Translate this page into:
Ringworm-like skin lesion is not always tinea
Correspondence Address:
Laura Atzori
Department of Medical Sciences and Public Health, University of Cagliari, Via Ospedale 54, Cagliari, 09124
Italy
| How to cite this article: Zanniello R, Ferreli C, Patta F, Pinna AL, Atzori L. Ringworm-like skin lesion is not always tinea. Indian J Dermatol Venereol Leprol 2019;85:335-337 |
History
A 20-year-old Caucasian man presented at the dermatology clinic of Cagliari University with an annular erythematous scaly lesion on the right jaw, which appeared 2 months before and was enlarging with an active border, studded with honey-colored crusts [Figure - 1]. The patient had burning and stinging sensation rather than itching. Previous treatments with topical antibiotic–steroid and antifungal formulations were not effective, and there was occurrence of a new lesion on the left nasal pyramid [Figure - 2]. The patient, who was a student of law, was not taking any drug, had no pets and played soccer as a hobby. Investigations included microbiological cultures, which excluded bacterial infections. However, microscopic examination of scraping from lesion, clarified with potassium hydroxide, revealing abundant demodex mites. More than five mites were present in the same field at very low magnification (4×). The mites were 0.3–0.4 mm long, with four legs and a long striated posterior segment, suggesting Demodex folliculorum [Figure - 3]. The patient refused to consent for a biopsy, due to the risk of unaesthetic scarring.
 |
| Figure 1: Annular erythematous scaly lesions with an active border composed of honey-colored crusts, irregular margins and clear borders on the right jaw |
 |
| Figure 2: Lesion on the left nasal pyramid |
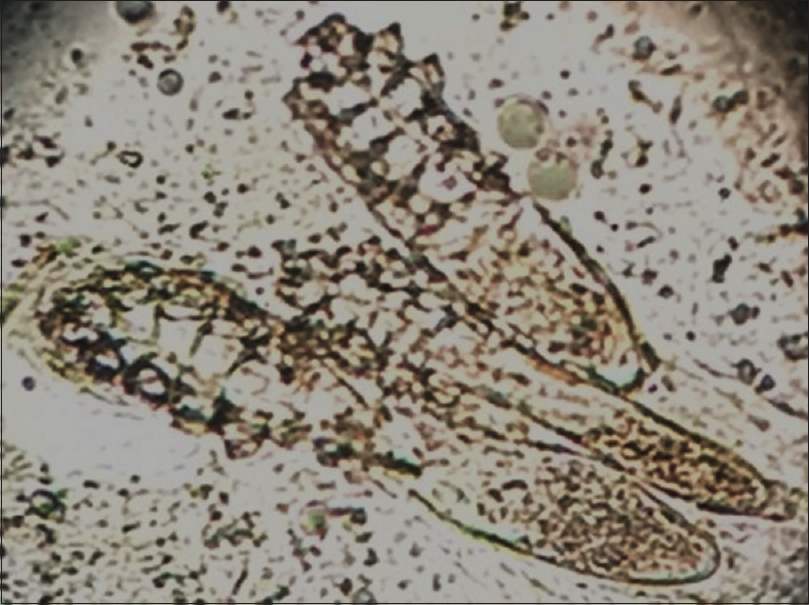 |
| Figure 3: Photomicrograph of a potassium hydroxide mount of a lesion scraping showing characteristic features of Demodex folliculorum (magnification ×10) |
What Is Your Diagnosis?
Answer
Annular demodicosis.
Discussion
Human demodicosis is still a controversial entity, because D. folliculorum and Demodex brevis are normally benign skin residents, which might become pathogenic when present in excessive number and/or because of an immune imbalance.[1] Classification defines two different forms: primary forms, characterized by the absence of preexisting or concurrent inflammatory dermatoses, abnormal mite colonization and healing after adequate acaricides treatment; and secondary demodicosis, usually associated with systemic or local immunosuppression.[1],[2],[3] The presence of abundant demodex mites (more than 5 mites per cm[2]) on microscopic examination,[3] the absence of preexisting dermatosis and response to acaricidal cream, in our case, is consistent with a primary infestation. Morphology of the mite is suggestive of D. folliculorum, because D. brevis is usually rounder and 0.15–0.2 mm shorter in length.[1] Treatment with topical ivermectin 10 mg/g cream once daily resulted in an almost complete clinical resolution after 15 days [Figure - 4], but direct microscopy was still positive. Maintenance of the treatment for 2 months led to clinical and direct microscopic clearance at follow-up visit, with no relapses in the following 6 months.
 |
| Figure 4: Almost complete clinical resolution of the lesions after 15 days of topical ivermectin |
Skin lesions induced by demodex mites develop as a consequence of mechanical blockage of follicles, with release and accumulation of products that cause local inflammation, as well as due to host-mediated foreign body and delayed hypersensitivity reaction to mite antigens.[2] Incidence shows a characteristic biphasic curve, with first peak during early adulthood, coinciding with the maximal sebum production and another in old age, when immune activity decreases. In recent years, demodex parasitism has been associated with a variety of clinical manifestations: The spinulate demodicosis, also known as pityriasis folliculorum, the rosacea-like demodicosis and a more pronounced inflammatory condition, named papulo-pustular/nodulo-cystic or conglobate demodicosis, affecting most commonly the perioral and periorbital areas.[3] Association with ocular and auricular involvement is also frequent, while in an elderly man, demodicosis can characteristically affect the scalp.[3],[4]
We described an unusual clinical presentation of demodicosis, mimicking tinea faciei, for the well-demarcated annular lesions, with centrifugal extension. A previous similar observation proposed the name of “annular demodex dermatitis.”[4] Our case presented with a more pronounced inflammation, with serous crusting at the periphery, suggesting impetigo, which in young adult might also represent a manifestation of acquired immune suppression. The HIV test and other routine hematological examinations confirmed the patient's immune competence. A skin biopsy was not performed, because of the presence of lesions on the face, as well as for the rapid improvement with topical ivermectin. We chose this topical acaricide because of its proven efficacy and high tolerability in facial rosacea.[5] Other suggested topical treatments include permethrin 5%, metronidazole, salicylic acid, retinoids and crotamiton with variable results, while the use of systemic agents, such as ivermectin and metronidazole, are reserved to very recalcitrant cases. As regards the pathogenesis, previous incongruous treatments with mixed corticosteroid antibiotic products were suggested as the cause of the exacerbation of symptoms and very atypical presentation in previous reports[6],[7]. This may be relevant in our patient too. We found no other usual triggering factors for the mite infestation, but the patient's habit of repeated daily washing of face with aggressive cleaners to prevent fungal infections, followed by the use of grease creams after sport activities might have altered the natural commensal flora and favored the demodex pathomorphosis. Early diagnosis in atypical presentations is important to avoid prolonged illness and incongruous treatments. This case highlights the need to consider demodicosis among the causes of annular lesions on the face.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rather PA, Hassan I. Human demodex mite: The versatile mite of dermatological importance. Indian J Dermatol 2014;59:60-6.
[Google Scholar]
|
| 2. |
Jarmuda S, O'Reilly N, Zaba R, Jakubowicz O, Szkaradkiewicz A, Kavanagh K, et al. Potential role of demodex mites and bacteria in the induction of rosacea. J Med Microbiol 2012;61:1504-10.
[Google Scholar]
|
| 3. |
Chen W, Plewig G. Human demodicosis: Revisit and a proposed classification. Br J Dermatol 2014;170:1219-25.
[Google Scholar]
|
| 4. |
Martinez-Diaz GJ, Clark KM, Vasquez JG, English JC 3rd. Facial erythematous annular plaques: A case of annular demodex facial dermatitis? J Am Acad Dermatol 2012;67:e268-9.
[Google Scholar]
|
| 5. |
Siddiqui K, Stein Gold L, Gill J. The efficacy, safety, and tolerability of ivermectin compared with current topical treatments for the inflammatory lesions of rosacea: A network meta-analysis. Springerplus 2016;5:1151.
[Google Scholar]
|
| 6. |
Karincaoglu Y, Tepe B, Kalayci B, Seyhan M. Pseudozoster clinical presentation of demodex infestation after prolonged topical steroid use. Clin Exp Dermatol 2008;33:740-2.
[Google Scholar]
|
| 7. |
Sakuntabhai A, Timpatanapong P. Topical steroid induced chronic demodicidosis. J Med Assoc Thai 1991;74:116-9.
[Google Scholar]
|
Fulltext Views
13,328
PDF downloads
2,124





