Translate this page into:
Correlating pemphigus disease area index (PDAI) severity categories with oral disease severity score (ODSS) in oral mucosal pemphigus - A pilot study
Corresponding author: Dr. Arun Dev Sharma, Department of Oral Medicine and Radiology, Government College of Dentistry, Indore, India. drarundev@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma AD, Reddy P, Parihar A, Tosh S, Mandlik R, Yadav N. Correlating pemphigus disease area index (PDAI) severity categories with oral disease severity score (ODSS) in oral mucosal pemphigus - A pilot study. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1527_2024
Abstract
Background
Pemphigus vulgaris is a chronic autoimmune blistering disorder that primarily affects the oral mucosa, with over two-thirds of patients developing oral lesions, often preceding skin involvement by weeks or months. The Oral Disease Severity Score (ODSS) provides a detailed, region-specific assessment of oral lesions, facilitating regular monitoring and treatment response. However, it lacks a comprehensive severity evaluation cut-offs needed for systemic therapy decisions.
Aim
To categorise oral pemphigus severity into moderate, significant, and extensive using ODSS.
Methods
The study included 25 oral pemphigus patients, confirmed histopathologically or by anti-DSG 3, evaluated severity using ODSS and PDAI scales, with statistical significance analysed between the scores and categories.
Results
The study comprised 25 subjects with a mean age of 47.48 years (±15.692), including 8 males (32%) and 17 (68%) females. The mean ODSS and PDAI scores were 30.12 (±13.902) and 20.72 (±14.105), respectively. A highly significant positive correlation (r=0.962, p-value <0.001) was observed between PDAI and ODSS scores. An AUC value (>0.8) confirmed ODSS’s good discriminating ability, categorising oral pemphigus severity: <21.5 as moderate, 21.5–48.5 as significant, and >48.5 as extensive, per PDAI criteria.
Limitation
Small sample size is the major limitation of this study.
Conclusion
This study proposes severity categories for ODSS for oral pemphigus, allowing it to be used for personalised treatment decisions.
Keywords
Disease severity
oral pemphigus
pemphigus disease area index
oral disease severity score
Introduction
Pemphigus is a chronic autoimmune mucocutaneous blistering disorder where autoantibodies, primarily IgG1 and IgG4 subclasses, target desmosomal proteins (Dsg1 and Dsg3) essential for cellular adhesion in epithelial and mucosal layers. This disruption of desmosomal integrity results in acantholysis and the formation of intraepithelial blisters.1 Pemphigus manifests as pemphigus vulgaris (PV), pemphigus foliaceus, and paraneoplastic pemphigus. PV affects the deeper layers of the epidermis and mucosa, whereas pemphigus foliaceus primarily involves the superficial epidermal layers, particularly the granular layer.2 Paraneoplastic pemphigus, on the other hand, is associated with underlying lymphoid neoplasms, often complicating its clinical presentation.3 PV is categorised into three clinical subgroups: mucosal dominant, mucocutaneous, and cutaneous types.4 The PDAI effectively assesses disease severity and classifies patients into moderate, significant, and extensive categories based on skin and mucosal involvement. However, using the PDAI to score oral-only cases is time-consuming and shows low inter- and intra-observer reliability compared to other oral disease scoring systems like the ODSS.5 The ODSS is effective for evaluating oral lichen planus and oral pemphigus, but it lacks severity grading for categorising patients into moderate, significant, and extensive categories. To address the challenge of assessing disease severity in patients with oral pemphigus, we conducted this study to assign severity cut-off scores for ODSS using PDAI as anchor.
Methods
The study was conducted at the Department of Oral Medicine and Radiology, Government college of dentistry, Indore, Madhya Pradesh aimed to assess the clinical manifestations and severity of oral pemphigus over a two-year period. Ethical approval was granted by the Institutional Ethics Committee (Certificate No. 234/IEC/SS/2024, dated 08/04/2024). The study included PV patients with pure oral mucosa involvement. A total of 25 patients met the inclusion criteria during the study period. The diagnosis in these patients was confirmed by histopathological examination and anti-desmoglein 3 (Dsg3) antigen positivity using ELISA. In selected cases, only anti-Dsg3 antibody levels were quantified, while immunofluorescence (IF) on biopsy samples was not conducted. Oral lesions in these pemphigus patients were mostly present as irregular erosions or superficial ulcerations, with the most common site being the buccal mucosa. Nikolsky’s sign is a phenomenon characterized by epithelial desquamation as a result of slight pressure or rubbing the skin or oral mucosa.it can best seen in gingiva of the affected patients. Along with diagnostic tests, we also obtained a comprehensive history and performed a detailed clinical examination to rule out other diagnoses. On the first visit, PDAI and ODSS scales were used to assess the severity of the oral lesions. The PDAI scores were then utilised to categorise the ODSS-scored patients into moderate [Figures 1a and 1b], significant [Figures 2a, 2b and 2c], and extensive [Figures 3a, 3b and 3c].

- (Moderate category) oral erosions on the lower lip.

- (Moderate category) oral ulcers on the right buccal mucosa.

- (Significant category) lower labial mucosa, showing multiple small ulcers.

- (Significant category) oral ulcers on the left retromolar pad area and the posterior part of the buccal mucosa.

- (Significant category) oral ulcers on the floor of the mouth and ventral surface of the tongue.
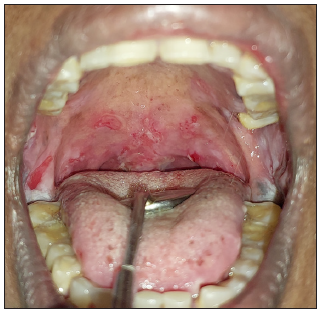
- (Extensive category) palatal ulcers along with the involvement of the bilateral retromolar pad area.
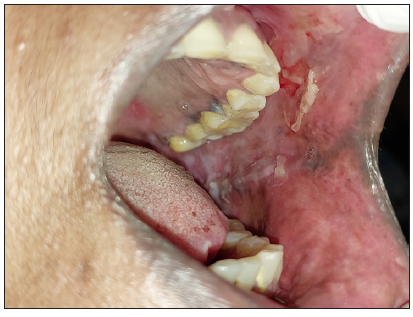
- (Extensive category) oral ulcers on the left buccal mucosa and part of the vestibule.

- (Extensive category) oral ulcers on the floor of the mouth and ventral surface of the tongue.
Statistical Analysis
Data was analysed using SPSS v25.0 (IBM, Chicago). The Shapiro-Wilk test was used to assess the normality of the data distribution. The correlation between PDAI and ODSS score was assessed using Pearson’s correlation coefficient. AUROC curve was plotted, cut was evaluated and sensitivity, specificity was assessed with respect to the calculated cut off. Descriptive statistics included frequencies, percentages, means (±SD), or medians (IQR). Categorical variable comparisons were evaluated using the Chi-square test, with significance at p < 0.05.
Results
The study was conducted among 25 subjects with a mean age of 47.48 ± 15.69 years. Remarkably, the distribution of age and gender closely resembled the findings reported by Ariyawardana A. et al in 2005.6 Among the subjects, 8 (32%) were males, and 17 (68%) were females. The mean ODSS and PDAI scores were 30.12 ±13.902 and 20.72 ± 14.105, respectively. On assessing the correlation between PDAI scores and ODSS scores, a statistically significant, strong positive correlation was found [r= 0.962, p <.001]. This finding supports the alignment of PDAI and ODSS in assessing oral pemphigus severity, validating their reliability in clinical practice.
Data illustrating the distribution of oral pemphigus patients across severity categories based on the PDAI scoring system is depicted in Table 1.
| PDAI category | Number of subjects | Percentage |
|---|---|---|
| Moderate (0-15) | 9 | 36% |
| Significant (16-45) | 14 | 56% |
| Extensive (>45) | 2 | 8% |
| Total | 25 | 100% |
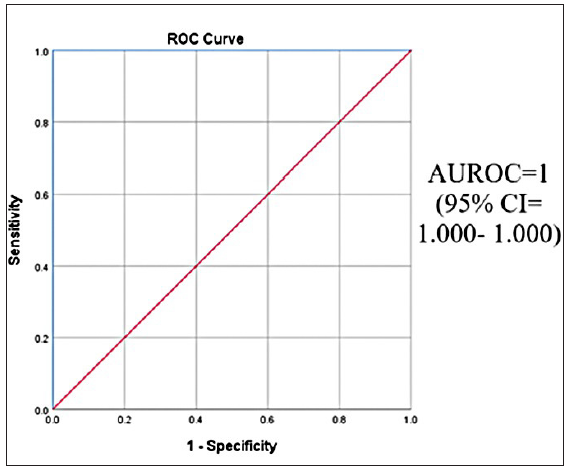
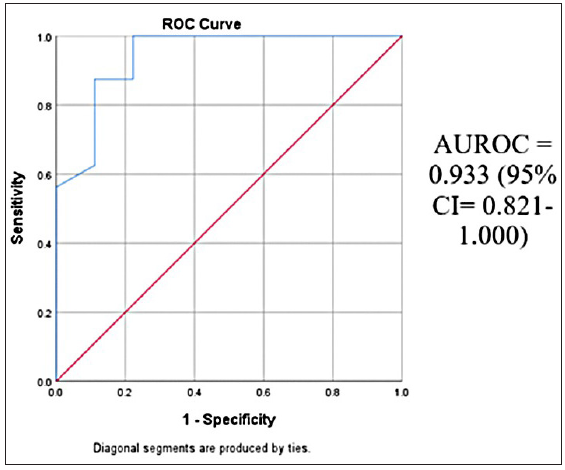
The Area under the receiver operating curve (AUROC) value >0.8 demonstrates the good discriminatory ability of ODSS in differentiating between severity grades of pemphigus [Table 2].
| PDAI category | AUROC | 95% confidence interval |
|---|---|---|
| Moderate-significant | 0.933 | 0.821-1.000 |
| Significant-extensive | 1.000 | 1.000-1.000 |
The established cut-off values for ODSS facilitate the categorisation of pemphigus severity based on the PDAI [Table 3]. An ODSS score <21.5 indicates moderate pemphigus, scores between 21.5 and 48.5 denote significant pemphigus, and score >48.5 indicates extensive pemphigus [Table 4]. The Receiver Operating Characteristic (ROC) curve [Figure 4] demonstrates the ODSS’s discriminatory ability, balancing sensitivity and specificity to differentiate between moderate and significant pemphigus severity effectively.
| New ODSS category | Cut off | Sensitivity | Specificity |
|---|---|---|---|
| Moderate-significant | 21.5 | 100% | 77.8% |
| Significant-extensive | 48.5 | 100% | 95.2% |
| ODSS score | Oral pemphigus severity categories |
|---|---|
| <21.5 | Moderate |
| 21.5-48.5 | Significant |
| >48.5 | Extensive |
- ROC curve of ODSS to distinguish between moderate and significant pemphigus based on PDAI.
The ROC curve illustrates ODSS’s effectiveness in identifying moderate pemphigus (sensitivity) while minimising the misclassification of significant pemphigus cases (specificity). The ROC curve [Figure 5] highlights ODSS’s ability to differentiate between significant and extensive pemphigus based on the PDAI, visualising the balance between sensitivity and specificity across various ODSS thresholds.
- ROC curve of ODSS to distinguish between significant and extensive pemphigus based on PDAI.
Discussion
The oral mucosa is commonly affected in PV, with over two-thirds of patients experiencing oral lesions during disease progression. In more than half of cases, oral symptoms appear as initial manifestations, often preceding skin involvement by weeks or months.7 This highlights the critical need for thorough oral mucosal examination in suspected PV cases, as early detection and timely treatment are essential for effective disease management. In these cases, a rapid and reliable scoring tool for oral-only manifestations is necessary. For this purpose, ODSS is the best parameter as it utilises the extent of involvement across all anatomical sites in the oral cavity, making it more efficient and less time-consuming during initial and follow-up visits. The ODSS includes a functional assessment of oral symptoms by incorporating a pain score, which is absent in the PDAI. A 2018 study showed that the ODSS demonstrated superior inter- and intra-observer reliability compared to the Physician’s Global Assessment (PGA), Autoimmune Bullous Skin Disorder Intensity Score (ABSIS), and PDAI, although it did not include severity gradings for further classification.5 Treatment for oral pemphigus typically involves topical and systemic corticosteroids, with mild cases receiving 0.5 mg/kg/day and moderate-severe cases requiring 1.0 mg/kg/day.8 Incorporating severity grading for oral pemphigus within ODSS will enable more personalised treatment strategies, enhancing the precision of therapeutic interventions and improving patient outcomes. Our study aims to identify the disease severity cut-offs for ODSS corresponding to PDAI severity categories.
Creating a composite PDAI score that incorporates ODSS measurements for oral lesions would allow for a balanced scoring system. By combining lesion count, size, and functional impairment into a single composite score, this adapted PDAI would provide a comprehensive overview of both the physical and functional burden of oral lesions during initial and follow-up visits. In our study, the mean ODSS and PDAI scores were 30.12 ± 13.902 and 20.72 ± 14.105, respectively. A highly significant correlation (r = 0.962, p < 0.001) was observed between ODSS and PDAI scores, indicating a strong association in assessing oral pemphigus severity. This underscores ODSS’s validity and reliability as a quick alternative to PDAI for evaluating disease severity in oral PV. The demonstrated superior inter- and intra-observer reliability of ODSS further supports its clinical utility, contributing to effective management and treatment of the condition.
Limitations
The study’s small sample size of 25 patients may limit the generalisability of its findings. Focusing solely on oral pemphigus and excluding patients with extraoral involvement restricts the scoring system’s applicability.
Conclusion
This study introduces the integration of severity categories into the ODSS for oral pemphigus, enhancing the accuracy of patient evaluation and management. By incorporating PDAI gradings, a more comprehensive assessment method is established. The strong correlation between ODSS and PDAI scores supports effective clinical practice. While the findings improve treatment decision-making, the small sample size and cross-sectional design limit generalisability and long-term progression capture. Future multicentre studies are essential to validate these findings. The scores of both the index are being evaluated for all the patients and then the grades of PDAI are integrated in ODSS scoring system to create a new grading for oral pemphigus vulgaris. so the integrated score and comprehensive score are used in the text.
Ethical approval
The research/study was approved by the Institutional Review Board at Government College of Dentistry, Indore, MP, India, number 234/IEC/SS/2024, dated 08/04/2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pemphigus in the XXI century: New life to an old story. Autoimmunity. 2006;39:521-30.
- [CrossRef] [PubMed] [Google Scholar]
- Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med. 1990;323:1729-35.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus. J Am Acad Dermatol. 2008;58:1043-6.
- [CrossRef] [PubMed] [Google Scholar]
- An oral disease severity score validated for use in oral pemphigus vulgaris. Br J Dermatol. 2018;179:872-81.
- [CrossRef] [PubMed] [Google Scholar]
- Oral pemphigus vulgaris in children and adolescents: A review of the literature and a case report. Int J Paediatr Dent. 2005;15:287-93.
- [CrossRef] [PubMed] [Google Scholar]
- Burket’s oral medicine (13th edition). John Wiley & Sons, Inc.; 2022. p. :43-5.
- Diagnosis and management of pemphigus: Recommendations of an international panel of experts. J Am Acad Dermatol. 2020;82:575-585.e1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







