Translate this page into:
A rare case of systemic amyloidosis presenting as palmar purpuric eczematous eruption
Corresponding author: Dr. Kanika Sahni, Department of Dermatology & Venereology, All India Institute of Medical Sciences, Delhi, India. kanu.sah@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary A, Gowda S K, Sharma R, Arava S, Sahni K. A rare case of systemic amyloidosis presenting as palmar purpuric eczematous eruption. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_137_2025
Dear Editor,
A 55-year-old man presented to the dermatology outpatient department with minimally itchy, red-coloured, bumpy lesions on his palms for 8 months. Examination revealed two morphologies. There were yellow to skin-coloured shiny translucent to waxy papules on the thenar eminence, palmar aspect of the distal and proximal interphalangeal and metacarpophalangeal joints. A few were ill-defined, purpuric, minimally scaly plaques on creases and thenar eminence of the right palm [Figures 1a and 1b]. He was previously diagnosed with palmar eczema and treated with topical steroids but showed only minimal improvement. An unusual morphology led us to examine the oral mucosa, which showed macroglossia with prominent tooth indentations, waxy infiltrated papules on the dorsum of the tongue, and multiple areas of purpura [Figure 1c]. There were multiple non tender boggy swellings on the occipital area of the scalp [Figure 1d]. The patient denied any weight loss, paraesthesia, light-headedness, syncope, hoarseness of voice or bony pains. The prominent macroglossia led us to consider primary systemic amyloidosis. We biopsied both tongue and palmar lesions, which showed amorphous eosinophilic deposits in the lamina propria, papillary and perivascular locations [Figure 2a]. Congo red stain showed khaki red to brown material on light microscopy, which demonstrated apple-green birefringence under polarised microscopy. Immunohistochemistry showed significant positivity positive for serum amyloid associated proteins [Figures 2b and 2c]. Serum for immunoglobulins IgM and IgG were elevated (1.2 and 17.9 g/dL respectively). Serum electrophoresis showed elevated free ĸ and λ chains (28.9g/L and 2164 g/L, respectively) with a reversal of the ĸ to λ ratio. Skeletal survey, M band electrophoresis, peripheral smear, serum calcium, and urine electrophoresis were normal. Bone marrow aspiration showed 17% plasma cells with λ restriction on flow cytometry. The skeletal survey was normal. Primary systemic amyloidosis with multiple myeloma was diagnosed, and the patient was planned for chemotherapy with bortezomib, dexamethasone and lenalidomide.

- Keratotic plaques and areas of purpura on bilateral palms.
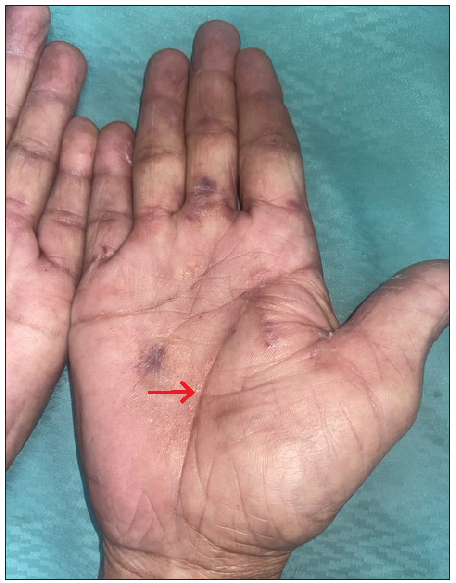
- Waxy papules and purpura along the creases of the right palm (indicated by the red arrow).

- Macroglossia with pebbly surface.
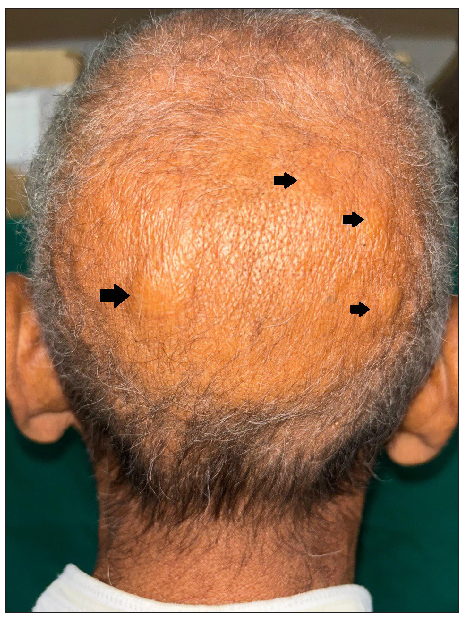
- Multiple soft boggy swelling over occiput (black arrows).
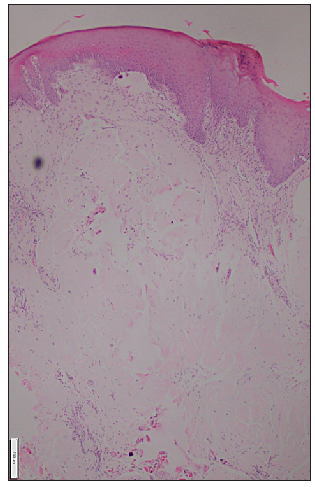
- Eosinophilic homogenous deposit in the dermal papilla (Haematoxylin & eosin, 50x).
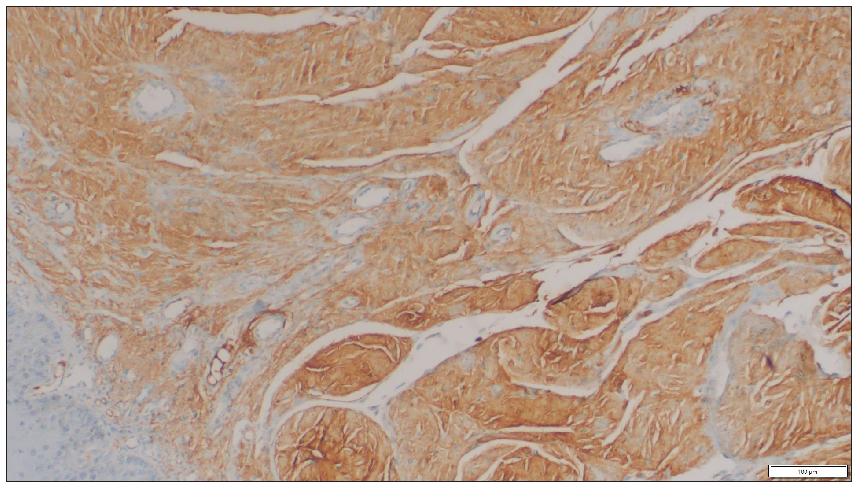
- Amyloid associated protein deposits on the dermal region of the tongue (Immunohistochemistry, 50x).
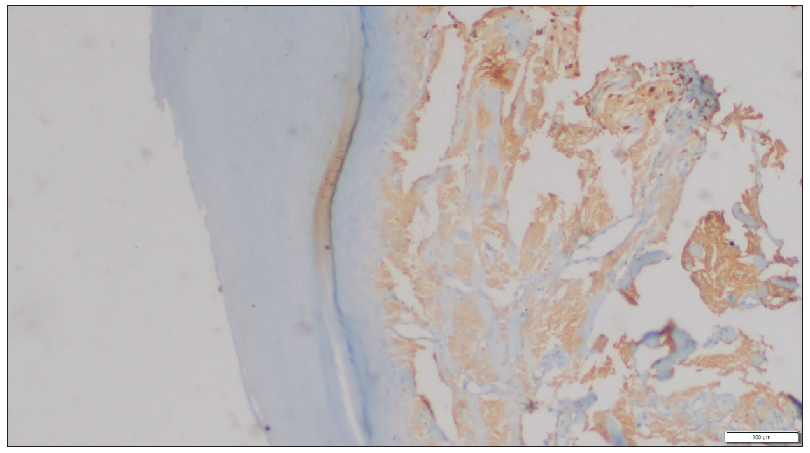
- Amyloid-associated protein deposits on the palm (Immunohistochemistry, 50x).
Primary systemic amyloidosis is a rare disease resulting from skin and organ deposition of monoclonal light chains either due to multiple myeloma or Waldenstrom macroglobulinemia.1 The complex interaction of these light chains with elastic tissue in the skin leads to dysfunction of the latter, which results in ecchymosis, easy bruising, cutis laxa, scleroderma, purpura, and waxy thickening (as in our case). Another significant pointer to the diagnosis is often macroglossia with scalloped margins over the lateral aspect of the tongue, as in our patient. Other cutaneous presentations of multiple myeloma include follicular hyperkeratotic spicules, diffuse alopecia, cutis verticis gyrata, nail dystrophy, and digital nodular swelling.2,3 When faced with a case demonstrating purpuric and ecchymotic lesions on the palms, the differential diagnoses include papular purpuric gloves and socks syndrome, palmoplantar erythrodysesthesia secondary to chemotherapy, dermatitis herpetiformis, and trauma.4,5 There are a few case reports of palmar purpura and nail fold waxy papules as manifestations of amyloidosis.6,7 However, in these reports, easy bruising and purpura were seen at other sites as well.
We hereby want to highlight the atypical presentation of primary systemic amyloidosis as palmar purpura and encourage an oral mucosal examination, which can often clinch the diagnosis of systemic amyloidosis.
Declaration of patient consent
The authors certify that they have obtained appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- A case of multiple myeloma-associated systemic amyloidosis with multiple skin manifestations as the first symptom. Clin Cosmet Investig Dermatol. 2023;16:987-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary systemic amyloidosis mimicking rhinophyma. Indian Dermatol Online J. 2019;10:204-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous manifestations of multiple myeloma and other plasma cell proliferative disorders. Semin Oncol. 2016;43:395-400.
- [CrossRef] [PubMed] [Google Scholar]
- Painful palmar and plantar purpura. JAMA Dermatol. 2021;157:993-4.
- [CrossRef] [PubMed] [Google Scholar]
- Purpuric paradigm: Multiple purpuric lesions on palms. Indian J Dermatol Venereol Leprol 2024:1-3.
- [CrossRef] [Google Scholar]
- Cutaneous amyloidosis as the first presentation of Waldenström macroglobulinemia. Caspian J Intern Med. 2020;11:340-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary systemic amyloidosis initially presenting with digestive symptoms: A case report and review of the literature. Diagn Pathol. 2015;10:174.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





