Translate this page into:
Acne fulminans in a young man with granulomatosis with polyangiitis (Wegener's granulomatosis): A chance association or marker of serious systemic disease?
2 P.D. Hinduja Research Center, Mahim, Mumbai, Maharashtra, India
3 One Center for Rheumatology and Genetics, Trivia Complex, Natubhai Circle, Vadodara, Gujarat, India
Correspondence Address:
Shyam Verma
18 Amee Society, Diwalipura, Vadodara - 390 015, Gujarat
India
| How to cite this article: Verma S, Joshi R, Shah R. Acne fulminans in a young man with granulomatosis with polyangiitis (Wegener's granulomatosis): A chance association or marker of serious systemic disease?. Indian J Dermatol Venereol Leprol 2020;86:669-673 |
Abstract
A 19-year-old man with granulomatosis with polyangiitis (Wegener's disease) presented with hemorrhagic facial nodules mimicking severe inflammatory acne (acne fulminans) as one of the first symptoms of the disease. The lesions were earlier treated as nodulocystic acne with isotretinoin without any benefit. Complete resolution was seen with pulsed methylprednisolone and oral prednisolone and mycophenolate mofetil thereafter. He also developed acute onset of severe pustular eruption of the face and a destructive ulcer of the auricle on two separate occasions. Facial lesions mimicking severe inflammatory acne, not responsive to standard treatment, may be a marker for more severe systemic disease such as Wegener's disease/granulomatosis with polyangiitis.
Introduction
Granulomatosis with polyangiitis affects mainly the upper and lower respiratory system and kidneys; however, many organs including skin may be involved. About 15% of the patients have cutaneous manifestations that are specific to granulomatosis with polyangiitis. Facial involvement with pyoderma-like lesions or ulcerations and especially involvement of the periauricular area are thought to be specifically suspicious for the disorder.
Case Report
A 19-year-old man was admitted with severe joint pains and fever with bleeding from “boils” on the face of a few days' duration. The lesions were painful, engorged with blood and had appeared in crops. In the past 2 years, he had developed painful bleeding nodular lesions on the face on and off, for which he was seen by a dermatologist and treated with a course of minocycline and topical clindamycin, without much effect. He had also received a course of 20 mg of isotretinoin per day for about 8 weeks, without much improvement. There was history of nasal polypectomy, a few months before presentation. He also had fleeting joint pains involving the ankles and knees and a history of purpuric eruption on the legs that cleared spontaneously. He complained of severe fatigue and had lost 7 kg body weight in the past 2 months. There was no cough or hemoptysis.
On examination, there were multiple crusted nodules on the face, many of which were breaking down, leaving bleeding ulcers with ragged edges [Figure - 1]a and [Figure - 1]b. A provisional diagnosis of acne fulminans versus hemorrhagic nodules related to a systemic disease, mimicking nodular acne was entertained. He had a total white blood cell count of 11,200 cells/mm[3], an erythrocyte sedimentation rate of 40 mm/1st hour and a C-reactive protein of 80 mg/L. His rheumatoid factor, antinuclear antibody studies, hepatic and renal profile were normal. His cytoplasmic antineutrophil cytoplasmic antibody was reported as 2+ on ethanol-fixed slide by immunofluorescence. PR3 (main antigen of cytoplasmic antineutrophil cytoplasmic antibody) was strongly positive at 9.73 by ELISA.
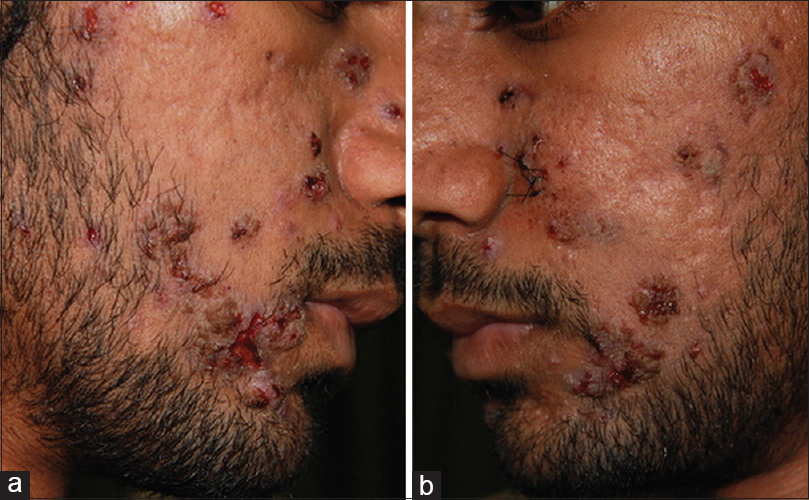 |
| Figure 1: (a and b): Hemorrhagic nodules mimicking nodular acne, some breaking down with crust formation and some juxtaposed with preexistent scars of acne |
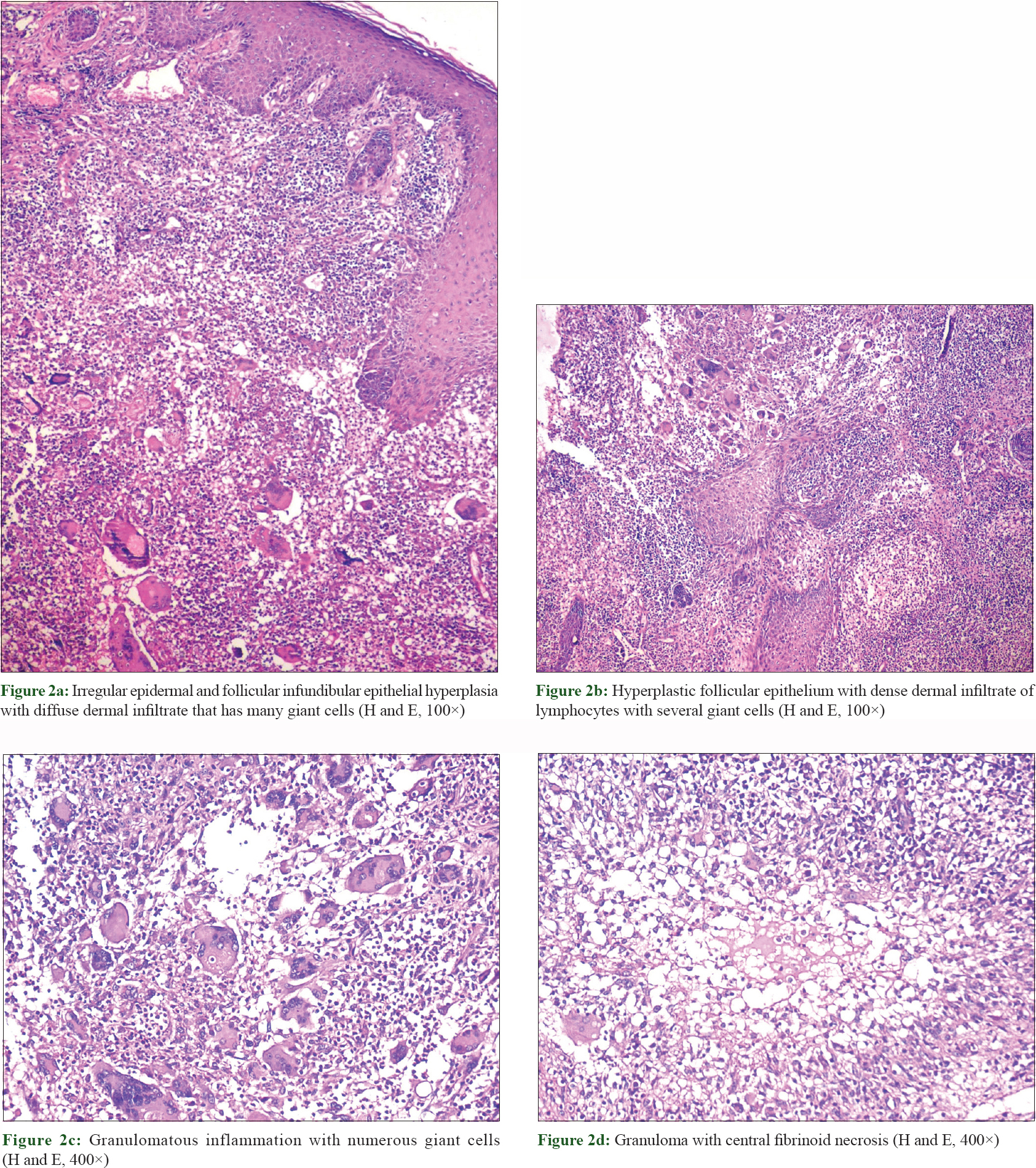
Commonly documented skin manifestations of granulomatosis with polyangiitis like papules, nodules on the limbs, palpable purpura, ulcers, oral ulcers, gingivitis etc., were absent. Two skin biopsies taken from the edge of an ulcerated nodule showed irregular epidermal and follicular infundibular epithelial hyperplasia with diffuse dermal infiltrate containing lymphocytes and numerous giant cells [Figure - 2]a. Follicular epithelium was hyperplastic with a dense dermal infiltrate of lymphocytes with several giant cells [Figure - 2]b. Against the backdrop of granulomatous inflammation with multiple giant cells were also some granulomas showing a central fibrinoid degeneration [Figure - 2]c and [Figure - 2]d. Computed tomography scan of paranasal sinuses and chest showed mucosal thickening of both ethmoid and maxillary sinuses and the nasal mucosa and discrete multiple angiocentric nodular opacities, respectively [Figure - 3]. His eyes, central nervous system and heart examinations were normal. His urine routine examination, urine 24-hour protein, serum creatinine and blood urea nitrogen were normal.
 |
 |
| Figure 3: Diffuse mucosal thickening involving both maxillary sinuses with blockage of osteomeatal complexes. Mucosal thickening is seen involving bilateral ethmoid sinuses too |
Clinicopathological correlation suggested a diagnosis of granulomatosis with polyangiitis presenting with hemorrhagic facial nodules mimicking nodular acne. He responded dramatically to methylprednisolone pulse of 500 mg administered intravenously for 5 days with topical mupirocin for 15 days for the lesions [Figure - 4]a and [Figure - 4]b. He was later treated with 60 mg of prednisolone and 2 g of mycofenolate mofetil. In the fifth month of treatment, he developed acute onset of painful pustular lesions studding his face and ulceration of the lobule of the ear [Figure - 5]a and [Figure - 5]b. Prednisolone was again increased to 80 mg and the lesions resolved in 3 weeks. He continued to be well with no complaints 12 months after starting therapy except for inflammatory acne-like facial nodules off and on that resolved spontaneously.
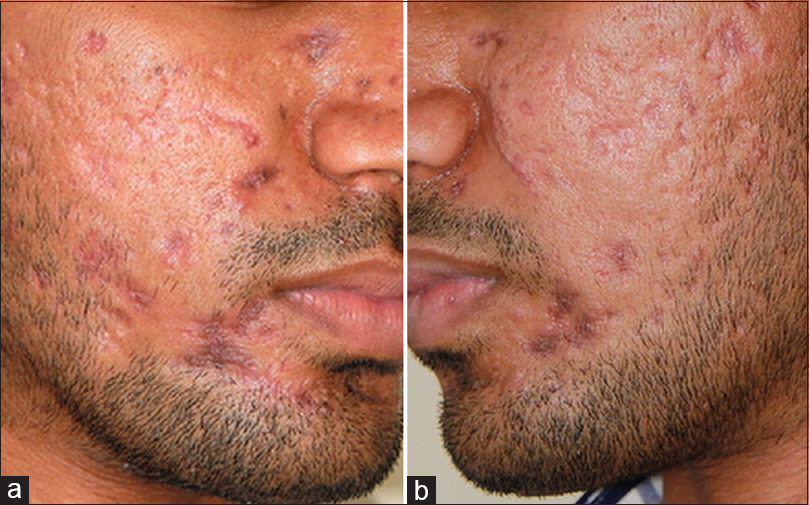 |
| Figure 4: (a and b): Healed lesions after pulsed methylprednisolone therapy |
 |
Discussion
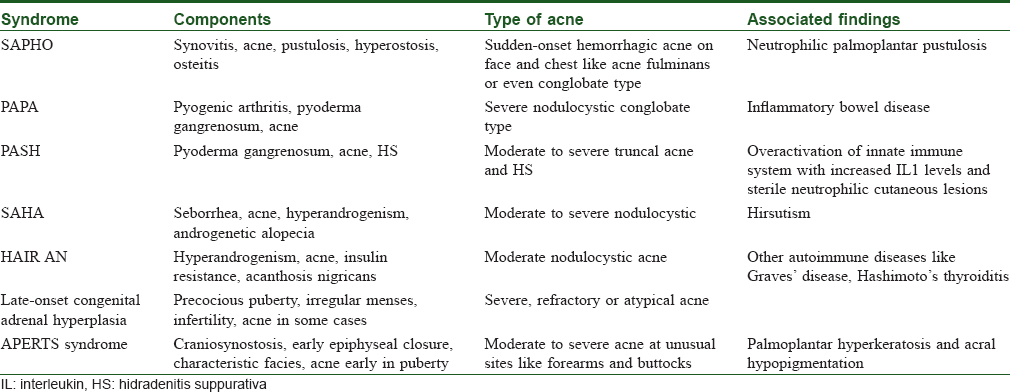
Granulomatosis with polyangiitis, previously known as Wegener's disease, is a rare multisystem disease. It is a form of small to medium vasculitis, and although it can affect any organ it most frequently targets the respiratory system and kidneys.[1] The peak incidence of the disorder which has been cited as between ages of 45 and 50 years has been shown to be increasing in child and adult population.[1],[2],[3] Data on the disorder in pediatric age group are sparse, but it is said to occur most commonly in the second decade.[1] Skin is involved in 35%–50% of patients with Wegener's granulomatosis[3],[4],[5] About 15% of patients have cutaneous lesions specifically associated with the disorder if one disregards those occurring secondary to infections, treatment or coexisting dermatoses unrelated to it.[1],[2],[3] Skin manifestations of the disorder include palpable purpura, cutaneous nodules, subcutaneous nodules, papules, vesicles, petechiae, urticarial lesions, panniculitis, pyoderma gangrenosum–like lesions and Raynaud's disease.[3],[4],[5] They are seldom seen to dominate the clinical picture.[4] Acneiform lesions have been reported in association with the disorder in patients younger than 20 years of age. They are often the first presenting symptom in this age group.[1],[6],[7],[8] Cutaneous lesions have been noted more frequently in multiorgan disease.[1],[2] Skin lesions are thought to run their course parallel to the systemic disease and generally respond to treatment of the disorder.[3],[4],[5] Our case gave history of developing painful acne-like eruptions on his back at 17 years of age which spontaneously resolved with scarring. He then developed facial nodules with systemic signs and symptoms that were treated by a dermatologist unsuccessfully. He had nasal symptoms which were diagnosed and treated as sinusitis and nasal polyposis and was eventually operated upon just a few months before the nodular eruption. There is only one previous report of hemorrhagic acneiform nodules occurring in a teenager in English literature but that patient seems to have had very mild lesions compared with ours.[6] Interestingly, that patient also developed an acute pustular eruption and a destructive ulcer of the auricular lobule. Facial involvement with pyoderma-like lesions or ulcerations and especially involvement of the periauricular area are thought to be specifically suspicious for Wegener's granulomatosis [Figure - 5]b.[2],[9] Over 50% of skin biopsies in granulomatosis with polyangiitis may yield nonspecific findings.[4],[10] Necrotizing vasculitis, granulomatous vasculitis, extravascular palisading granulomas and leukocytoclastic vasculitis are most commonly reported.[1],[4],[10] While evidence of some form of vasculitis helps in a definitive diagnosis of the disorder, it is not always the case and absence of it does not rule out granulomatosis with polyangiitis. Erythema nodosum–like septal granulomatous inflammation and acneiform granulomatous folliculitis have been reported.[1] Granulomatous pathology is also encountered not infrequently and represents tissue damage. It is said to be seen most often in non-purpuric lesions.[11] Our patient's skin biopsy from the facial nodules showed dense granulomatous infiltrate with plenty of lymphocytes and several giant cells but no evidence of vasculitis. A granuloma with central fibrinoid necrosis was also seen. This case underscores the importance of meticulously investigating patients presenting with severe acne-like lesions with associated musculoskeletal, upper airway, pulmonary or renal involvement with a high index of suspicion granulomatosis with polyangiitis. The knowledge of possibility of various presentations of acne-like lesions occurring on the face also reduces the chances of treatment with unnecessary antibiotics and topical drugs for acne. [Table - 1] shows a number of other conditions, mainly syndromes, that present with acne as a significant component.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wright AC, Gibson LE, Davis DM. Cutaneous manifestations of pediatric granulomatosis with polyangiitis: A clinicopathologic and immunopathologic analysis. J Am Acad Dermatol 2015;72:859-67.
[Google Scholar]
|
| 2. |
Comfere NI, Macaron NC, Gibson LE. Cutaneous manifestations of Wegener's granulomatosis: A clinicopathologic study of 17 patients and correlation to antineutrophil cytoplasmic antibody status. J Cutan Pathol 2007;34:739-47.
[Google Scholar]
|
| 3. |
Daoud MS, Gibson LE, DeRemee RA, Specks U, el-Azhary RA, Su WP, et al. Cutaneous Wegener's granulomatosis: Clinical, histopathologic, and immunopathologic features of thirty patients. J Am Acad Dermatol 1994;31:605-12.
[Google Scholar]
|
| 4. |
Almatrooshi M. Dermatologic Manifestations of Granulomatosis with Polyangiitis (Wegener Granulomatosis): Granulomatosis with Polyangiitis, Types of Skin Involvement, Histopathological Findings; 2018. https://www.emedicine.medscape.com/article/1085290-overview. [Last accessed on 2018 Dec 14].
[Google Scholar]
|
| 5. |
Fauci AS, Haynes BF, Katz P, Wolff SM. Wegener's granulomatosis: Prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 1983;98:76-85.
[Google Scholar]
|
| 6. |
Dosal J, Good E, Alshaiji J, De Solo S, Ricotti C, Alvarez-Connelly E, et al. Hemorrhagic acneiform lesions in a teenager as the initial presentation of granulomatosis with polyangiitis. Pediatr Dermatol 2014;31:e18-9.
[Google Scholar]
|
| 7. |
Chyu JY, Hagstrom WJ, Soltani K, Faibisoff B, Whitney DH. Wegener's granulomatosis in childhood: Cutaneous manifestations as the presenting signs. J Am Acad Dermatol 1984;10:341-6.
[Google Scholar]
|
| 8. |
Cabral DA, Uribe AG, Benseler S, O'Neil KM, Hashkes PJ, Higgins G, et al. Classification, presentation, and initial treatment of Wegener's granulomatosis in childhood. Arthritis Rheum 2009;60:3413-24.
[Google Scholar]
|
| 9. |
Gibson LE, Su WP. Cutaneous vasculitis. Rheum Dis Clin North Am 1995;21:1097-113.
[Google Scholar]
|
| 10. |
Barksdale SK, Hallahan CW, Kerr GS, Fauci AS, Stern JB, Travis WD, et al. Cutaneous pathology in Wegener's granulomatosis. A clinicopathologic study of 75 biopsies in 46 patients. Am J Surg Pathol 1995;19:161-72.
[Google Scholar]
|
| 11. |
Francès C, Du LT, Piette JC, Saada V, Boisnic S, Wechsler B, et al. Wegener's granulomatosis. Dermatological manifestations in 75 cases with clinicopathologic correlation. Arch Dermatol 1994;130:861-7.
[Google Scholar]
|
Fulltext Views
5,025
PDF downloads
2,353





