Translate this page into:
Acrokeratosis paraneoplastica (Bazex syndrome) with bullous lesions
2 Division of Oncology, University Hospital of Marqués de Valdecilla, University of Cantabria, Santander, Cantabria, Spain
3 Division of Pathology, University Hospital of Marqués de Valdecilla, University of Cantabria, Santander, Cantabria, Spain
Correspondence Address:
C Duran-Vian
University Hospital of Marqués de Valdecilla, Valdecilla st, 25, 39008 Santander, Cantabria
Spain
| How to cite this article: Duran-Vian C, Gómez C, Navarro I, Reguero L, Alonso L, González-Vela M C, González-López M A. Acrokeratosis paraneoplastica (Bazex syndrome) with bullous lesions. Indian J Dermatol Venereol Leprol 2020;86:335 |
Sir,
Acrokeratosis paraneoplastica (Bazex syndrome) is a rare paraneoplastic skin disease associated mostly with squamous cell carcinomas of the upper aerodigestive tract. This syndrome is defined by erythematous, violaceous, scaly plaques on the hands and feet and on other acral locations such as ears and nose. Bullous lesions are uncommon, and most of them are located in acral areas.
A 57-year-old male consulted for a 3-month-long appearance of an insidious and progressive asymptomatic blistering eruption that involved his trunk and retroauricular region associated with scaly plaques on the hands and feet.
His past medical and personal history were significant for arterial hypertension, tobacco use and alcohol abuse. He was diagnosed 3 months earlier with oropharyngeal squamous cell carcinoma after presenting with dysphagia and weight loss. For the last 1 month, the patient was receiving chemotherapy with cisplatin for his cancer.
Cutaneous examination revealed several 0.5–3 cm tense, straw-colored fluid-filled bullae and erosions around his left retroauricular region and back [Figure - 1] and [Figure - 2]. In addition, he had symmetrically distributed violaceous psoriasiform lesions on the hands, palmoplantar hyperkeratosis, edematous fingers and violaceous psoriasiform plaques in both ears [Figure - 3] and [Figure - 4]. There were no bullous lesions on his hands or feet.
 |
| Figure 1: Asymptomatic tense blister* and erosion seen on the left retroauricular region |
 |
| Figure 2: Tense bulla with non-erythematous base, containing clear fluid present on the back of the patient. Flexural aspects, abdomen, feet and hands were spared |
 |
| Figure 3: Violaceous psoriasiform lesions on the dorsum of the hands associated with swelling of the digits with a blue to violet discoloration |
 |
| Figure 4: Induration, desquamation and violaceous swelling of the left ear helix |
No treatment was prescribed and skin biopsies were performed from the hyperkeratotic ear lesions and bullae on the back in order to confirm the clinical suspicion of acrokeratosis paraneoplastica and discard a concomitant primary autoimmune bullous disorder, especially bullous pemphigoid.
The biopsy from the ear revealed hyperkeratosis and interface dermatitis with mixed perivascular inflammatory infiltrate [Figure - 5]. The biopsy from the bullous area showed a subepidermic bullae, dyskeratosis and a mixed inflammatory infiltrate consisting of eosinophils, lymphocytes and melanophages [Figure - 6]. Direct immunofluorescence was negative. The presence of interface dermatitis with hyperkeratosis and eosinophil-rich infiltrate was consistent with the clinical diagnosis of Bazex syndrome.
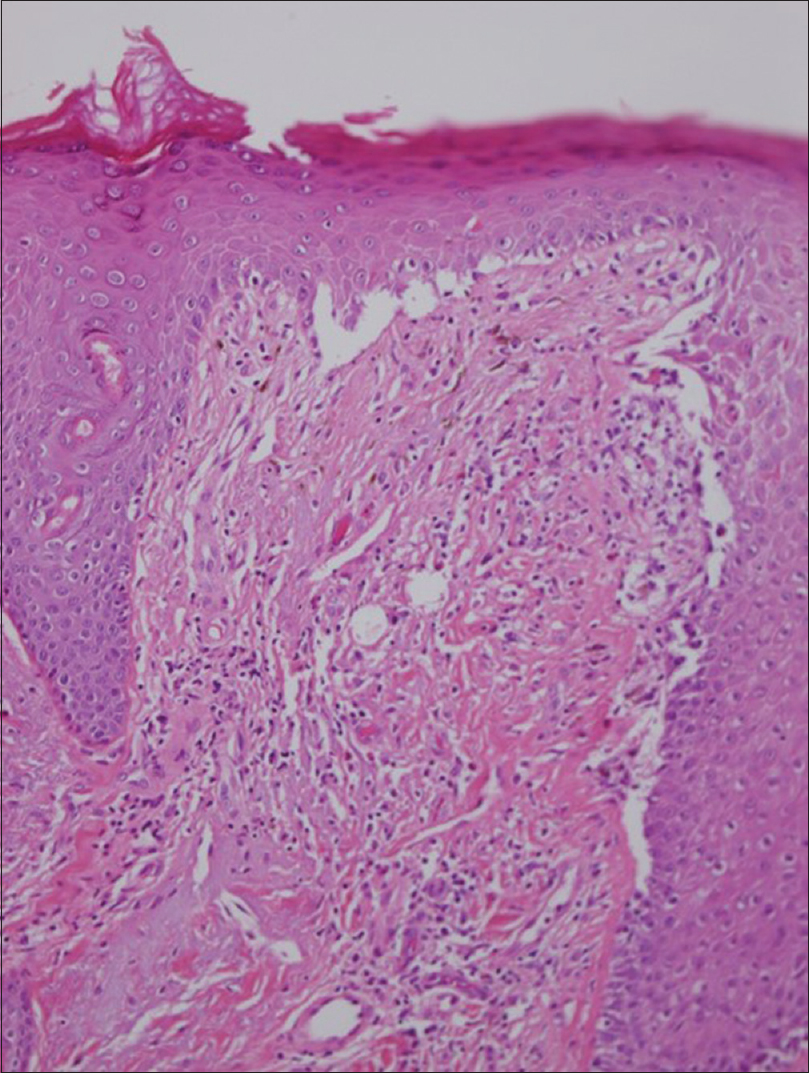 |
| Figure 5: Hyperkeratosis, acanthosis, subepidermal blister and deep perivascular and periadnexal lymphocytic infiltrate are shown in the biopsy from the helix (hematoxylin and eosin, ×100) |
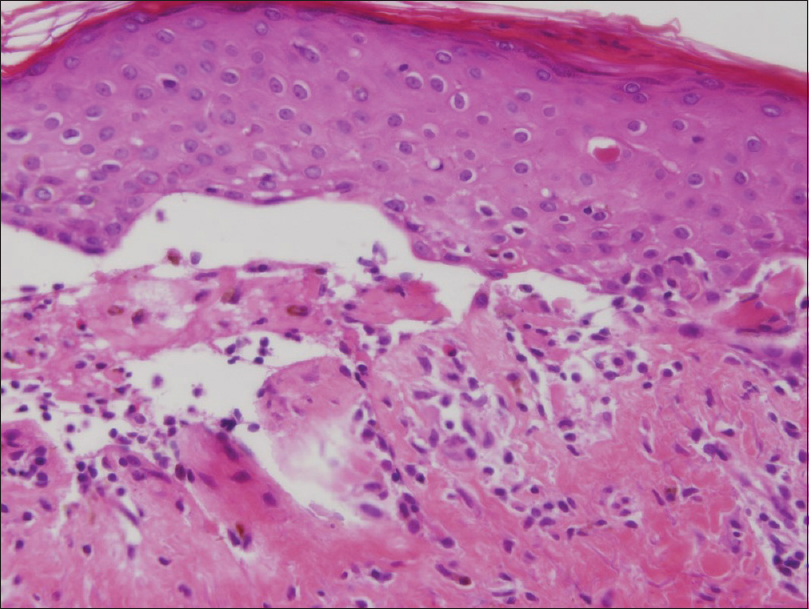 |
| Figure 6: Subepidermal blister, dyskeratosis and a mixed inflammatory infiltrate are demonstrated in the biopsy from the back bullous area (hematoxylin and eosin, ×200) |
Two months later, the patient showed an improvement of his clinical manifestations that we attributed to chemotherapy treatment. Nevertheless, a few months later the patient died of acute liver failure.
Bazex syndrome is a rare disease in which characteristic cutaneous changes are associated with underlying carcinoma. The presence of bullae and vesicles is not typical and has only been reported in a minority of patients with Bazex syndrome, especially located on the hands and feet.[1],[2],[3] Although the eruption can involve the limbs and trunk, we were unable to find any previous reports of bullous lesions located on the back.
The histological features of Bazex syndrome are often non-specific or show necrotic keratinocytes causing a vacuolization of the basal zone, thus leading to the creation of subepidermal clefts, clinically presenting as bullae, as we described.[4] Although the histological findings can include subepidermal or intraepidermal vesicles, no typical features of bullous autoimmune disorders have been reported. In addition, direct immunofluorescence is usually negative.
Our patient's clinical findings were suggestive of a blistering disease, but neither hematoxylin and eosin nor direct immunofluorescence evaluation showed evidence of bullous pemphigoid or paraneoplastic pemphigus.
Various explanations have been proposed for bullae formation such as coincidental distinct bullous disorder (porphyria, bullous pemphigoid) or developing another paraneoplastic bullous disorder such a paraneoplastic pemphigus.[1] Deposits of IgA, IgG and C3 in a nonspecific pattern along the epidermal basement membrane have been reported in some cases, supporting the theory that bulla formation is most probably part of the changes that may affect the skin of patients with Bazex syndrome.[1],[5]
These bullous lesions are rare in Bazex syndrome and they can mimic an autoimmune bullous disease. We emphasize the need to suspect Bazex syndrome in patients who present with atypical psoriasiform changes and bulla formation located not only on acral sites but also on the back. A correct diagnosis is based on histopathological features and negative immunofluorescence tests that exclude other bullous diseases with specific findings, especially in cases of acrokeratosis with unusual manifestations, as presented earlier.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Mutasim DF, Meiri G. Bazex syndrome mimicking a primary autoimmune bullous disorder. J Am Acad Dermatol 1999;40:822-5.
[Google Scholar]
|
| 2. |
Gill D, Fergin P, Kelly J. Bullous lesions in Bazex syndrome and successful treatment with oral psoralen phototherapy. Australas J Dermatol 2001;42:278-80.
[Google Scholar]
|
| 3. |
Schoeffler A, Sagot V, Marzin A, Brogniart P, Kanitakis J, Navailles B, et al. Acrokératose paranéoplasique bulleuse. Ann Dermatol Vénéréol 2006;133:557-60.
[Google Scholar]
|
| 4. |
Räßler F, Goetze S, Elsner P. Acrokeratosis paraneoplastica (Bazex syndrome) – A systematic review on risk factors, diagnosis, prognosis and management. J Eur Acad Dermatol Venereol 2017;31:1119-36.
[Google Scholar]
|
| 5. |
Pecora AL, Landsman L, Imgrund SP, Lambert WC. Acrokeratosis paraneoplastica (Bazex' syndrome). Report of a case and review of the literature. Arch Dermatol 1983;119:820-6.
[Google Scholar]
|
Fulltext Views
3,340
PDF downloads
3,065





