Translate this page into:
Bridging gaps in pediatric dermatology via telemedicine: An analytical cross-sectional study on 961 children in resource-limited areas of North India using the e-Sanjeevani 2.0 platform
Corresponding author: Dr. Richa Gupta, Department of Telemedicine, Postgraduate Institute of Medical Education and Research, Chandigarh, rg.telepgi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vashisht KR, Sahu P, Mandula PP, Dash N, Agarwal A, Gupta R, et al. Bridging gaps in pediatric dermatology via telemedicine: An analytical cross-sectional study on 961 children in resource-limited areas of North India using the e-Sanjeevani 2.0 platform. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1223_2024
Abstract
Background
Pediatric tele-dermatology (PTD) offers a potential solution for delivering specialised dermatological care to children in remote areas.
Objectives
To evaluate the scope, utilisation, receptivity, and factors influencing the optimisation of PTD practice within the context of a developing country’s demographic.
Methods
The study analysed 961 PTD consultations over six months, conducted in underserved areas of North India via an assisted telemedicine platform, e-Sanjeevani 2.0. Data were gathered cross-sectionally through standardised forms, complemented by a retrospective survey to capture the perceptions of referring healthcare providers (RHPs). Patient clinico-demographics and various consultation characteristics were assessed for their impact on clinical decision-making.
Results
Among the 961 cases studied (median age 5 years, IQR: 2–11; 52.1% female), the majority consisted of infections, infestations, and dermatitis, 1.35% cases were acute/emergency dermatoses managed empirically, and only 4.47% required referral. Friedman test revealed highly significant differences in perceived helpfulness amongst the four consultation variables (p<0.001) – image quality being the most helpful, followed by audiovisual/text interaction, multiple images, and past/medical/family history. Wilcoxon Signed Ranks tests indicated significant differences in perceived helpfulness between each pair of variables (p<0.001). The RHP survey reflected a strong endorsement of the process and a high perceived parent/guardian satisfaction rate (4.47 ± 0.87 on a 5-point scale).
Limitations
The study did not evaluate diagnostic or management concordance due to a lack of in-person evaluation. Other limitations included a low follow-up rate, short duration of study that may have missed seasonal variations in paediatric dermatoses. Additionally, clinical outcomes, cost-effectiveness, and technical factors such as connectivity and video quality were not assessed.
Conclusion
The findings support the use of real-time PTD to manage less complex, non-procedural cases, reduce in-person consultations, and improve access to paediatric dermatology care in resource-constrained settings. High-quality images and effective audiovisual communication are pivotal for its optimisation. The service had clinical and educational value and was well-received by parents and providers. The integration of eSanjeevani into India’s healthcare infrastructure offers a functional foundation for larger scale expansion of PTD services. Further studies in diverse settings are needed to identify operational barriers to broader implementation and evaluate diagnostic accuracy through direct comparisons with in-person evaluations.
Keywords
eSanjeevani
paediatric dermatology
paediatric teledermatology
paediatric teledermatology
teledermatology
telemedicine
Introduction
Telemedicine integration across various specialties has surged globally, bridging healthcare gaps by reducing logistics, cutting costs, and enabling timely care.1 Paediatric dermatology, often reliant on urban-based specialists with limited rural access, differs from adult dermatology in disease prevalence, presentation, and the need for specialised knowledge. Barriers to dermatology are pronounced in children due to subtler symptoms, varied morphology, and reliance on parental support.2–5 Access is further constrained in underserved communities by geographic, financial, language, and cultural barriers; making paediatric teledermatology (PTD) a promising solution.6–10
This six-month analytical cross-sectional study explores factors that optimise PTD care in resource-limited settings using e-Sanjeevani 2.0 platform— a public health telemedicine initiative by the Government of India, operating on a ‘hub-and-spoke’ model, connecting referring healthcare providers (RHPs) at peripheral centres to specialists at higher centres for real-time, secure ‘provider-to-provider’ interactions through audiovisuals, images, and texts11,12 [Figure 1]. Integrating basic examinations performed by RHPs with detailed assessments by specialists, including the generation of e-prescriptions, e-Sanjeevani is the largest documented telemedicine initiative in primary healthcare worldwide.13,14 This study, conducted at a tertiary centre ‘hub’ for cases from Haryana, examines the scope, feasibility, utilisation, clinico-demographics, operational aspects, and provider perceptions of delivering dermatological care to children via telemedicine.
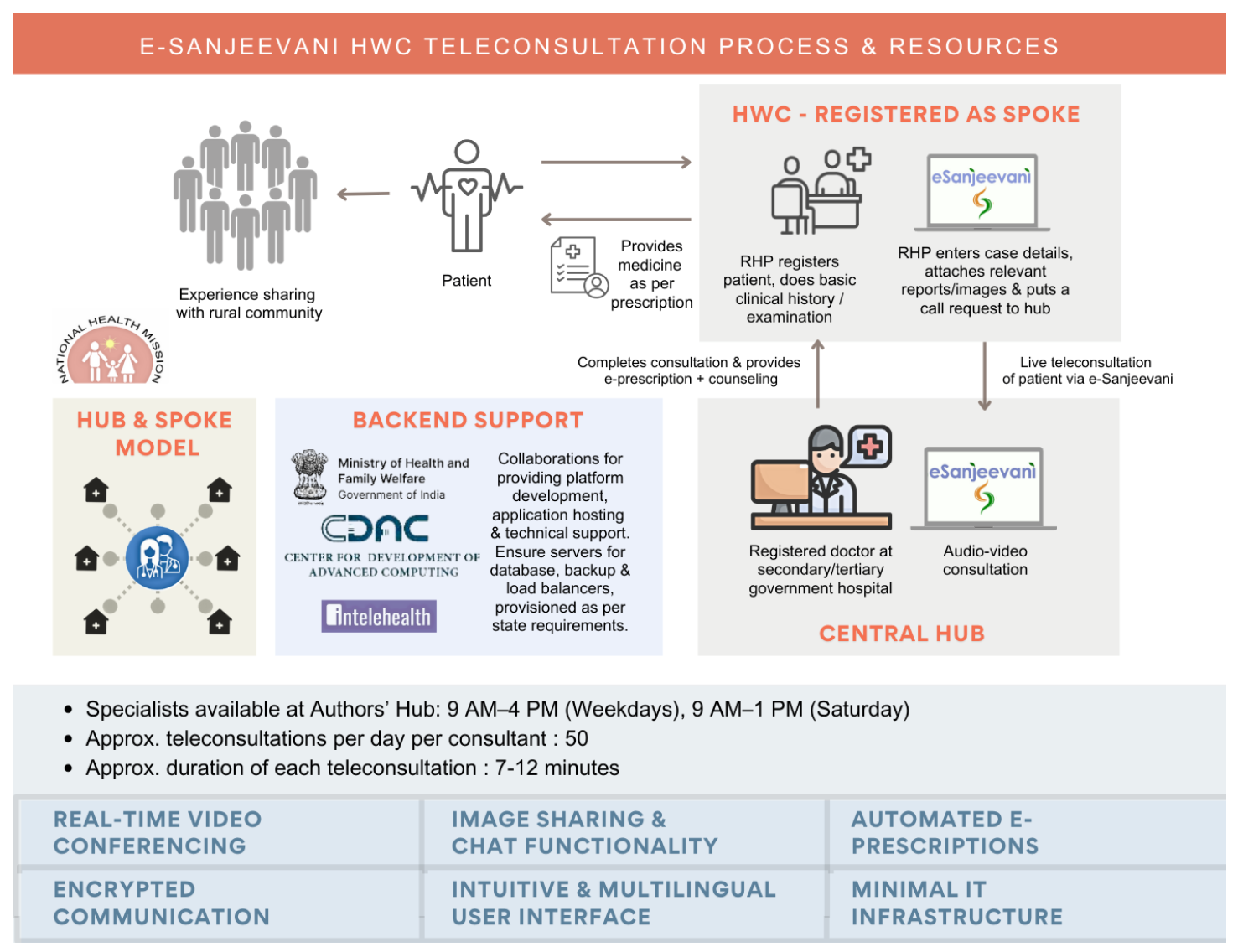
- Overview of e-Sanjeevani’s hub-and-spoke model, where Referring Healthcare Providers (RHPs) at the peripheral ‘spokes’ such as Health and Wellness Centres (HWCs), connect patients to specialists at higher centres via real-time teleconsultation.
Methods
Study design & Population: Data were gathered cross-sectionally from individual PTD consultations, complemented by a retrospective survey capturing RHPs’ overall experiences and perceptions. Participants ranged from neonates to 18-year-olds, seeking remote consultations for dermatological conditions, recruited via consecutive sampling at the authors’ tertiary centre over six months (August 2023 to January 2024). Cases lacking clear photographs or provisional diagnoses were excluded. The study received ethical approval and adhered to the Declaration of Helsinki. Informed verbal consent was obtained from the parents/guardians before teleconsultations, as required by national telemedicine guidelines for consultations initiated by RHPs. The e-Sanjeevani 2.0 platform complies with relevant data protection regulations, and all data were anonymised.11,12
Data collection & Variables: Standardised data collection forms captured demographic details, consultation specifics, and provider perceptions. Consultation data were compiled by technical support into Excel sheets. Four consultation variables were assessed for their impact on physician confidence in diagnosis and management: image quality, multiple images, audiovisual/text interaction, and ancillary (past/medical/family) patient history. Acute/emergency cases managed empirically and those requiring referral were assessed. RHPs’ perspectives were evaluated via a retrospective Google form survey, assessing comfort with the service, educational benefits, and perceived parental/guardian satisfaction (1-5 scale) [Supplemental-data].
Statistical analysis: Analyses were performed using SPSS v22 (IBM Corp., Armonk, NY). Descriptive statistics were used to summarise the data. Friedman test assessed differences in perceived helpfulness, and pairwise comparisons were made using the Wilcoxon Signed Ranks test, considering p<0.05 as significant and p<0.001 highly significant.
Results
Demographics and clinical characteristics: The study included 961 children (median age: 5 years, IQR: 2–11; 52.1% female). Most diagnoses were infections and infestations, followed by dermatitis, while naevi and tumours were least common [Figure 2]. The follow-up rate for teleconsultations on the platform was 9.6%. Only 43 cases (4.47%) required in-person consultations for acute dermatoses, including 13 emergency/acute cases (1.35%), empirically managed per national telemedicine guidelines along with urgent referral for in-person care12 [Table 1].
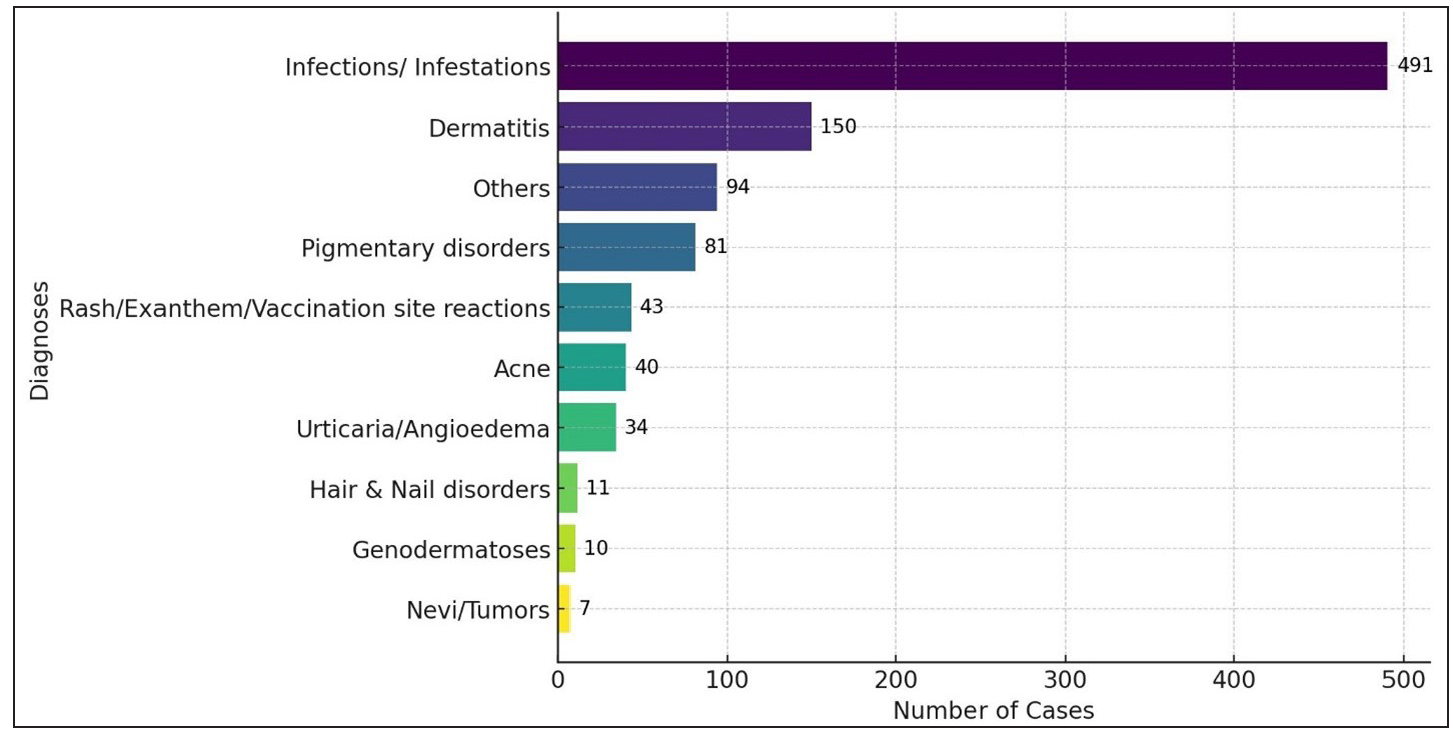
- Frequency distribution of broad diagnoses of paediatric teledermatology cases seen during the study period.
| Category | Cases (%) | Examples |
|---|---|---|
| Emergency/Acute Dermatoses managed empirically | 13 (1.35) | Angioedema, burns, Stevens-Johnson syndrome, omphalitis, neonatal candidiasis, staphylococcal scalded skin syndrome, acne fulminans |
| Referrals for in-person care | 43 (4.47) |
Acute Dermatoses: Same as above. Procedures: Warts, molluscum contagiosum, pyogenic granuloma, keloids/scars. Biopsy/Further evaluation: Mycetoma, scrofuloderma. Complex cases requiring in-person care: Ulcerated haemangiomas, rapidly progressive vitiligo, psychodermatoses (e.g., dermatitis artefacta, trichotillomania), concomitant malnutrition in acrodermatitis enteropathica, genodermatoses (e.g., epidermolysis bullosa, Peutz-Jeghers syndrome) |
Consultation characteristics: The helpfulness of consultation variables for PTD case management was rated on a three-point scale: (1)Not helpful—diagnosis and treatment were confidently made without it; (2)Somewhat helpful—contributory but not essential; (3)Very helpful—critical for diagnosis or treatment. Image quality was ‘very helpful’ in 79.1% of cases, followed by audiovisual/text interactions (50.1% rated ‘very helpful’). Multiple images were rated ‘somewhat helpful’ in 40.5% of cases, while ‘ancillary’ (past/medical/family) history was deemed ‘not helpful’ in 65.1% of cases [Table 2; Figures 3a,3b]. A Friedman test revealed significant differences in perceived helpfulness across the four consultation variables (χ2 (3, N=961) =1463.075, p<0.001). Wilcoxon Signed Ranks tests showed highly significant differences between each pair (p<0.001), with Image Quality being the most helpful, followed by Audiovisual/Text Interaction, Multiple Images, and Past/Medical/Family History [Table 3]. Although multiple images were rated as ‘somewhat helpful’ and ancillary history as ‘not helpful’ overall, they were particularly considered ‘very helpful’ for diagnoses like rashes, acne, vitiligo (multiple images), scabies and impetigo (ancillary history).
| Consultation Variable |
Helpfulness ratings 1 = not helpful (minimum) 2 = somewhat helpful 3 = very helpful (maximum) |
Helpfulness ratings Number of cases (% of cases) |
||||
|---|---|---|---|---|---|---|
| Mean rating ± SD | Median rating (range 1 to 3) | Not helpful | Somewhat helpful | Very helpful | Total cases | |
| Quality of image | 2.78 ± 0.442 | 3 | 11 (1.1%) | 190 (19.8%) | 760 (79.1%) | 961 (100%) |
| Multiple images | 1.85 ± 0.757 | 2 | 358 (37.2%) | 389 (40.5%) | 214 (22.3%) | 961 (100%) |
| Audiovisual/text interaction | 2.43 ± 0.625 | 3 | 70 (7.3%) | 410 (42.6%) | 481 (50.1%) | 961 (100%) |
| Past/ medical/ family history | 1.46 ± 0.685 | 1 | 626 (65.2%) | 229 (23.8%) | 106 (11%) | 961 (100%) |
SD: Standard deviation
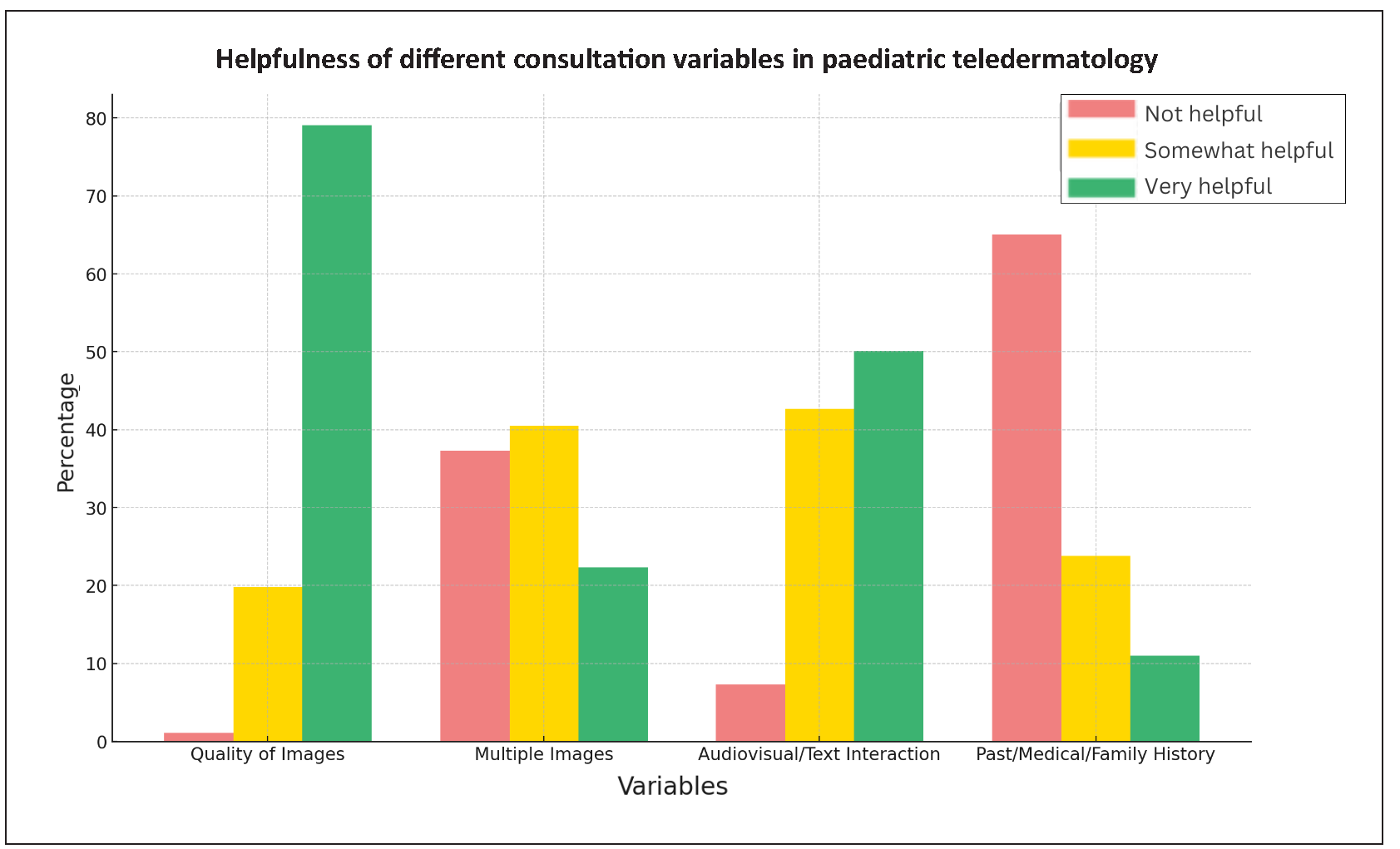
- Bar chart illustrating percentage of responses indicating how helpful each variable was in diagnosing and management of PTD cases.

- Crosstab Heatmap showing helpfulness ratings of consultation variables in PTD. (The y-axis represents consultation variables, and x-axis denotes their ratings. Each row sums to 100%, with the darkest cell indicating the most common response, highlighting the relative importance of each factor.) Bold indicates statistical significance.
| Comparison | Z value | p-value | More helpful variable |
|---|---|---|---|
| Quality of images vs. Multiple images | 22.846 | < .001 | Quality of images |
| Quality of images vs. Audiovisual/Text interaction | 13.156 | < .001 | Quality of images |
| Quality of images vs. Past/medical/family History | 24.859 | < .001 | Quality of images |
| Audiovisual/Text Interaction vs. Multiple Images | 15.909 | < .001 | Audiovisual/Text interaction |
| Multiple Images vs. Past/Medical/Family History | 11.602 | < .001 | Multiple images |
| Audiovisual/Text Interaction vs. Past/Medical/Family history | 22.984 | < .001 | Audiovisual/Text interaction |
RHP perception: Links to the online (Google Form) survey were sent to the 185 RHPs who had consulted the hub for PTD cases over six months, of which 107 responded (57.83% response rate). RHPs viewed the service positively, noting substantial clinical and educational value [Table 4]. The high mean satisfaction rating (4.47 on a 1-5 scale) with a low standard deviation (0.87) demonstrated consistent satisfaction among parents/guardians, as reported by RHPs. Chi-square tests showed no significant differences in comfort, outcomes perception, recommendations, or satisfaction across different RHPs and centre types, suggesting uniformly positive perceptions of PTD. Centre types follow India’s primary healthcare hierarchy by population size, ensuring equitable care [Figure 4].
| Parameter | Result | Inference |
|---|---|---|
| Comfort with platform | 100% Comfortable | All providers were comfortable using the telemedicine platform for PTD cases. |
| Parent/Guardian satisfaction | Mean: 4.47 (on a scale of 1-5), SD: 0.87 | High and consistent satisfaction levels among parents/guardians. |
| Perception of treatment outcomes amongst RHPs | 84.11% believe online is almost as good as in-person. | Majority were confident in PTD, some preferred in-person consultations. |
| Educational benefits of service | 98.13% enabled better management. | Nearly all providers feel better prepared to manage future cases. |
|
Recommendation of e-Sanjeevani for paediatric cases with skin concerns |
96.26% Would recommend, 3.74% Would not | Strong endorsement of the platform by providers. |
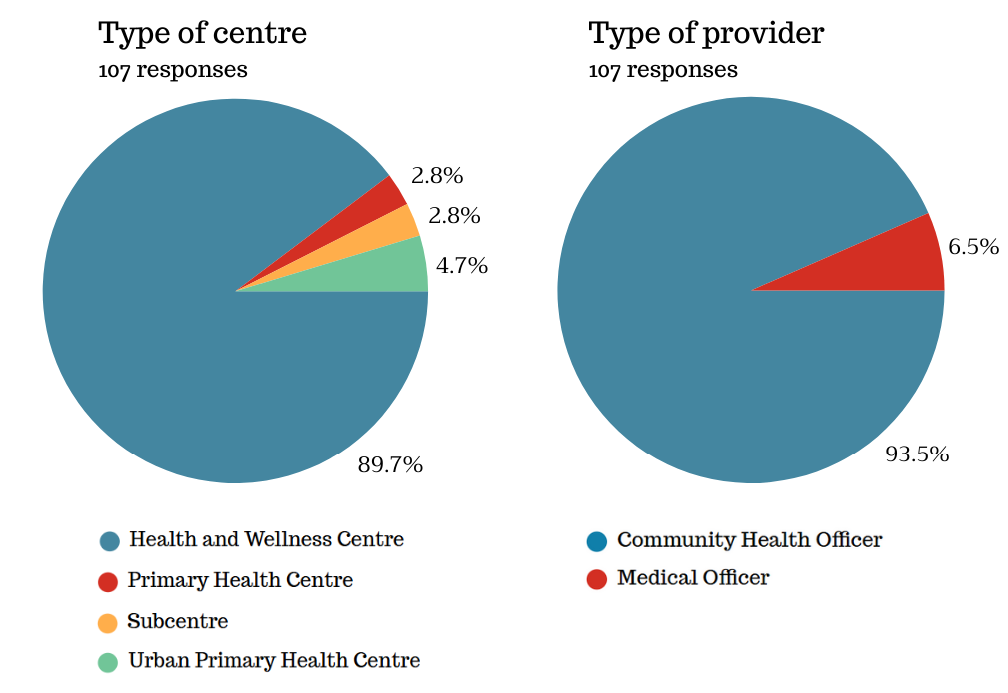
- Distribution of provider and centre types in 107 RHP responses.
Discussion
The existing literature on PTD mostly from Western sources and focussed on store-and-forward (asynchronous) systems. In contrast, this study offers key insights into PTD in a developing country, using a well-established telemedicine platform to address a wide spectrum of dermatological disorders in a large paediatric cohort from underserved communities.
Quality of image was significantly more helpful than other consultation variables for diagnosing and tailoring management. While studies have shown mixed results regarding image quality’s impact on diagnosis alone, most emphasise its importance.5,15-18 The next key factor was audio-video communication, suggesting that real-time (synchronous) teledermatology systems may be more effective than asynchronous ones, though further validation is needed. Ancillary patient history, while valuable in traditional clinical settings, was relatively less useful in PTD where audiovisual assessment predominates. Hence, PTD systems should prioritise good audio-video connectivity and training providers to capture high-quality, representative images over extensive historical data collection.15
While certain variables were less helpful, their value should not be undermined. Multiple images, though mostly ‘somewhat helpful,’ proved valuable for dermatoses requiring assessment of extent/distribution/severity to guide management, and those with varied clinical morphologies, including rashes (atopic dermatitis, seborrheic dermatitis, chickenpox), acne, and vitiligo. This aligns with Philips et al.’s findings on the importance of multiple images for childhood rashes.16 Ancillary history, though of limited overall utility, was ‘very helpful’ in 11% of cases, especially contagious dermatoses like scabies and impetigo, where understanding family contacts and living conditions aided management. Infections and infestations were the most common diagnoses in this cohort, while naevi and tumours were least common, contrasting with Western PTD studies that report more naevi.10,19
Emergency/acute dermatoses, comprising 1.35% of PTD cases, were advised for immediate in-person interaction as per national telemedicine guidelines. Teleconsultations facilitated necessary immediate interventions such as appropriately-dosed empirical antibiotics/antivirals/steroids, monitoring, counselling on local care, and urgent referral to higher centres. Overall, only a small percentage (4.47%) of cases required referrals for in-person evaluation, including these emergency/acute cases [Table 1]. This suggests that a majority (95.53%) of first-time, low-complexity, non-procedural cases could be managed remotely, demonstrating PTD’s utility in situations where immediate in-person specialist care is unavailable. The process also serves as an effective triage system, determining the necessity and urgency of referrals and preventing complications.3,10,12 RHPs strongly endorsed the service, rating it nearly as effective as in-person care for PTD, with added educational benefits, aligning with previous reports demonstrating bidirectional learning.15,17,20 Another assisted telemedicine model, ‘e-consults’ in the US, which uses the store-and-forward format, showed comparable provider satisfaction.15,17 Parental/guardian satisfaction ratings likely reflect growing acceptance due to convenience, live specialist interactions, reduced wait times, cost savings, accessibility, and avoiding the logistical challenges of traveling with young children or missing work/school.1,3,10,15,21 Previous studies report higher parental satisfaction with synchronous (real-time) PTD compared to store-and-forward systems, though comparative trials are lacking.1,15,21 While diagnostic and management concordance could not be assessed, prior studies report concordance rates of 70.1%-89%.1,15,16,22-25
Limitations
The study had several limitations. Diagnostic and management concordance could not be assessed, as referred cases were not always evaluated at the authors’ centre, precluding direct comparisons between telemedicine and in-person diagnoses. The diagnostic discordance in this study remains unclear, warranting further investigation. The telemedicine model resulted in an average travel distance saved of 459 km per patient, likely influencing decisions regarding in-person consultations. The 9.6% follow-up rate, reflecting only platform re-consultations, was lower than that in studies with shorter travel distances or in-person follow-ups. Other limitations included short duration, potentially missing seasonal variations in paediatric dermatoses, and restriction of the study population to those able to access peripheral ‘spoke’ centres, despite minimised selection bias through consecutive sampling. Additionally, patient-reported outcomes and operational factors like connectivity, video quality, and cost-effectiveness were not assessed. Future multi-centre studies should address these gaps, particularly in evaluating diagnostic accuracy through direct comparisons with in-person evaluations.
Conclusion
This study demonstrates the feasibility and effectiveness of PTD in marginalised areas in a developing country, highlighting its utility to manage routine cases, empirically treat emergency dermatoses, and serve as a triage tool. The integration of e-Sanjeevani into India’s healthcare infrastructure offers a functional foundation for further upscaling PTD services. Enhancements should focus on optimising image quality, enabling audiovisual communication, refining historical data usage, and continuing training for RHPs. It is hoped that the insights gained will help bridge gaps in paediatric dermatological care, particularly in remote resource-constrained settings.
Acknowledgements
The authors express their gratitude to Mr. Ankit Gill and Mr. Ritesh Garg, telemedicine operators at the Department of Telemedicine, PGIMER, Chandigarh, for their assistance in preparing the Excel sheets. The authors appreciate the dedicated healthcare providers, support staff, and patients involved in this initiative, as well as the National Health Mission (NHM) Haryana for their support.
Ethical approval
The research/study was approved by the Institutional Ethical Committee at Post Graduate Institute of Medical Education & Research, Chandigarh, number PGI/IEC/2023/EIC000523, dated 10.02.2023.
Declaration of patient consent
Patient consent is not required as the identity of patients is not disclosed or compromised in any form.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Efficacy, perception, and utilization of pediatric teledermatology: A systematic review. JAAD Int. 2023;12:3-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pediatric teledermatology: A tool for combating dermatology care disparities. Dermatol Online J. 2021;27
- [CrossRef] [Google Scholar]
- Effectiveness of pediatric teledermatology. J Drugs Dermatol. 2020;19:1250.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric teledermatology--a survey of current use. Pediatr Dermatol. 2008;25:158-62.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology: Kids are not just little people. Clin Dermatol. 2017;35:594-600.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical training and research opportunities for dermatology residents in India. Indian Dermatol Online J. 2018;9:231-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pediatric teledermatology: A review of the literature. Pediatr Dermatol. 2021;38:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- Emergence of dermatology in India. Indian J Dermatol Venereol Leprol. 2009;75:86-92.
- [CrossRef] [PubMed] [Google Scholar]
- Access to pediatric dermatology. Curr Opin Pediatr. 2022;34:359-66.
- [CrossRef] [PubMed] [Google Scholar]
- The majority of skin lesions in pediatric primary care attention could be managed by teledermatology. PLoS One. 2019;14:e0225479.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evolution of India’s national teleconsultation platform e-Sanjeevani: A comparative analysis of versions 2.0 and 1.0, with a preliminary report from the state of haryana. Health Technol. 2025;15:153-60.
- [Google Scholar]
- Telemedicine_Practice_Guidelines.pdf. Guidelines for Telemedicine Services. Available from: https://esanjeevani.mohfw.gov.in/assets/guidelines/Telemedicine_Practice_Guidelines.pdf Last accessed date January 29, 2025.
- Navigating dermatological care: Experience with assisted teledermatology practice on e-sanjeevani platform. J Eur Acad Dermatol Venereol. 2024;38:2311-3.
- [CrossRef] [PubMed] [Google Scholar]
- eSanjeevani. Available from: https://esanjeevani.mohfw.gov.in/#/about Last accessed date January 29, 2025.
- Evaluation of electronic consults for outpatient pediatric patients with dermatologic complaints. Pediatr Dermatol. 2021;38:1210-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric teledermatology consultations: Relationship between provided data and diagnosis. Pediatr Dermatol. 2013;30:561-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric dermatology eConsultation: Insights to reduce barriers to utilization and increase access to care. Pediatr Dermatol. 2024;41:1114-6.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology: Diagnostic reliability in 383 children. Eur J Dermatol. 2015;25:563-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tele-derm national: A decade of teledermatology in rural and remote Australia. Aust J Rural Health. 2016;24:193-9.
- [CrossRef] [PubMed] [Google Scholar]
- Managing outbreak of community-onset paediatric impetigo in underserved areas of North India via teledermatology: A tertiary care centre’s experience. Indian J Dermatol Venereol Leprol 2024:1-3.
- [Google Scholar]
- Implementation of a pediatric provider-to-provider store-and-forward teledermatology system: Effectiveness, feasibility, and acceptability in a pilot study. Pediatr Dermatol. 2020;37:1106-12.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of pediatric teledermatology using parent-submitted photographs: A randomized clinical trial. JAMA Dermatol. 2017;153:1243-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Store-and-forward teledermatology versus in-person visits: A comparison in pediatric teledermatology clinic. J Am Acad Dermatol. 2009;60:956-61.
- [CrossRef] [PubMed] [Google Scholar]
- Store-and-forward teledermatology results in similar clinical outcomes to conventional clinic-based care. J Telemed Telecare. 2007;13:26-30.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of the effectiveness of teledermatology in the diagnosis of skin lesions in pediatric patients. Rev Assoc Med Bras (1992). 2023;69:e20230253.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







