||||
| Dermatology Life Quality Index (DLQI) | Symptoms, social activities, work/school, personal relationships, treatment-associated problems | Scores range from 0 to 3 for each question | 0–30 points | Ten-item questionnaire | High scores indicate a more pronounced impact on overall quality of life. | 2.24–3.10 | http://www.dermcalculator.com/dlqi/ |
| PROM | Advantages | Disadvantages |
|---|---|---|
| Urticaria Activity Score (UAS) |
Prospective, CSU-specific measure evaluates disease activity, severity and treatment response Predicts treatment outcomes and prognosis Daily scoring provides a detailed picture Correlations with various aspects of urticaria noted |
Not suitable for chronic inducible urticaria (CIndU) |
| Urticaria Control Test (UCT) |
Simple, fast completion Covers multiple parameters beyond itch and wheals Combined use with UAS for a comprehensive understanding Standardised and quantitative assessment Valuable in clinical research |
Influenced by cultural and language differences May not capture fluctuations in disease control between assessments |
| Chronic Urticaria Quality of Life Questionnaire (CU-QoL) |
Assesses the impact on various aspects of life Tracks changes over time and evaluates interventions Detailed evaluation of disease impact |
Applicable only for CSU, lacks specific angioedema questions Time-consuming Validated for adults only Equal weighting of all questions may not reflect individual priorities |
| Urticaria Severity Score (USS) |
Monitors severity, quality of life and treatment efficacy Standardised approach to treatment Enables longitudinal monitoring |
Time-consuming Does not account for variations in aetiology or specific triggers May not fully reflect the complete range of symptoms or their effect on QoL |
| Angioedema Activity Score (AAS) |
Symptom-specific PROM for angioedema Versions with four-week and three-month recall periods Provides nuanced understanding of temporal dynamics |
Does not account for variations in aetiology or specific triggers |
| Angioedema Quality of Life Questionnaire (AE-QoL) |
Specific and targeted assessment of angioedema impact Captures burden beyond clinical symptoms Available in multiple languages |
May not be sensitive to subtle changes in QoL over time Requires further evaluation for the minimal clinically important difference |
| Angioedema Control Test (AECT) |
Retrospective evaluation of disease control Simple, brief and easy to administer Available in two versions with different recall durations |
Requires more validation research in larger populations to establish dependability |
| Hereditary Angioedema-specific tools (HAE-AS, HAE-QoL) | Evaluate disease activity and quality of life specifically for hereditary angioedema | Limited information on the performance in different populations, and in children and adolescents |
| Cold Urticaria Activity Score (ColdUAS) |
Self-administered questionnaire for ColdU Prospective measurement of disease activity Covers various factors, including symptoms, triggers and avoidance |
Limited to ColdU cases, not applicable for other forms of urticaria |
| CholU-QoL |
Disease-specific QoL measure for chronic inducible urticarias Valid total score with good reliability and validity |
Not developed for children with CholU Sensitivity to change and minimally significant difference not fully characterised |
| Urticaria Activity and Impact Measure (U-AIM) |
Nine-item patient-reported assessment for CSU Evaluates activity and impact in the preceding seven days Single evaluation, unlike UAS7 or UAS7TD |
Some individuals may not have symptoms for the seven days prior to evaluation |
| Dermatology Life Quality Index (DLQI) |
Generic skin-specific questionnaire Useful for comparing QoL across different dermatological diseases |
Non-urticaria specificity may limit sensitivity compared to urticaria-specific PROMs |
Urticaria-specific PROMs
Several specific PROMs have been developed in order to assess the impact of chronic urticaria on the quality of life of affected patients.
Urticaria activity score
It is the most widely used CSU-specific, prospective, and patient-reported measure that evaluates disease activity or severity in the previous week. With its scoring system, ranging from remission to severe disease activity, the urticaria activity score has proven effective in predicting treatment outcomes and prognosis. Both the number of wheals (0–3: >50) and the intensity of the itch (0–3: severe) make up this questionnaire. Every 24 hours, patients must record the symptoms, and the combined data produces a daily urticaria activity score ranging from 0 to 42. A score of 0 denotes the complete absence of wheals and itching, while a score of 6 denotes the lowest feasible degree of disease activity.
There are now two variants of the daily urticaria activity score: one measures the number of hives and the severity of the itching twice a day (every 12 hours), while the other measures the same two parameters once a day (every 24 hours). A weekly score (UAS7) is the total of the daily hives score and itching intensity. UAS7 stratification values are currently being defined. A UAS7 score between 7 and 15 denotes low disease activity, between 16 and 27 moderate disease activity and between 28 and 42 severe disease activity.5 A recent study discovered a strong correlation and consistency between UAS7 results based on twice daily versus once daily measurement of itch intensity and number of hives.6
Studies have demonstrated correlations between urticaria activity score and various aspects of chronic urticaria, providing valuable insights into predicting treatment responses and disease outcomes.7 It is not suitable for chronic inducible urticaria (CIndU), as the patients may avoid their known triggers and may have variable exposure to the triggers, hence urticaria activity score may be applicable in limited cases. According to a recent investigation, up to 36% of patients with CSU also had CIndU. The urticaria activity score in this group may be impacted by inducible urticaria activity, since it may be challenging for the patients to distinguish between the symptoms of CSU and CIndU.
The urticaria activity score however does not link the clinical severity of the condition to both the psychological distress brought on by chronic urticaria and quality of life.
The urticaria control test
Designed as a retrospective four-question instrument, urticaria control test assesses disease control among CSU patients in the preceding one month.8 Its advantages include simplicity, fast completion and coverage of multiple parameters beyond itch and wheals. A score of ≤11 denotes inadequate illness management, whereas a score of ≥12 suggests well-controlled urticaria. The initial inquiry concerns the frequency of all three symptoms together: itching, hives and/or swelling. The overall impact on quality of life is the subject of the second question, the frequency of treatment failure to control symptoms is the subject of the third question; and the overall effectiveness of illness management is the subject of the fourth and final question. For CSU patients, urticaria control test provides a quantifiable, standardised evaluation of disease control. Patients with both spontaneous and inducible chronic urticaria can evaluate their illness control using the urticaria control test, which is the first reliable and useful instrument for this purpose. However, children were not used in the testing of the urticaria control test. Furthermore, the urticaria control test requires language validation, and it might miss fluctuations in disease control between evaluations. Combined use of urticaria severity test and urticaria control test is proposed to provide a more comprehensive understanding of disease control.7
Chronic urticaria quality of life questionnaire
Chronic Urticaria Quality of Life Questionnaire (CU-QoL) evaluates how pruritus, swelling, everyday activities, sleep and appearance are affected in patients with chronic urticaria. It monitors improvements in quality of life over time and assesses how well treatments work.9 Condition-specific quality of life (QoL) considers how the affected person perceives the physiological effects of the condition and the available treatment options. This subjective instrument is essential for evaluating chronic conditions like CSU and comparing various treatment options. Unlike symptom rating, QoL surveys may be used to measure and track changes in a variety of aspects, including emotional changes. QoL must be given high priority in the management of illness due to the very low mortality rate and the unexpected character of CSU episodes. Generic QoL surveys may be used to assess the effects of different diseases, enabling some cross-population comparison. Among Indian languages, its use has been validated in Bengali.10 It does not, however, contain any particular questions on the effects of angioedema and is relevant to only CSU. Although it provides a thorough analysis of the disease’s effects, it has several limitations, including time requirements and the equal weighting of all questions. This is not appropriate for CholU – it only applies to CSU – and is recommended for use in adults.
Urticaria severity score
Urticaria Severity Score (USS) monitors the severity of chronic urticaria, quality of life and treatment efficacy through 12 questions covering distinct aspects of patients’ experiences.11 In addition to offering a standardised treatment plan, urticaria severity score makes it possible to track the course of the disease over time in CSU patients. While the urticaria severity score offers a sensitive indicator for tracking response to therapy, one significant drawback is its time-consuming nature. Nevertheless, it does not accurately represent the whole spectrum of symptoms, the size of the wheals or their impact on quality of life, nor does it take into consideration differences in chronic urticaria’s aetiology or particular triggers. There is another score –the UTSS (urticaria total severity score) – which takes into account the size of the wheals as one of its components.12
Angioedema-specific tools
The angioedema activity score
It is a recommended five-item tool for assessing disease activity in patients with recurrent angioedema. With different versions employing both the four-week and the three-month recall periods, it provides a nuanced understanding of the disease’s temporal dynamics. AAS is a standardised, symptom-specific PROM designed to assess disease activity in angioedema cases, including hereditary angioedema. Its application may be impacted by the fact that it only evaluates the frequency and length of angioedema episodes, without taking into consideration changes in aetiology or particular triggers.
Comprehensive health-related quality of life (HRQoL) questionnaires tailored to angioedema patients, comprising 17 items and accessible in several languages, enhance the evaluation of functioning, mood/fatigue, anxiety/shame and food-related effects.13
Angioedema quality of life questionnaire
The goal of angioedema QoL is to give physicians a focused and precise evaluation of how angioedema has affected the quality of life of patients. There are 25 items in it that cover pertinent Health-Related QoL (HRQoL) domains.14 It recognises and measures the angioedema burden that goes beyond clinical manifestations. However, depending solely on self-reporting might result in subjective biases and make it less responsive to gradual shifts in QoL. The tool also takes into account functioning, mood, fatigue, fear/shame of illness which may be missed by asking only about the symptom frequency. Hence, it holds the potential to capture the unique challenges faced by angioedema patients.
Angioedema control test
The four-item Angioedema Control Test (AECT) was created to evaluate disease control retrospectively over time in individuals with recurrent angioedema. The four angioedema control test items evaluate unpredictability, impact, treatment efficacy and signs and symptoms.15 There are two variants of the angioedema control test available: one with a three-month recall time and the other with a four-week recall period. The angioedema control test can be used in clinical trials and regular clinical practice because of its simplicity, concision and retrospective methodology; nevertheless, further validation research in bigger populations is needed to completely characterise its dependability.
Hereditary angioedema-specific tools
Hereditary Angioedema Activity Score (HAE-AS) is a 12-item retrospective questionnaire that evaluates disease activity. Two of the items have a one-month recall period, while the remaining ten have a six-month recall time.16
Hereditary Angioedema Quality of Life (HAE-QoL) is a six-month recall period retrospective questionnaire. It consists of 25 questions broken down into 7 sections that assess treatment difficulties, mental health, physical functioning and health, stigma associated with disease, emotional role, and social functioning, perceived control over illness, and concern for children.17
Non-specific PROMs
Dermatology life quality index
The dermatology life quality index, a generic skin-specific questionnaire, serves as a standard in assessing health-related QoL across various dermatological diseases. While advantageous for comparing QoL across different conditions and languages, its non-urticaria specificity may limit sensitivity compared to urticaria-specific PROMs.
Newer PROMs
Cold Urticaria Activity Score
The ColdUAS (cold urticaria activity score) is a self-administered questionnaire designed to monitor disease activity prospectively in persons with cold urticaria. The four criteria to take into account are the frequency and severity of symptoms (burning and itching), frequency and severity of signs (wheals and/or angioedema), exposure to certain triggers, and avoidance of these triggers. Recall period for each item is the preceding 24 hours.18 Patients with any kind of cold urticaria, including primary, secondary, and familial subtypes and whether typical or atypical, can utilise this score if they are at least 12 years old.
Cholinergic Urticaria Quality of Life
The first disease-specific quality-of-life measure for chronic inducible urticarias as well as the first of its kind is the cholinergic urticaria quality of life (CholU-QoL). It could enhance regular patient management and be a useful tool for clinical studies.
Excellent internal consistency was observed in the five-domain framework of the final 28-item cholinergic urticaria quality of life (symptoms, functional life, social interaction, therapy and emotions).19 Additionally, the cholinergic urticaria quality of life demonstrated acceptable levels of test-retest reliability, known groups validity, and convergent validity in addition to a valid total score. No significant predictors of the cholinergic urticaria quality of life total score were identified by multiple regression analysis.
The tool has not been validated in children. Other limitations include lack of studies to determine its sensitivity and minimal clinically important difference.
Urticaria Activity and Impact Measure
A recently created quick retrospective nine-item patient-reported outcome measure intended for use in clinical practice is called Urticaria Activity and Impact Measure (U-AIM). Urticarial activity and effect through the preceding seven days are evaluated utilising a seven-day patient recall in only one assessment. The Urticaria Activity and Impact Measure is a useful, retroactive technique that does not require daily evaluations to evaluate the impact and disease activity of CSU. While daily evaluation and documenting of illness activity as part of the UAS7 allow patients to actively manage their condition and identify triggers, the Urticaria Activity and Impact Measure also offers a proxy score for the UAS7.12 However, it is a relatively longer questionnaire, and some individuals might not have any symptoms for the seven days before their doctor’s appointment.
PROM accessibility in smartphone applications
It would be ideal to have apps designed for tracking daily symptoms, managing the condition and routinely evaluating the quality of life of CSU patients. They can assist in identifying significant initiators (stress, infections) as well as the consequences for day-to-day functioning (difficulty sleeping, absence from work or school, and other comorbidities). Additionally, applications that monitor daily circumstances and particular problems can be very helpful to the doctor in creating the best possible treatment plan. The UCARE CURCIT analysis [Urticaria Centers of Reference and Excellence (UCARE); chronic urticaria information and communication technologies (CURICT)] shows that many patients, especially those with higher education levels, are keen to use smartphone applications and communication technology to monitor their illness and communicate with their doctors on a regular basis.20 However, a study by Antó et al. in 2016 showed that there are not many smartphone applications available globally for CSU patients.21 TARGET My Hives, UrCare, Urticaria, UrticariApp, and SymTracTM HIVES are the five applications for CU self-evaluation that were found through both automatic and manual searches in this study. Only two of these apps permitted the entry of triggers, while three permitted the entry of prescriptions taken. None of the five discussed comorbidities or offered personalised guidance. This indicates that patients have limited access to CU-driven apps on the iOS and Android platforms.
A global steering team of experts in urticaria created a recent app in 2022, called CRUSE®. Patients’ ability to track and record their symptoms and medication use over time as well as share images was identified as a priority for the app on CSU, which was based on active patient engagement. In order to provide doctors with real-time insights, the CRUSE® app gathers patient data, including age, sex, disease onset, triggers, medication, and CSU features. The validated urticaria PROMs that make up CRUSE® are urticaria activity score (UAS), angioedema activity score (AAS), urticaria control test (UCT), and angioedema control test (AECT). The EQ-5D visual analogue scale (EQ-5D VAS) is also included. The range of this quantitative measure, from ‘the best health you can imagine’ to ‘the worst health you can imagine’, represents the patients’ assessment of their current state of health.22 This data are then securely communicated to doctors.
Artificial intelligence and urticaria outcome measures
The traditional process of completing urticaria activity questionnaires is time-consuming, and is susceptible to bias because of its subjective nature. Scoring systems utilising limited categories lack continuous scales and exhibit high minimum detectable change. Moreover, asynchronous reporting hinders chronological accuracy and external verification. The introduction of AI, particularly Convolutional Neural Networks (CNNs), has revolutionised healthcare. A recent study proposes the automatic UAS (AUAS), leveraging CNNs to automate hive counting, aiming to enhance objectivity and speed in filling scoring systems like the UAS.23 This AI application has the potential to streamline the process, improve health outcomes and offer robust end-points for evaluating urticaria treatments.
Challenges and future directions
While PROMs have significantly contributed to understanding chronic urticaria, challenges remain. Limited data on inducible urticaria and paediatric populations necessitate further research.24 The transaction validation of PROMs in different languages, and exploring relationships between various PROMs are areas that require attention.
Expert perspective
While PROMs in chronic urticaria offer a comprehensive evaluation of the life quality of patients, it is often tedious to incorporate them in a busy practice. The authors generally use UAS7 and UCT in their urticaria clinic OPDs as PROMs as they are relatively more feasible. Apart from being essential research tools, these measures should be aligned with patient care for a holistic management of chronic urticaria. While the choice of PROMs is the clinician’s, there should be a tool used consistently in practice across all settings, to improve patient management in this frustrating disease.
Conclusion
Chronic urticaria profoundly impacts the QoL of affected individuals. PROMs play a pivotal role in identifying the overall impact of this skin disease. They offer a better understanding of the profound impact of urticaria on patients’ lives, guiding the physician regarding the effectiveness of treatment.
The integration of these measures in both clinical trials and routine practice is essential for a holistic evaluation of urticaria patients. Given the variability and subjective nature of urticaria symptoms, further research on these measures, especially in diverse populations and languages, is paramount.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The international EAACI/GA2LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy. 2022;77:734-66.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of chronic urticaria on the quality of life in Indian patients. Indian J Dermatol. 2012;57:110-3.
- [CrossRef] [PubMed] [Google Scholar]
- Patient reported outcome measures in practice. BMJ. 2015;350:g7818.
- [CrossRef] [PubMed] [Google Scholar]
- Clinically relevant outcome measures for assessing disease activity, disease control and quality of life impairment in patients with chronic spontaneous urticaria and recurrent angioedema. Curr Opin Allergy Clin Immunol. 2015;15:220-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinically relevant outcome measures for assessing disease activity, disease control and quality of life impairment in patients with chronic spontaneous urticaria and recurrent angioedema. Curr Opin Allergy Clin Immunol. 2015;15:220-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of urticaria activity score over 7 days (UAS7) values obtained from once-daily and twice-daily versions: Results from the ASSURE-CSU study. Am J Clin Dermatol. 2018;19:267-74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of omalizumab in chronic spontaneous urticaria assessed with patient-reported outcomes: A prospective study. J Eur Acad Dermatol Venereol. 2018;32:1761-7.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of the urticaria control test: A patient-reported outcome instrument for assessing urticaria control. J Allergy Clin Immunol. 2014;133:1365-72, 1372.e1–6.
- [CrossRef] [PubMed] [Google Scholar]
- A new tool to evaluate the impact of chronic urticaria on quality of life: Chronic urticaria quality of life questionnaire (CU-QoL) Allergy. 2005;60:1073-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adaptation and validation of the Bengali version of the chronic urticaria quality of life questionnaire (CU-Q2oL) Indian J Dermatol Venereol Leprol. 2023;89:385-92.
- [CrossRef] [PubMed] [Google Scholar]
- The urticaria severity score: A sensitive questionnaire/index for monitoring response to therapy in patients with chronic urticaria. Ann Allergy Asthma Immunol. 2009;102:475-82.
- [CrossRef] [PubMed] [Google Scholar]
- Validity and responsiveness of the urticaria activity and impact measure: A new patient-reported tool. Ann Allergy Asthma Immunol. 2018;120:641-7.
- [CrossRef] [PubMed] [Google Scholar]
- Development, validation, and initial results of the angioedema activity score. Allergy. 2013;68:1185-92.
- [CrossRef] [PubMed] [Google Scholar]
- Development and construct validation of the angioedema quality of life questionnaire. Allergy. 2012;67:1289-98.
- [CrossRef] [PubMed] [Google Scholar]
- Development of the angioedema control test: A patient-reported outcome measure that assesses disease control in patients with recurrent angioedema. Allergy. 2020;75:1165-77.
- [CrossRef] [PubMed] [Google Scholar]
- HAE-AS: A specific disease activity scale for hereditary angioedema with C1-inhibitor deficiency. J Investig Allergol Clin Immunol. 2021;31:246-52.
- [CrossRef] [PubMed] [Google Scholar]
- Psychometric field study of hereditary angioedema quality of life questionnaire for adults: HAE-QoL. J Allergy Clin Immunol Pract. 2016;4:464-73.e4.
- [CrossRef] [PubMed] [Google Scholar]
- Development of the cold urticaria activity score. Allergy. 2022;77:2509-19.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of the cholinergic urticaria quality-of-life questionnaire (CholU-QoL) Clin Exp Allergy. 2018;48:433-44.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic urticaria patients are interested in apps to monitor their disease activity and control: A UCARE CURICT analysis. Clin Transl Allergy. 2021;11:e12089.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Automatic screening of self-evaluation apps for urticaria and angioedema shows a high unmet need. Allergy. 2021;76:3810-3.
- [CrossRef] [PubMed] [Google Scholar]
- CRUSE® -An innovative mobile application for patient monitoring and management in chronic spontaneous urticaria. Clin Transl Allergy. 2024;14:e12328.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Automatic urticaria activity score: Deep learning-based automatic hive counting for urticaria severity assessment. JID Innov. 2023;4:100218.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Questions and answers in chronic urticaria: Where do we stand and where do we go? J Eur Acad Dermatol Venereol. 2016;30(Suppl 5):7-15.
- [CrossRef] [PubMed] [Google Scholar]






