Translate this page into:
Primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder in a woman successfully treated with intralesional interleukin injection and occlusive corticosteroid
Correspondence Address:
Donghua Liu
Department of Dermatology and Venereology, First Affiliated Hospital of Guangxi Medical University, No. 6, Shuang Yong Road, Nanning
China
| How to cite this article: Jiang Y, Liu D, Alnasri A. Primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder in a woman successfully treated with intralesional interleukin injection and occlusive corticosteroid. Indian J Dermatol Venereol Leprol 2020;86:726-729 |
Sir,
Primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder can manifest as a single invasive plaque, nodule or tumour. The most common presentation is as a localized lesion and multiple lesions are rare. Currently, this disease is treated with local excision, radiation therapy, topical intralesional steroids, oral doxycycline or autologous stem cell transplant. Herein, we report a case of this disease which could be completely treated with intralesional interleukin injection and topical occlusive corticosteroid.
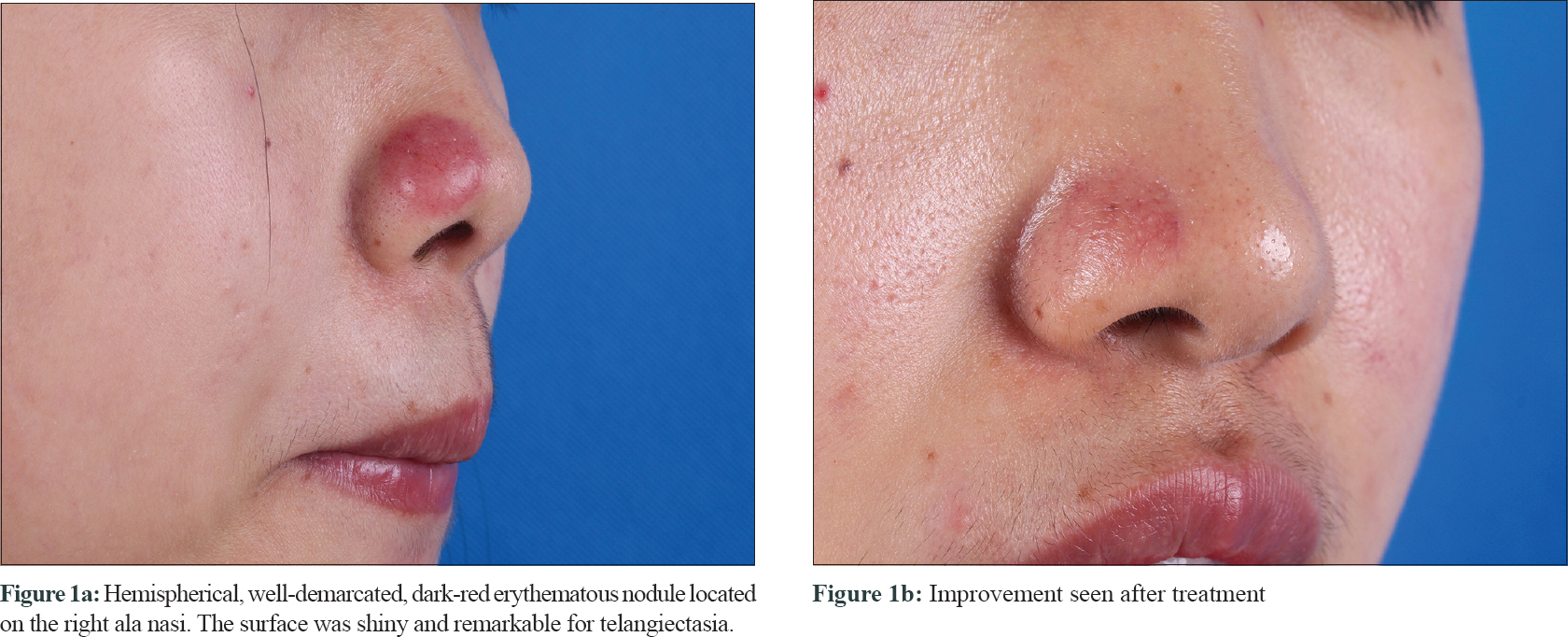
A 28-year-old woman presented with a painless nodule on her nose of one month duration. On clinical examination, there was a solitary, firm, hemispherical, dark-red erythematous nodule, with shiny surface and telangiectases, located on the right ala of the nose, of 1.8 × 1.5 cm size [Figure - 1]a.
 |
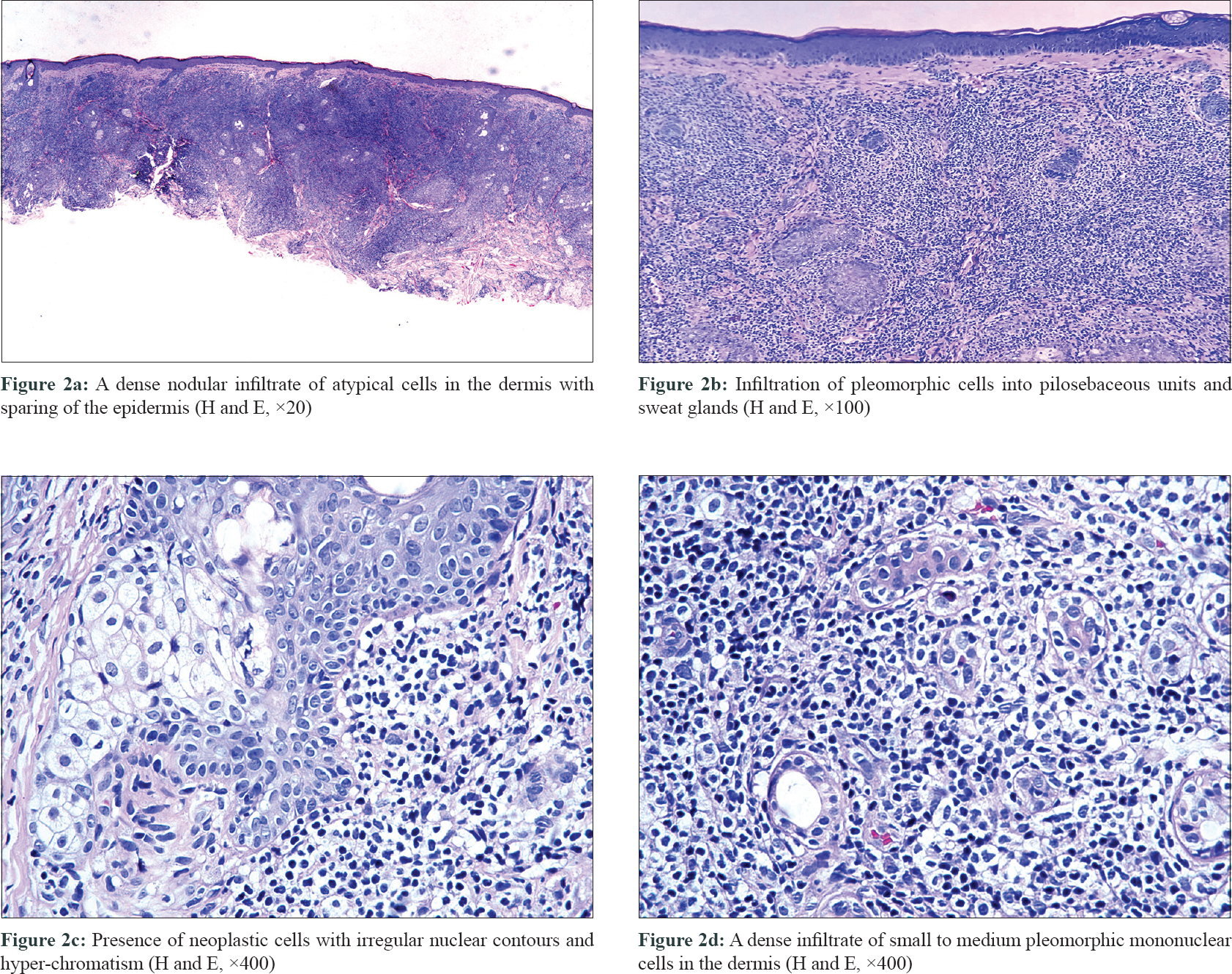
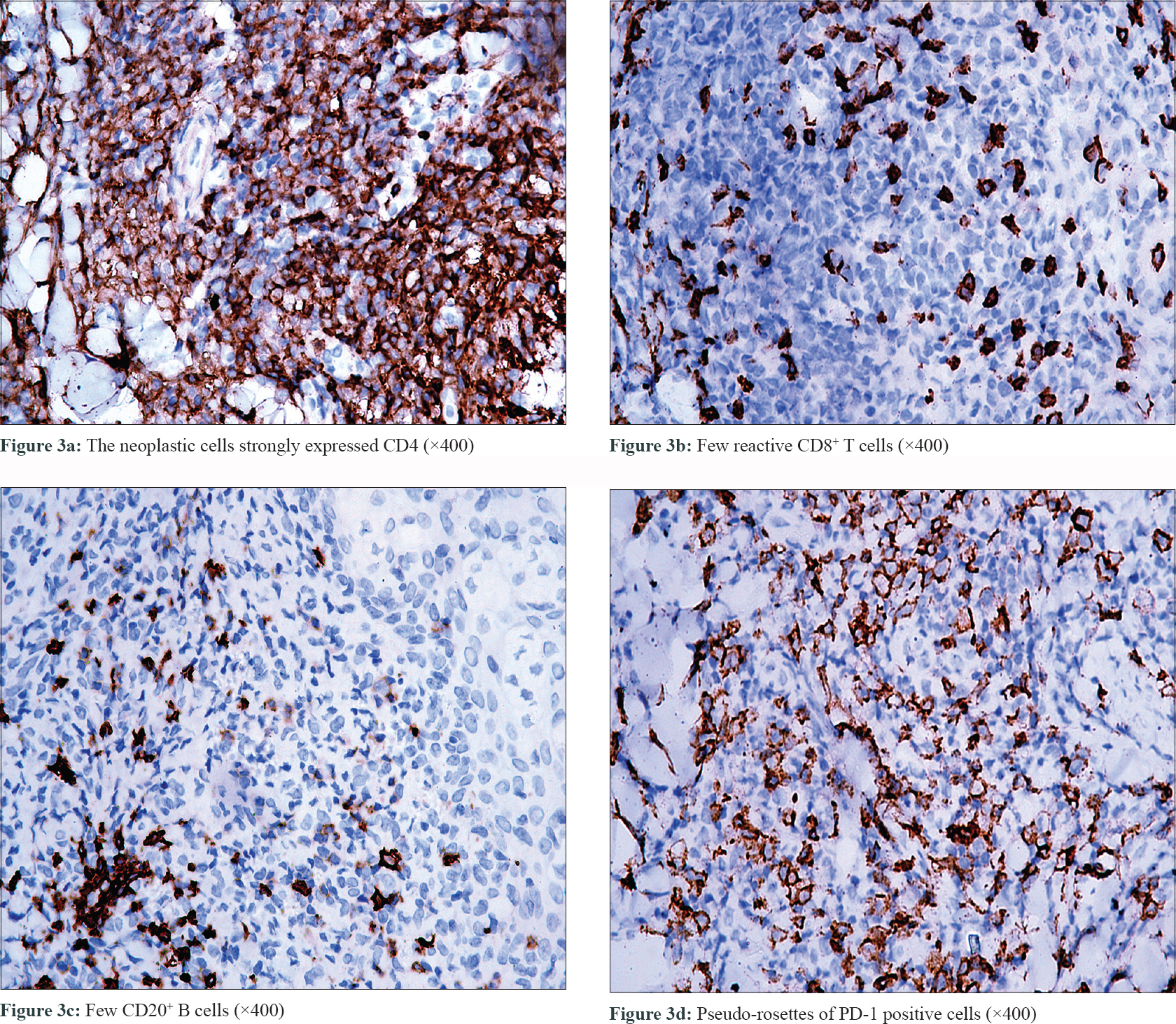
On laboratory examination, the complete blood count was normal. Histopathological examination of the nodule showed a dense infiltration of small to medium pleomorphic mononuclear cells in the dermis [Figure - 2]d. The epidermis was spared, but there was infiltration into the pilosebaceous units and sweat gland [Figure - 2]a and [Figure - 2]b. Some of the neoplastic cells had irregular nuclear contours with hyper-chromatism. There was neither eosinophil nor plasma cell infiltration [Figure - 2]c. The immunohistochemical staining revealed that the neoplastic cells strongly expressed CD3, CD4 and PD-1 positive 'pseudo-rosettes”. [Figure - 3]a and [Figure - 3]d. The neoplastic cells were negative for CD10, Mum1, TIA-1 and Tdt. There were few reactive CD8+ T cells and CD20+ B cells [Figure - 3]b and [Figure - 3]c. Proliferative index (Ki67) was approximately 30%. EBV-encoded small RNA was negative. Thus a final diagnosis of primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder was made.
 |
 |
The patient received an intralesional injection of 5lakh IU of interleukin-2 as well as one daily occlusion with flumetasone ointment for 3 weeks. The nodule disappeared completely [Figure - 1]b with no recurrence in even after 11 months of treatment.
Primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder, defined by a predominance of small- to medium-sized CD4+ pleomorphic T-cells,[1] often occurs as a single invasive plaque, nodule or tumour, without the typical macule and plaque stage of mycosis fungoides. In the 2018 WHO-EORTC classification update for primary cutaneous lymphomas, the term primary cutaneous CD4 positive small/medium T-cell lymphoma was modified to lymphoproliferative disorder.[1] The low clinical risk, localized disease and similarity to clonal drug reactions suggested that this entity should no longer be classified as an overt cutaneous lymphoma. It is characterized by a relatively indolent clinical behavior and an uncertain malignant potential. The frequency of the disease is 9% and the five-year disease-specific survival is 99%.[1] The disease is known to have a good prognosis and in order to avoid metastasis, positive treatment is still recommended. Therefore, the diagnosis requires a careful morphologic and immunophenotypic analysis, as well as molecular genetic studies.[2]
The differential diagnosis of the disease includes cutaneous lymphoid hyperplasia, mycosis fungoides, primary cutaneous follicle center lymphoma and primary cutaneous marginal zone lymphoma. The most significant difference between cutaneous lymphoid hyperplasia and this disease are the lymphocytic atypia and the loss of the pan T-cell markers. In the past, the disease was often misdiagnosed as mycosis fungoides, which classically progresses through patch, plaque and tumor stages, besides PD-1 is rarely expressed. The histopathological examination of primary cutaneous follicle center lymphoma reveals the proliferation of bcl 6+, bcl 2- follicle center cells. Another disease named primary cutaneous marginal zone lymphoma show clonal immunoglobulin rearrangements and negative CD4. Similarity in the clinical manifestation makes the diagnosis difficult, but histopathology, immunohistochemistry and molecular genetics can discriminate among those diseases. A literature review showed that the disease has no sex predominance and the prognosis was not age-related.[2] The lesion has certain common characteristics such as single lesion, small size (<3 cm), no ulceration and a low proliferative index. After topical therapy, a few cases have recurred in situ, while some recurred elsewhere and a few did not relapse. None of them had received chemotherapy.[3]
The optimal treatment for this disease is not yet defined. The treatment includes surgical resection, systemic chemotherapy, radiotherapy or immunotherapy, as well as topical corticosteroids. Of note, in a previous case report, it was mentioned that the nodule can even spontaneously regress after biopsy.[4]
According to literature, intralesional interleukin injection has been proved to have a therapeutic effect on lymphomas.[5] Considering the anti-tumor and immune enhancement effects of interleukin, we used intralesional interleukin injection in the treatment of this lymphoproliferative disorder.
In this study, the positive prognostic factors include the singularity of the lesion, small size (<3 cm) and the absence of ulceration. In conclusion, we have presented a a rare case, successfully treated by using a combination treatment of intralesional interleukin injection and occlusive corticosteroid ointment.
Acknowledgement
We would like to express my great appreciation to Prof. Yongyao Gu (Pathology Department, First Affiliated Hospital of Guangxi Medical University).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Cerroni L, Kempf W, Berti E, Facchetti F, Swerdlow SH, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood 2019;133:1703-14.
[Google Scholar]
|
| 2. |
Jain G, Aiyer HM. Primary cutaneous CD4 positive small/medium T cell lymphoma. Indian J Dermatol Venereol Leprol 2018;84:186-8.
[Google Scholar]
|
| 3. |
Maurelli M, Colato C, Gisondi P, Girolomoni G. Primary cutaneous CD4+ small/medium pleomorphic T-cell lymphoproliferative disorder: A case series. J Cutan Med Surg 2017;21:502-6.
[Google Scholar]
|
| 4. |
González Fernández D, Valdés Pineda F, Gómez Díez S, Vivanco Allende B. Primary cutaneous CD4+small/medium-Sized T-cell lymphoma with spontaneous regression after biopsy. Actas Dermosifiliogr 2015;106:767-8.
[Google Scholar]
|
| 5. |
Querfeld C, Rosen ST, Guitart J, Rademaker A, Foss F, Gupta R, et al. Phase II trial of subcutaneous injections of human recombinant interleukin-2 for the treatment of mycosis fungoides and Sézary syndrome. J Am Acad Dermatol 2007;56:580-3.
[Google Scholar]
|
Fulltext Views
3,337
PDF downloads
1,527





