Translate this page into:
Acitretin-induced differentiation syndrome in a case of generalized pustular psoriasis
Correspondence Address:
P. S. S. Ranugha
Department of Dermatology, JSS Medical College and Hospital, JSS Academy of Higher Education and Research, MG Road, Mysore - 570 004, Karnataka
India
| How to cite this article: Gowda P, Shastry V, Ranugha P, Rangappa V. Acitretin-induced differentiation syndrome in a case of generalized pustular psoriasis. Indian J Dermatol Venereol Leprol 2020;86:231 |
Differentiation syndrome, also known as retinoic acid syndrome, is a rare complication of systemic retinoids, usually seen during treatment of acute promyelocytic leukemia with all trans retinoic acid.[1] Acitretin, a second-generation retinoid, is the treatment of choice in generalized pustular psoriasis. We report differentiation syndrome in a case of generalized pustular psoriasis, after acitretin treatment.
A 42 year old female, with a 2 year history of generalized pustular psoriasis was in remission with 100 mg cyclosporine (CysA) twice daily and 10 mg prednisolone once daily. She was receiving short, intermittent courses of cyclosporine for 2 years with two episodes of exacerbation in the past 2 years. For the present episode, she was admitted for acute exacerbation of pustular lesions on the neck, abdomen and thighs after stopping CysA for 2 weeks. The histopathology of pustular lesions from the abdomen revealed parakeratosis, acanthosis and spongiform pustules of Kogoj [Figure - 1]. No systemic manifestations were seen at the time of admission. Acitretin 25 mg was given orally, and after 6–7 h of the first dose, she developed fever, facial puffiness, periorbital edema and erythema, breathlessness and cough without expectoration. There was no chest pain, nausea, vomiting, abdominal pain or passage of high-colored urine. Itching or wheals were not present and no fresh crops of pustules appeared. On examination, the patient was febrile with tachycardia, dyspnea, hypotension, periorbital edema [Figure - 2]a and bilateral pitting edema of the hands and feet. Generalized erythema and scaling were present with relative sparing of the palms and soles. Resolving pustular lesions were seen on the face, trunk and extremities. No mucosal involvement was seen and lymphadenopathy was absent. Bilateral basal crepitations were heard on auscultation of the lung fields. Oxygen saturation was 94%. Arterial blood gas analysis showed respiratory alkalosis with metabolic acidosis, however, renal function test and serum electrolytes were normal. Complete hemogram showed leukocytosis (leukocyte count 19,670 cells/mm3), chest X-ray, electro and echocardiogram were normal. Skin biopsy was not done as the patient did not provide consent for it.
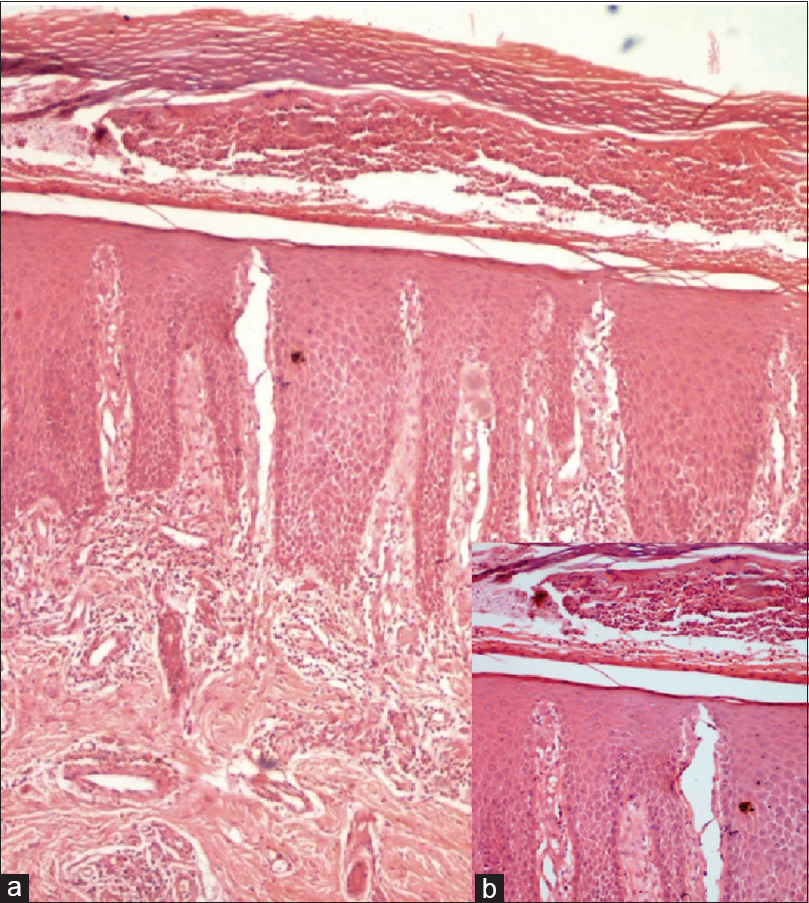 |
| Figure 1: (a) Epidermis displaying focal parakeratosis, acanthosis and neutrophil collections in stratum corneum and malpighii (hematoxylin and eosin, ×100). (b) Inset showing spongiform pustules of Kogoj in Malpighian layer (hematoxylin and eosin, ×400) |
 |
| Figure 2: |
Acute generalized exanthematous pustulosis and angioedema were ruled out because of the absence of fresh pustules and lip or laryngeal edema, respectively. As the patient did not have fatigue, myalgia, flushing or gastrointestinal symptoms suggestive of a capillary leak syndrome, the diagnosis of differentiation syndrome was considered over capillary leak syndrome, although the latter could not be ruled out completely. Causality assessment using Naranjo scale attributed the reaction to acitretin. Acitretin was stopped immediately and patient was started on intravenous betamethasone and supportive therapy. Periorbital edema subsided over 2 days and symptomatic improvement was seen [Figure - 2]b. Steroids were tapered and stopped over 2 weeks and the patient was put on oral cyclosporine 150 mg twice daily for generalized pustular psoriasis. There has been no recurrence of similar complaints till date.
Differentiation syndrome is seen in 2–27% of acute promyelocytic leukemia patients on all trans retinoic acid, with 5% mortality. The onset of differentiation syndrome after initiation of all trans retinoic acid has been shown to range from 0 to 46 days (median 12 days). The differentiation of leukemic blasts during induction therapy by all trans retinoic acid/arsenic trioxide causes cellular migration and endothelial activation leading to differentiation syndrome.[1] The clinical presentation is highly variable. While fever, dyspnea and peripheral edema are reported in >50% of cases, hypotension and pulmonary infiltrates are less common.[1] Diagnosis is based on the presence of at least two of the following signs and symptoms: dyspnea, unexplained fever, weight gain >5 kg, unexplained hypotension, acute renal failure and chest radiograph demonstrating pulmonary infiltrates or pleuro-pericardial effusion.[1] The disease may progress to acute respiratory distress syndrome, diffuse alveolar damage or massive intra-alveolar hemorrhage.[2] Administration of high-dose dexamethasone at the onset of first sign or symptom has been shown to reduce mortality associated with differentiation syndrome.[1]
Our patient had fever, hypotension and respiratory distress, which started immediately after acitretin and hence satisfied the criteria for differentiation syndrome. Our case could be considered as having a mild form of differentiation syndrome as she satisfied three criteria (<4), whereas the presence of four or more criteria is classified as severe differentiation syndrome.[1] Prompt response to withdrawal of acitretin and administration of systemic steroids in our case helped us rule out capillary leak syndrome retrospectively. Capillary leak syndrome is characterized by shock and massive edema, often after a nonspecific prodrome of weakness, fatigue and myalgia, with a risk for ischemia-induced organ failure, rhabdomyolysis, muscle compartment syndromes and venous thromboembolism. Acute episode of capillary leak syndrome is treated with vasopressor therapy and judicious fluid replacement; the role of steroids is controversial.[3] Differentiation syndrome has been considered synonymous with capillary leak syndrome by some.[4],[5] Whether both are identical or different entities needs further research. Systemic involvement in generalized pustular psoriasis is usually associated with fever, fresh crops of pustules, hepatitis and rarely, acute respiratory distress syndrome. The absence of new pustules and presence of facial puffiness and periorbital edema helped us rule out generalized pustular psoriasis with systemic involvement.
The pathogenesis of differentiation syndrome is not fully known, but it is believed that an excessive inflammatory response is provoked by leukemic cells in the process of differentiation. This results in increased production of chemokines and expression of adhesion molecules on acute promyelocytic leukemia cells leading to organ infiltration by blast cells, particularly the lungs, capillary-leak syndrome and organ failure.[2] The lymphocytes are, however, differentiated in psoriasis, and the exact pathogenesis of differentiation syndrome in psoriasis needs to be studied further.
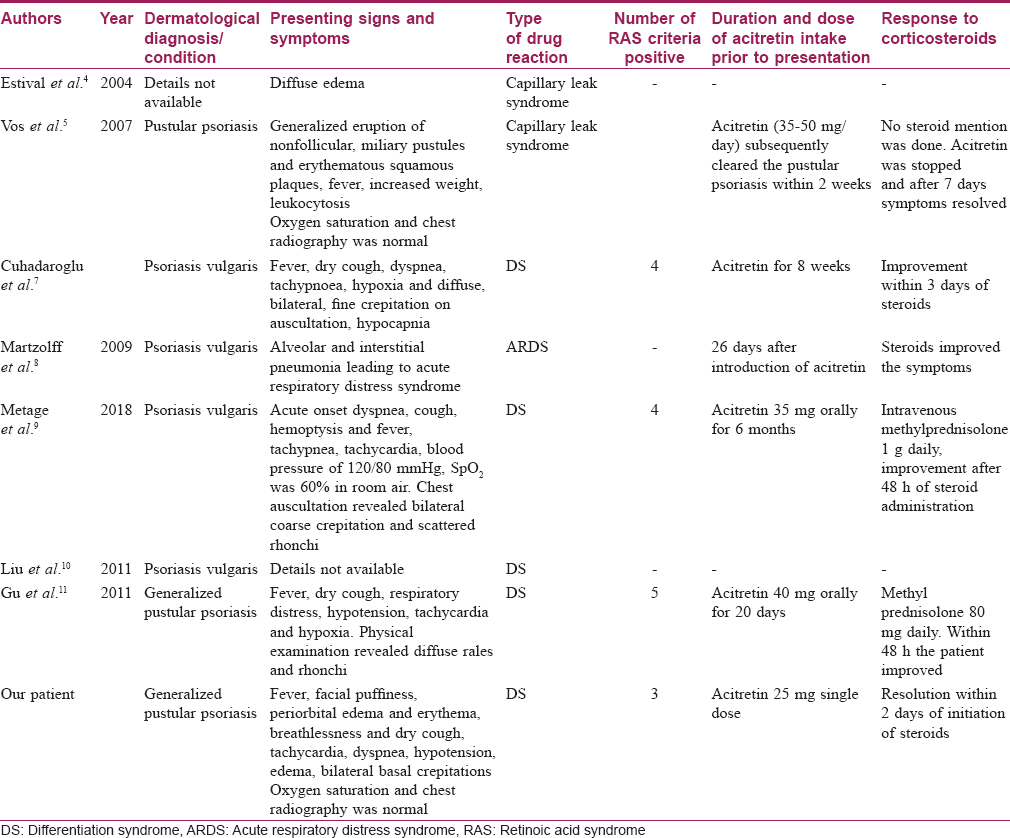
Although all trans retinoic acid is being used as an antitumor agent in Kaposi's sarcoma, head and neck squamous cell carcinoma, ovarian, bladder, neuroblastoma (glioblastoma multiforme), differentiation syndrome is not reported in any of these patients. Why differentiation syndrome occurs only in acute promyelocytic leukemia cases is still a gray zone. Acitretin belongs to the class of aromatic synthetic retinoids in which the cyclo-hexenyl group of retinoic acid has been replaced by a 4-methoxy-2, 3, 6-trimethylphenyl group. 6 Acitretin and all trans retinoic acid have a similar structure, except for slight modification in the aromatic ring. This might explain the occurrence of differentiation syndrome with acitretin. Two cases of capillary leak syndrome due to acitretin in generalized pustular psoriasis have been described earlier.[4],[5] Respiratory distress with acitretin has also been described in generalized pustular psoriasis.[7] Solitary cases of acitretin-induced pneumonia[8] and three cases of differentiation syndrome have been reported in patients with psoriasis vulgaris.[9],[10],[11] Various reports of differentiation syndrome in psoriasis described so far have been tabulated and compared in [Table - 1].
We, as dermatologists, need to be aware of this rare complication with acitretin as early identification and treatment of this condition can be lifesaving, as in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Montesinos P, Sanz MA. The differentiation syndrome in patients with acute promyelocytic leukemia: Experience of the PETHEMA group and review of the literature. Mediterr J Hematol Infect Dis 2011;3:e2011059.
[Google Scholar]
|
| 2. |
Cardinale L, Asteggiano F, Moretti F, Torre F, Ulisciani S, Fava C, et al. Pathophysiology, clinical features and radiological findings of differentiation syndrome/all-trans-retinoic acid syndrome. World J Radiol 2014;6:583-8.
[Google Scholar]
|
| 3. |
Druey KM, Greipp PR. Narrative review: The systemic capillary leak syndrome. Ann Intern Med 2010;153:90-8.
[Google Scholar]
|
| 4. |
Estival JL, Dupin M, Kanitakis J, Combemale P. Capillary leak syndrome induced by acitretin. Br J Dermatol 2004;150:150-2.
[Google Scholar]
|
| 5. |
Vos LE, Vermeer MH, Pavel S. Acitretin induces capillary leak syndrome in a patient with pustular psoriasis. J Am Acad Dermatol 2007;56:339-42.
[Google Scholar]
|
| 6. |
Handbook4_Retinoids-6.pdf. Available from: https://www.iarc.fr/en/publications/pdfs-online/prev/handbook4/Handbook4_Retinoids-6.pdf. [Last accessed on 2018 Dec 17].
[Google Scholar]
|
| 7. |
Cuhadaroglu C, Korular D, Erelel M, Kiyan E, Kiliçaslan Z. Respiratory distress with acitretin, reversal by corticosteroid. Dermatol Online J 2001;7:5.
[Google Scholar]
|
| 8. |
Martzolff L, Huber M, Dukic R, Thannberger P, Kieffer C, Kieffer P, et al. Acitretin-induced pneumonia: An underestimated complication of treatment of psoriasis. Rev Med Interne 2008;29:393-6.
[Google Scholar]
|
| 9. |
Metage C, Hazarika B, Sarma J, Karwa R. Retinoic acid syndrome in a elderly male with psoriasis – A case report. Respir Med Case Rep 2018;24:81-3.
[Google Scholar]
|
| 10. |
Liu D, Cao F, Yan X, Chen X, Chen Y, Tu Y, et al. Retinoic acid syndrome in a patient with psoriasis. Eur J Dermatol 2009;19:632-4.
[Google Scholar]
|
| 11. |
Gu W, Zhao G, Shi F. Acitretin-induced retinoic acid syndrome. J Am Acad Dermatol 2011;65:e148-9.
[Google Scholar]
|
Fulltext Views
5,020
PDF downloads
4,773





