Translate this page into:
Antibiotic resistance and biofilm formation in Cutibacterium acnes: A descriptive cross-sectional study
Corresponding author: Dr. Navya Anna Paul, Department of Dermatology, Cutis Academy of Cutaneous Sciences, Bangalore, Karnataka, India. Email id: navya.annapaul57@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Paul NA, M. Ramesh Bhat, Antony B, Jayaraman J. Antibiotic resistance and biofilm formation in Cutibacterium acnes: A descriptive cross-sectional study. Indian J Dermatol Venereol Leprol. 2025;91:315-20. doi: 10.25259/IJDVL_539_2024
Abstract
Background
The issue of antibiotic resistance in acne vulgaris has emerged as a significant concern in recent times. Though the ability of Cutibacterium acnes to form biofilms have been established, its role in acne vulgaris has yet to be ascertained.
Aims
This descriptive cross-sectional study was aimed to investigate the ability of C. acnes to form biofilms and its potential association with resistance to the commonly used antibiotics.
Methods
A total of 88 patients with acne vulgaris were selected for this study. Clinical examination and severity grading was done. The collected samples were analysed with Matrix-Assisted Laser Desorption Ionization Time of Flight Mass Spectrometry (MALDI-TOF-MS) and further subjected to biofilm testing using the microtiter plate assay.
Results
C. acnes were isolated from 43.1 of the samples (n = 38). The highest resistance was observed with azithromycin (73.7%) followed by clindamycin (65.8%), doxycycline (15.8%), ampicillin (31.6%) and minocycline (5.3%). Thirty-seven per cent of the isolates were resistant to at least two antibiotics, 63.2% of C. acnes had a weak capacity to form biofilms and more than 60 percent of the isolates showed resistance to atleast two types of antibiotics as well as weak biofilm forming capacity.
Limitations
Single-centre study, small sample, long-term follow-up of the patients was not done. In addition, this study is representative of only C. acnes species.
Conclusion
While C. acnes have the ability to create biofilms, its effectiveness in antibiotic resistance can be deemed as modest based on the findings of this study. It is important to consider alternative mechanisms such as genetic or biochemical plasticity that may contribute to antibiotic resistance.
Keywords
Acne
antibiotic resistance
biofilms
Cutibacterium acnes
Introduction
Acne vulgaris affects approximately 9.4% of the global population, making it a significant public health concern.1 The primary pathogen associated with acne vulgaris is Cutibacterium acnes, a bacterium that plays a pivotal role in maintaining the skin’s microbiota balance, ultimately leading to the development of this chronic inflammatory skin disease.2–4
Over the years, antibiotics, both in topical and oral forms, have been the cornerstone of acne management. However, the extended and often indiscriminate use of antibiotics has led to the emergence of antibiotic-resistant C. acnes strains, posing a formidable challenge to the current treatment protocols. Recent research has shed light on the potential role of biofilms (the structured aggregates of bacterial cells) in conferring antibiotic resistance to C. acnes.5,6 Biofilm formation may act as a protective shield, limiting the penetration of antibiotics and exacerbating resistance issues.
In light of this concern, our study aims to investigate the ability of C. acnes to generate biofilms and elucidate their potential connection to antibiograms. By doing so, we seek to contribute to a broader understanding of the dynamics of antibiotic resistance in acne vulgaris and pave the way for innovative strategies that address C. acnes biofilms and their implications for treatment.
Methods
Patients with clinically diagnosed acne vulgaris satisfying the inclusion and exclusion criteria, and attending the dermatology outpatient department for 18 months from November 2020 to May 2022 at a Tertiary Hospital in South India, were considered for the study. Approval from the institution’s scientific and ethics council was taken.
Study design: Descriptive Cross-sectional study.
Selection criteria
Patients over the age of 12 years with acne vulgaris were considered for the study. Patients who had not been treated with topical or oral antibiotics in any form for at least four weeks were enrolled. Patients who were using oral or topical isotretinoin, hormonal medication, or any complementary and alternative medicine (CAM) therapy were excluded; patients diagnosed with hormonal acne were also excluded.
Each patient was subjected to a comprehensive general physical, systemic, and cutaneous examination, and data were recorded on a preformatted proforma.
A clinical diagnosis of acne vulgaris was made. Using the Investigator’s Global Assessment Scale System (IGA), the disease severity was defined and categorised as Grade 0 to 4.
Grade 0: Clear; Grade 1: Few comedones with few papule; Grade 2: Less than half the face is involved with many visible comedones and pustules; Grade 3: Involvement of more than half the face with visible comedones, papules, pustules and one nodule; Grade 4: The entire face is involved with comedones, papules pustules, nodules and cyst.
Sample collection and processing
The skin surface was cleaned with ethanol. The sample was collected according to the type of lesion. Comedones/pustules were extracted/expressed from the lesion using a sterile needle and placed in a thioglycolate transport medium. The sample was mixed for 30 seconds in a vortex mixer to disperse the bacteria. The vortex sample was inoculated on Propionibacterium selective agar, placed in a Becton and Dickinson (BD) GasPak EZ Sachet (Germany) (anaerobic gas generating pouch system with indicator) and incubated at 37ᵒC for 48 hours to isolate Cutibacterium. After incubation, the characteristic large white to yellow dry colonies were identified as Cutibacterium species based on Gram’s staining, colony morphology, and Matrix Assisted Laser Desorption Ionization – Time of Flight Mass Spectrometry (MALDI-TOF MS) (Bruker, Germany).
Upon completion of Cutibacterium species identification, only C. acnes colonies were subjected to antimicrobial susceptibility testing on Brucella Blood Agar in an anaerobic environment using a Becton and Dickinson (BD) GasPak EZ sachet by disc diffusion technique.
For susceptibility testing, the following antimicrobial agents were used: doxycycline (30 mcg/disc), minocycline (30 mcg/disc), azithromycin (15 mcg/disc), ampicillin (10 mcg/disc) and, clindamycin (10 mcg/disc) [Figure 1].

- Antibiotics (minocycline, doxycycline, ampicillin, azithromycin and clindamycin) placed on Brucella Blood Agar showing different zones of inhibition (disc diffusion technique).
Due to its lack of lipophilic properties, ampicillin is not routinely used to treat acne vulgaris. However, it has been used for antibiotic sensitivity testing in C. acnes strains because it is a commonly used beta-lactam antibiotic that can effectively target gram-positive bacteria, including some C. acnes strains. In addition, using a well-known and widely used antibiotic facilitates the comparison of results across studies.
Antibiogram – disc diffusion technique
C. acnes were grown in Viande Levure (VL) broth, and the turbidity was adjusted to 0.5 McFarland before being applied to Brucella blood agar. On Brucella blood agar plates, the aforementioned antimicrobial discs were placed. After anaerobic incubation, the zones of inhibition on the plates were measured and compared with the Kirby-Bauer chart as established by the Clinical Laboratory Standards Institute (CLSI).7
Biofilms – using microtitre plate assay
Stock isolates frozen at ‒80°C in glycerol (50%) were revived in Bacto Brain Heart Infusion broth supplemented with glucose (0.5%) in the Don Whitley Anaerobic Chamber for 48 hours at 37°C. Quantification of biofilm formation was performed using a microtiter plate assay with modifications based on the study by Holmberg et al.6
C. acnes was grown for 48 hours in the Brain Heart Infusion broth supplemented with glucose, and 50 μL of this culture was added to the wells of a sterile 96-well flat-bottomed plastic culture plate containing 150 μL of the medium and incubated anaerobically at 37°C for 48 hours. A biofilm-producing Staphylococcus epidermidis was used as a positive control on each plate, and the medium alone served as a negative control. Each isolate was tested in duplicate. The medium was removed, followed by gentle washing (three times) with 200 μL of phosphate-buffered saline (PBS), by pipetting.
The remaining biofilm was fixed in 200 μL of methanol for ten minutes and then stained in 160 μL of crystal violet (1% [w/v] in water, gram staining for microscopy) for 4 min. The wells were destained by pipetting 200 μL of PBS three times and extracted with 200 μL of acetone-ethanol (20:80 [v/v]). In an enzyme-linked immunosorbent assay (ELISA) reader, the absorbance was measured at 550 nm [Figure 2]. The cut off OD values for the study were as follows:
-
1.
>0.240 was considered Strong Positive.
-
2.
>0.120 to <0.240 was considered Moderate positive
-
3.
<0.120 was considered to be Weak positive.
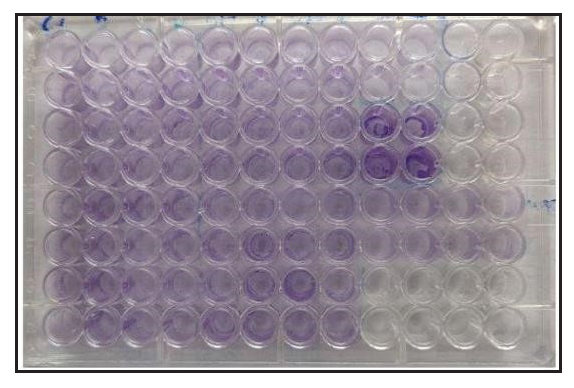
- Microtitre plate assay: Stained and fixed with crystal violet stain.
Results
Fifty-one per cent of patients belonged to the 21–30-year age group, while 45.5% were less than 20, with a mean age of 21 ± 4.45 years. Women constituted 71.6% of the patient population, while only 28.4% of patients were men. The female-to-male ratio was 2.5:1. The duration of acne varied from five months to six years.
The most frequently encountered severity of acne among the patients was Grade 3 (43.2%), followed by Grade 2 (31.8%) and Grade 4 (13.6%). The most prevalent skin lesions observed in these patients were pustules. C. acnes were isolated from 43.1% of the patients (N = 38).
Seventy-four per cent of the isolates showed resistance to azithromycin. The second most common antibiotic to show resistance was clindamycin (65.8%), followed by ampicillin (31.6%), doxycycline (15.8%), and minocycline (5.3%). Minocycline showed the most sensitivity (94.78%) followed by doxycycline (84.2%). Only two isolates showed resistance to minocycline [Figure 3, Table 1].
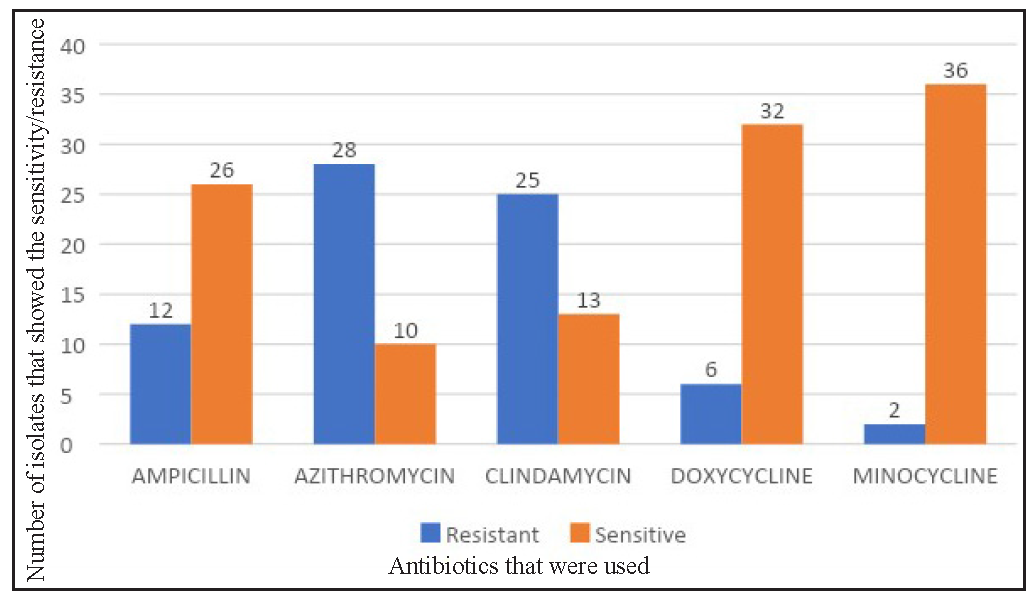
- Antibiotic susceptibility of antibiotics. Minocycline shows the most sensitivity.
| Antibiotic | Sensitive | Resistance | ||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Azithromycin (N=38) | 10 | 26.3 | 28 | 73.7 |
| Doxycycline (N=38) | 32 | 84.2 | 6 | 15.8 |
| Minocycline (N=38) | 36 | 94.7 | 2 | 5.3 |
| Ampicillin (N=38) | 26 | 68.4 | 12 | 31.6 |
| Clindamycin (N=38) | 13 | 34.2 | 25 | 65.8 |
An analysis of antibiotic susceptibility across different age groups, a distinct pattern was revealed for azithromycin. While most antibiotics exhibited comparable susceptibility profiles, azithromycin demonstrated significantly higher resistance (73.9%) in the 20 years and older age group compared to the under 20 group (73% susceptibility).
In our study, out of 38 isolates, 68.4 % of the isolates were resistant to two or more types of antibiotics, while 13.2% were resistant to only one antibiotic. Only 18 % of the samples were susceptible to all the antibiotics [Table 2 and Table 3].
| Number of antibiotics to which resistance was present | Number of isolates showing antibiotic resistance | Percentage distribution |
|---|---|---|
| 0 | 7 | 18.4% |
| 1 | 5 | 13.2 % |
| 2 | 14 | 36.8% |
| 3 | 8 | 21.1% |
| 4 | 4 | 10.5% |
| Total Isolates: 38 |
| Antibiotics | No of Strains | Percentage |
|---|---|---|
| Azithromycin, Clindamycin | 11 | 29% |
| No Antibiotics | 7 | 18% |
| Ampicillin, Azithromycin, Clindamycin | 5 | 13% |
| Ampicillin, Azithromycin | 3 | 8% |
| Azithromycin, Clindamycin, Doxycycline | 3 | 8% |
| Clindamycin | 2 | 5% |
| Azithromycin | 2 | 5% |
| Ampicillin, Azithromycin, Clindamycin, Doxycycline | 2 | 5% |
| Ampicillin, Azithromycin, Clindamycin, Minocycline | 1 | 3% |
| Ampicillin | 1 | 3% |
| Azithromycin, Clindamycin, Doxycycline, Minocycline | 1 | 3% |
| Grand Total | 38 | 100% |
Biofilms in acne
The biofilm-forming capacity of the isolates was evaluated and compared to that of S. epidermidis, which served as a positive control.
The isolates were graded based on their capacity to produce biofilms as strong (S), moderate (M), and weak (W).
Sixty-three percent of C. acnes was found to have weak biofilm formation capability. As depicted in Table 4, only 37% of the isolates possessed a moderate ability to form biofilms which was much less than the percentage showing antibiotic resistance Thus we could conclude that the capacity to form biofilms is not necessarily indicative of the antibiotic resistance.
| Biofilm capacity | Number of isolates | Percentage distribution (%) |
|---|---|---|
| Moderate | 14 | 36.8 |
| Weak | 24 | 63.2 |
| Total | 38 | 100 |
More than 60% of the samples had resistance to more than two types of antibiotics and a weak capacity to form biofilms. There was no statistical significance between the biofilm-forming capacity and the number of antibiotics an isolate was resistant to (P = 0.761) [Tables 2 and 4]. Consequently, this study indicates that the capacity for biofilm formation is not necessarily proportional to the number of antibiotics to which a sample is resistant.
Discussion
Antibiotics have been the cornerstone of acne treatment for decades, working primarily in two ways: first, as an anti-inflammatory agent and second, as an antimicrobial agent.8 Antibiotics must possess lipophilic qualities to penetrate the lipid-rich sebaceous gland.
Global reports have indicated shifts in antibiotic susceptibility patterns, with the prescribing practices of medical professionals significantly shaping the landscape of antibiotic resistance. Incorrect dosages, inadequate treatment durations, and prescription practices can contribute to the emergence of antibiotic resistance.
In our study, we found that minocycline and doxycycline were the antibiotics with the most sensitivity followed by ampicillin, clindamycin, and azithromycin.
An intriguing pattern emerged in our investigation: 73.7% of bacteria were resistant to Azithromycin, 65.8% were resistant to clindamycin and nearly 29% were resistant to both. Research by Ross et al. (2003) across Europe revealed that Spain had the highest levels of resistance to clindamycin and erythromycin.9 In 2016, a study conducted by Sardana et al, reported 100% resistance to azithromycin, 98% to erythromycin, 90.4% to clindamycin, and 44.2% resistance to doxycycline, with minocycline showing the least resistance.10 In Malta, a study by Mercieca et al. (2020) discovered 47.4% population had resistance to azithromycin.11 Notably, in both domestic and international studies, minocycline regularly emerges as the most sensitive drug [Table 5]. Numerous antibiotic susceptibility studies indicate an evolving global pattern of antibiotic resistance. However, analysing these researches necessitates consideration of limitations, such as the difficulty in comparing data due to the variations in methodologies used for susceptibility studies.
| Prevalence of antibiotic resistance in acne – world-wide comparison (%) | ||||||
|---|---|---|---|---|---|---|
| Study | Location | Clin | Doxy | Mino | Azi | Amp |
| Mercieca et al (2020)11 | Malta | 42.1 | 5.3 | 0 | 47.4 | NS |
| Rodriguez-Cavallini et al. (2004)22 | Costa Rica | 23 | NS | NS | NS | 27 |
| Schafer et al. (2013)23 | Chile | 7.5 | 0 | NS | NS | NS |
| Mendoza et al. (2013)24 | Colombia | 15 | 9 | 1 | NS | NS |
| Galvan Perez et al. (2002)25 | Spain | 51.8 | NS | 2.3 | NS | NS |
| Ross et al. (2003)9 | Spain | 90 | NS | 0 | NS | NS |
| Greece | 75 | NS | NS | NS | NS | |
| Hungary | 40 | NS | NS | NS | NS | |
| Italy | 58 | NS | NS | NS | NS | |
| UK | 50 | NS | NS | NS | NS | |
| Sweden | 45 | NS | NS | NS | NS | |
| Bettoli et al. (2006)26 | Italy | 37.6 | NS | 1.1 | NS | NS |
| Dumont-Wallon et al. (2010)27 | France | NS | 100 | NS | NS | NS |
| Tan et al. (2007)1 | Singapore | 7.5 | 3.4 | 1.7 | NS | NS |
| Ishida et al. (2008)28 | Japan | 8.3 | NS | 0 | NS | NS |
| Zandi et al. (2011)29 | Iran | 43 | NS | NS | NS | NS |
| Luk et al. (2013)30 | Hong Kong | 53.5 | 16.3 | 16.3 | NS | NS |
| Sardana et al. (2016)10 | India | 90.4 | 44.2 | 1.9 | 100 | NS |
| Nakase et al. (2017)31 | Japan | 38.6 | 0 | 0 | 44.3 | NS |
| Zhu et al. (2019)32 | China | 55.5 | 1.3 | NS | 58.6 | NS |
| Our Study (2024) | India | 65.8 | 15.8 | 5.3 | 73.7 | 31.6 |
NS: not studied, CLIN: clindamycin, DOXY: doxycycline, MINO: minocycline, AZI: azithromycin, AMP: ampicillin.
The sampling techniques used in different investigations vary greatly, with some using expressed material and others using surface swabs. Lack of standardized data collection protocols, sampling methods, and antibiotic susceptibility testing, make cross-study comparisons difficult.
While hyperseborrhoea, hyperkeratinisation, sebaceous gland follicle occlusion, and C. acnes colonisation have historically been viewed as pivotal in acne pathogenesis, recent years have systematically challenged this notion.12
Acne vulgaris is increasingly being connected to the interaction of skin bacteria and host immunity.13 Despite the lack of a direct link between C. acnes and acne, addressing C. acnes remains a key component of acne treatments. Antibiotics have been a mainstay due to their combination of bactericidal and anti-inflammatory effects. Antibiotics, both topical and systemic, are routinely utilised and are normally prescribed for three to four months.14–15
Antibiotic overuse has resulted in therapeutic failures, treatment-resistant acne, impaired skin microbiome, and increased opportunistic infection risks. In the 1970s, Leyden et al. addressed antibiotic resistance concerns in acne vulgaris.16
Antibiotic resistance in acne must be considered when experiencing diminished responses, absence of response, or relapses. Early detection of antibiotic failure is critical for reducing needless and excessive antibiotic use.
Recent research attributes C. acnes antibiotic resistance primarily to biofilm formation and genetic/biochemical plasticity.
Biofilms are protective matrices made up of extracellular polysaccharides, proteins, lipids, and DNA that allow bacteria to survive in harsh environments.17
Burkhart and Burkhart established the concept of biofilms in acne in 2007.18–20 Subsequent research revealed that C. acnes biofilms stimulate proliferation, improve follicular adherence and virulence and increase pro-inflammatory and lipase activity. However, evidence of its clinical application remains limited.21
In our study, we assessed isolates’ antibiotic susceptibility alongside their biofilm-forming capacity. Comparatively, only 63.2% displayed weak biofilm-forming ability against S. epidermidis biofilm forming ability as control. Holmberg et al. and Mongaret et al separately demonstrated deeper infections to possess greater biofilm-forming potential than commensal acne-derived isolates.6,22
Interestingly, four isolates demonstrated resistance to four distinct antibiotic classes. Of these, two isolates exhibited weak biofilm-forming capabilities, while the remaining two displayed moderate biofilm formation capacity. Correlation analysis between antibiotic resistance and biofilm formation capacity revealed no statistically significant association.
Limitations
The study is a single centre study and it is limited by its sample size. Long-term follow-up was not done; hence the correlation between the antibiotic resistance and treatment outcomes has not been identified. The antibiogram performed in this study is only for C. acnes. This data is not representative for other species, such as S. epidermidis.
Conclusion
Patients with acne vulgaris have historically relied on antibiotics as their primary therapeutic choice. Antibiotic resistance has emerged as a result of its prolonged and irrational usage.
It is concerning that the global pattern of antibiotic resistance is constantly evolving. The absence of standardized sample collection and isolation protocols can further contribute to the heterogeneity between research.
A significant amount of research has been done on antibiotic resistance in acne. One of the possibilities that were proposed centred on the formation of a biofilm by C. acnes. The potential of C. acnes to generate biofilms has been demonstrated; however, our findings suggest that its role in acne is not significant.
Due to the restricted ability of the cutaneous C. acnes to form biofilms, its contribution to antimicrobial resistance in acne vulgaris is likely to be modest or limited. It is important to consider alternative mechanisms such as genetic or biochemical plasticity that may contribute to antibiotic resistance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
IADVL postgraduate thesis grant 2020.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Reference
- A global perspective on the epidemiology of acne. Br J Dermatol. 2015;172(Suppl 1):3-12.
- [CrossRef] [PubMed] [Google Scholar]
- The natural history of cutaneous propionibacteria, and reclassification of selected species within the genus Propionibacterium to the proposed novel genera Acidipropionibacterium gen. nov., Cutibacterium gen. nov. and Pseudopropionibacterium gen. nov. Int J Syst Evol Microbiol. 2016;66:4422-32.
- [CrossRef] [PubMed] [Google Scholar]
- Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: A brief look at the latest updates. J Eur Acad Dermatol Venereol. 2018;32(Suppl 2):5-14.
- [CrossRef] [PubMed] [Google Scholar]
- Heterogeneity and antibiotic resistance in Propionibacterium acnes isolates and its therapeutic implications: Blurring the lines between commensal and pathogenic phylotypes. Dermatol Ther. 2016;29:451-4.
- [CrossRef] [PubMed] [Google Scholar]
- A Myrtus communis extract enriched in myrtucummulones and ursolic acid reduces resistance of Propionibacterium acnes biofilms to antibiotics used in acne vulgaris. Phytomedicine. 2016;23:307-15.
- [CrossRef] [PubMed] [Google Scholar]
- Biofilm formation by Propionibacterium acnes is a characteristic of invasive isolates. Clin Microbiol Infect. 2009;15:787-95.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis and presentation of cumulative antimicrobial susceptibilty test data; Approved guideline (4th ed). Pennsylvania: Clinical and laboratory standards institute; 2014.
- An overview of topical antibiotics for acne treatment. Dermatology. 1998;196:130-4.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic-resistant acne: Lessons from Europe. Br J Dermatol. 2003;148:467-78.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-sectional pilot study of antibiotic resistance in propionibacterium acnes strains in Indian acne patients using 16s-RNA polymerase chain reaction: A comparison among treatment modalities including antibiotics, benzoyl peroxide, and isotretinoin. Indian J Dermatol. 2016;61:45-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The antibiotic susceptibility profile of cutibacterium acnes in maltese patients with acne. J Clin Aesthet Dermatol. 2020;13:11-6.
- [PubMed] [PubMed Central] [Google Scholar]
- Potential role of the microbiome in acne: A comprehensive review. J Clin Med. 2019;8:987.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Skin microbiome and acne vulgaris: Staphylococcus, a new actor in acne. Exp Dermatol. 2017;26:798-803.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-73.e33.
- [CrossRef] [PubMed] [Google Scholar]
- Propionibacterium acnes colonization in acne and nonacne. Dermatology. 1998;196:55-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic resistance in acne: Mechanisms, complications and management. Am J Clin Dermatol. 2020;21:813-9.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic-resistant Propionibacteria acnes may not be the major issue clinically or microbiologically in acne. Br J Dermatol. 2003;148:365-6.
- [CrossRef] [PubMed] [Google Scholar]
- Expanding the microcomedone theory and acne therapeutics: Propionibacterium acnes biofilm produces biological glue that holds corneocytes together to form plug. J Am Acad Dermatol. 2007;57:722-4.
- [CrossRef] [PubMed] [Google Scholar]
- Biofilm formation by Propionibacterium acnes is associated with increased resistance to antimicrobial agents and increased production of putative virulence factors. Res Microbiol. 2007;158:386-92.
- [CrossRef] [PubMed] [Google Scholar]
- Cutibacterium acnes biofilm study during bone cells interaction. Microorganisms. 2020;8:1409.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Etiología bacteriana y susceptibilidad a antibióticos en pacientes con acné. Revista Biomédica. 2004;15:101-6.
- [PubMed] [Google Scholar]
- Antimicrobial susceptibility and genetic characteristics of Propionibacterium acnes isolated from patients with acne. Int J Dermatol. 2013;52:418.
- [CrossRef] [PubMed] [Google Scholar]
- Antimicrobial susceptibility of Propionibacterium acnes isolates from acne patients in Colombia. Int J Dermatol. 2013;52:688-92.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic resistance of Propionibacterium acnes in patients treated for acne vulgaris in Malaga. Actas Dermosifiliogr. 2002;93:271-5.
- [Google Scholar]
- Antibiotic resistance of propionibacteria. Four years’ experience of a large number of cases in Italy. Dermatology. 2006;212:206-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial resistance in French acne patients. Int J Dermatol. 2010;49:283-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antimicrobial susceptibilities of Propionibacterium acnes isolated from patients with acne vulgaris. Microbiol Immunol. 2008;52:621-4.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of microbial agents of acne vulgaris and Propionibacterium acnes antibiotic resistance in patients referred to dermatology clinics in Kerman, Iran. Jundishapur J Microbiol. 2011;4
- [Google Scholar]
- Antibiotic-resistant Propionibacterium acnes among acne patients in a regional skin centre in Hong Kong. J Eur Acad Dermatol Venereol. 2013;27:31-6.
- [CrossRef] [PubMed] [Google Scholar]
- Antimicrobial susceptibility and phylogenetic analysis of Propionibacterium acnes isolated from acne patients in Japan between 2013 and 2015. J Dermatol. 2017;44:1248-54.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotic susceptibility of Propionibacterium acnes isolated from patients with acne in a public hospital in Southwest China: Prospective cross-sectional study. BMJ Open. 2019;9:e022938.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







