Translate this page into:
Paraneoplastic hypercalcaemia in giant condyloma acuminatum associated squamous cell carcinoma
Corresponding author: Dr. Fatmagul Dirican Ulusoy, Department of Dermatology, Liv Hospital Ulus, Istanbul, Turkey. fgdirican@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dirican Ulusoy F, Acar A, Yaman B, Ceylan C. Paraneoplastic hypercalcaemia in giant condyloma acuminatum associated squamous cell carcinoma. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_826_2024
Dear Editor,
Giant condyloma acuminatum (GCA), also known as the Buschke-Lowenstein tumour, is a rare tumour caused by the human papillomavirus (HPV) that affects the anogenital region and slowly progresses to being invasive. The reason behind the transformation of GCA to squamous cell carcinoma (SCC) is unclear, but the oncogenic properties of HPV and the chronic inflammatory environment within the condyloma are believed to be associated with the same. While paraneoplastic hypercalcaemia is well-defined in many malignant diseases, it has rarely been reported in patients with localised skin tumours.1-3 Paraneoplastic hypercalcaemia is exceptionally rare in GCA cases and can easily be overlooked.
A 63-year-old man presented with anogenital lesions that persisted for the last 20 years. Physical examination revealed irregular, papillomatous plaque lesions extending from the base of the penis to the suprapubic region and a verrucous tumoral mass lesion in the right scrotal area [Figure 1]. Histopathological examination of two skin biopsies revealed findings consistent with verruca vulgaris and in situ SCC [Figures 2a and 2b]. Laboratory investigations showed normal liver and kidney function tests, serum immunoglobulin levels, and negative serologies for hepatitis B, hepatitis C, HIV, and syphilis. Serum calcium level was 13.2 mg/dL (normal range: 8.6-10.2 mg/dL). The values for serum calcium were persistently higher for 5 consecutive days preoperatively, prompting the initiation of intravenous hydration therapy.

- Irregular papillomatous plaque extending from the penile root to the suprapubic region and verrucous tumoral mass lesion extending to the right inguinal region.
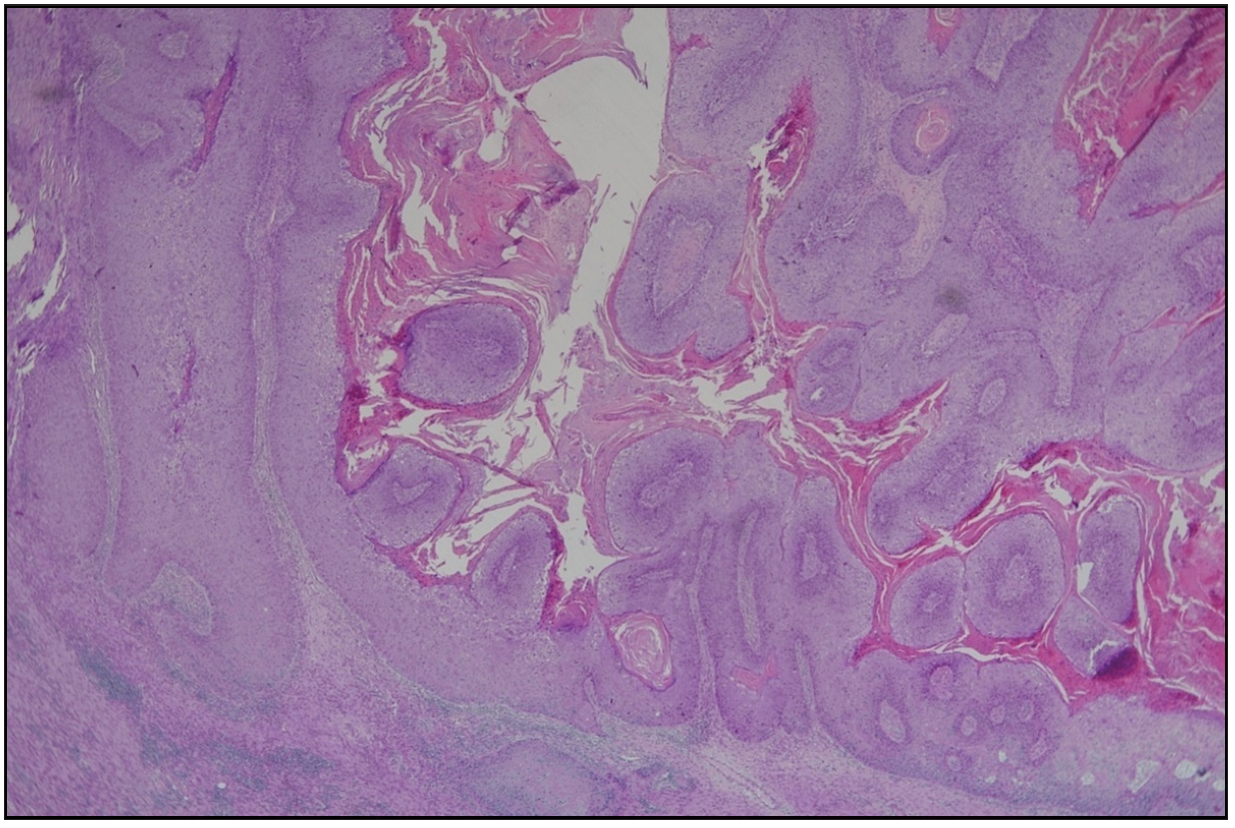
- Papillomatous condylomatous hyperplasia of the epidermis with full-thickness dysplasia. (Haematoxylin & eosin, 20x).
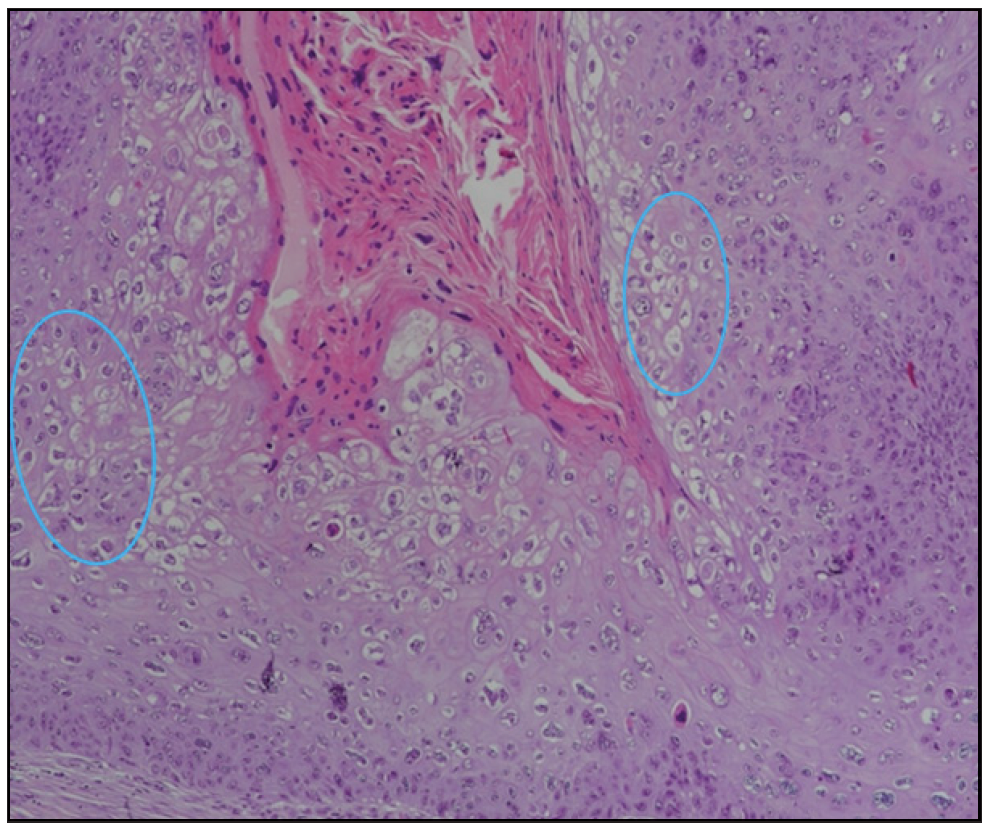
- Full-thickness dysplasia in the epidermis and koilocytotic changes (blue circles) (Haematoxylin & eosin, 200x).
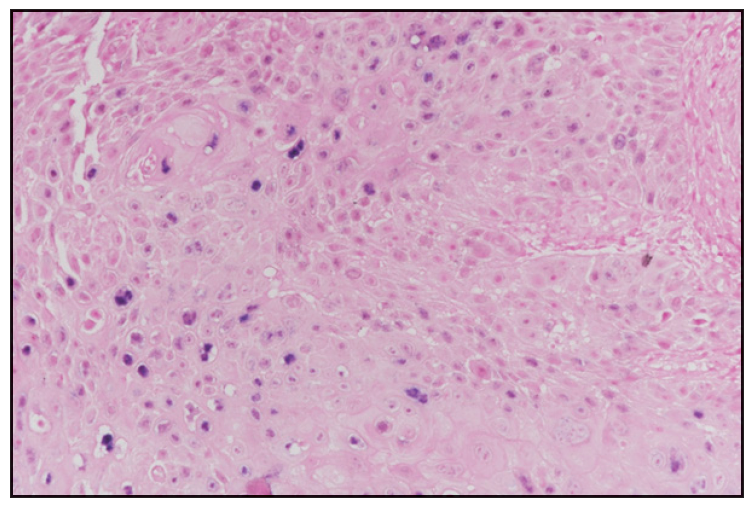
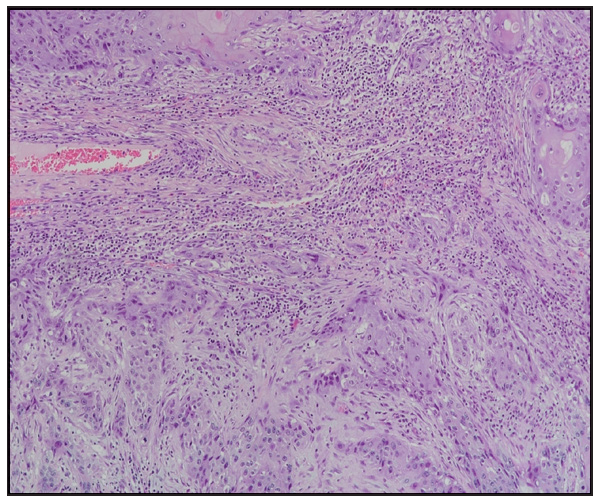
Comprehensive investigation for hypercalcaemia aetiology revealed low parathyroid hormone (PTH) levels, with normal 25-hydroxy vitamin D and phosphorus levels. Protein electrophoresis showed polyclonal γ-globulin elevation. Metastatic workup, including thoracic and abdominal computed tomography scans, were unremarkable. The lesions were completely excised. Histopathological examination of the excision material revealed invasive SCC on the base of the condyloma. In the biopsy where the patient was diagnosed with SCC in situ, HPV6/11 positivity was detected in the examinations performed in terms of low and high-risk HPV subtypes in chromogenic in situ hybridization. [Figures 2c, 2d and 2e]. After the operation [Figure 3], serum calcium levels returned to normal (9.4 mg/dL) within 24 hours. Preoperative and postoperative albumin levels were measured and were found to be within the normal range.
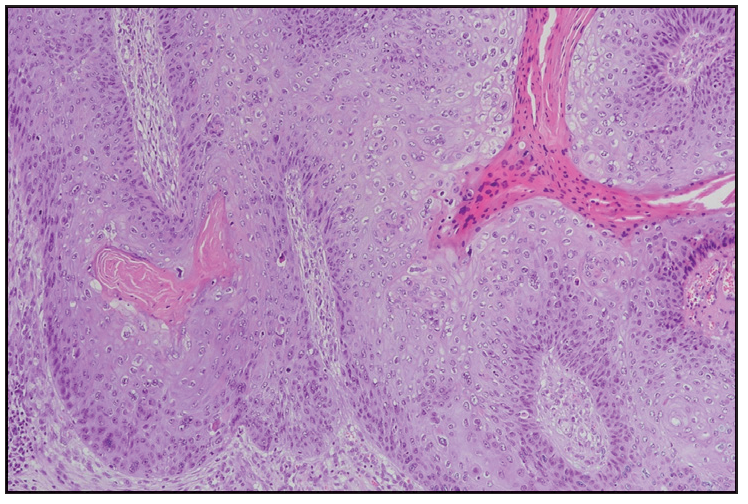
- Invasive squamous cell carcinoma nests in the dermis below condyloma acuminatum. Haematoxylin and eosin, 100x).
- Invasive areas of SCC seen in the dermis below condyloma acuminatum (Haematoxylin and eosin, 100x).
- HPV6/11 positivity at chromogenic in situ hybridisation (Haematoxylin and eosin, 200x).

- Extensive skin defect in the scrotal, inguinal, and pubic regions after excision.
Surgical excision is the primary treatment for hypercalcaemia associated with GCA. Hernandez et al. reported that in a case involving GCA and elevated parathyroid hormone-related protein, serum calcium levels normalised after surgery, and the parathyroid hormone-related protein became undetectable.1 Similarly, in our case, serum calcium levels significantly decreased to normal levels following surgical excision. For patients ineligible for surgical intervention, Linnemann et al. demonstrated the effectiveness of diuretics infusions and the adjunctive use of bisphosphonates.2
We presume that the moderate hypercalcemia in our patient was caused by PTHrP secreted by tumor cells. The PTHrP resembles parathyroid hormone, binds to parathyroid hormone receptors, adversely activating various organs with most of the damage to the bones with its osteolytic action resulting in hypercalcemia. Consistent with these findings, we detected lytic areas in the left proximal humerus and lateral scapula in the bone survey of our patient.
In summary, GCA can progress to invasive SCC, with paraneoplastic hypercalcaemia being a rare but significant complication. Due to the rarity of this complication, it would not be cost-effective to monitor calcium levels in all patients with GCA, as it would increase workload. However, in patients presenting with signs of hypercalcaemia, dermatologists should consider this rare complication and provide appropriate and timely medical intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Paraneoplastic hypercalcemia caused by an invasive squamous cell carcinoma arising from a giant anal condyloma acuminatum. Int J Colorectal Dis. 2009;24:359-60.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of paraneoplastic hypercalcemia in a patient with giant condyloma acuminatum: A case report. J Med Case Reports. 2013;7
- [Google Scholar]
- Giant condylomata acuminata of buschke-lowenstein associated with paraneoplastic hypercalcemia. J Investig Med High Impact Case Rep. 2018;6:2324709618758348.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






