Translate this page into:
Erythematous scaly facial plaques with overlying hair loss
Correspondence Address:
Neetu Bhari
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Narayanan A, Ramam M, Bhari N. Erythematous scaly facial plaques with overlying hair loss. Indian J Dermatol Venereol Leprol 2019;85:347 |
A 17-year-old boy presented with multiple, well-defined, erythematous plaques of variable sizes with fine scales on the forehead, supraorbital area, nose, cheeks, chin and neck [Figure - 1] of two months duration. They were gradually progressive and asymptomatic. Most of the plaques showed prominent follicular openings while those on the eyebrow and beard showed overlying loss of hair. There was no associated loss of sensation, lymphadenopathy or constitutional features such as fever or weight loss.
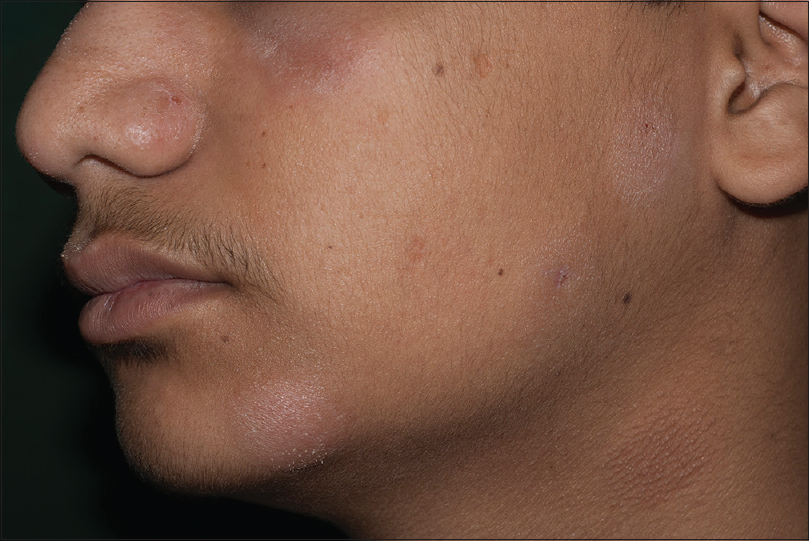 |
| Figure 1: Well-defined, scaly, erythematous plaques on face and neck |
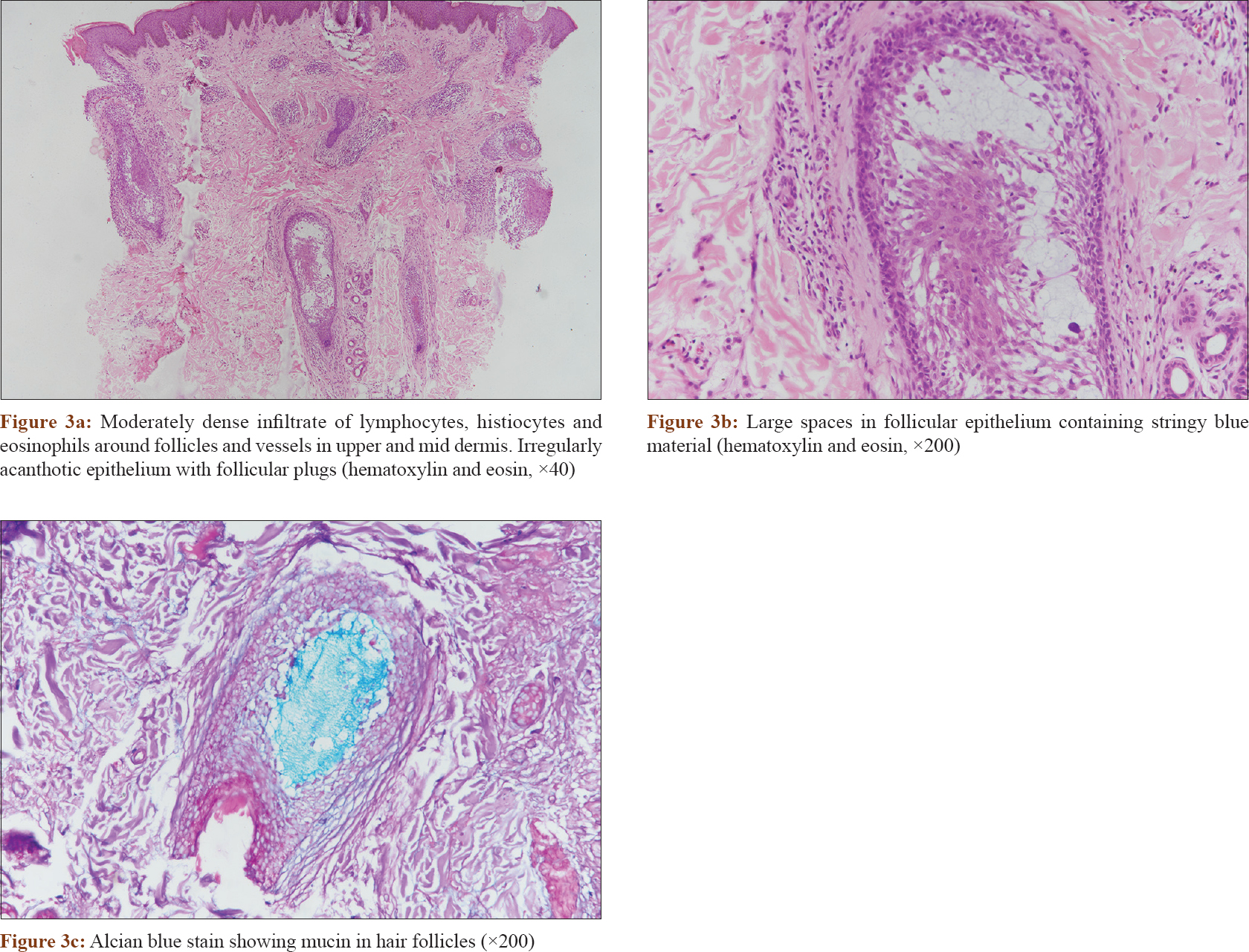
Dermoscopy showed presence of dilated follicular ostia with follicular plugs of amorphous material [Figure - 2]. On histopathological evaluation, there was a moderately dense infiltrate of lymphocytes, histiocytes and eosinophils around the follicles and the vessels in the upper and mid dermis. The overlying epithelium was irregularly acanthotic with some follicular plugs. Hair follicles in the dermis showed large spaces in the follicular epithelium containing stringy blue material [Figure - 3]a and [Figure - 3]b. Alcian blue stain showed the material in the follicles to be mucin [Figure - 3]c.
 |
| Figure 2: Dilated follicular ostia with follicular plugs of amorphous material (Heine Delta 20T, polarized, ×10) |
 |
Question
What is your diagnosis?
Answer
Follicular mucinosis/alopecia mucinosa.
Discussion
Follicular mucinosis/alopecia mucinosa was first described by Pinkus in 1957 as a process of mucinous follicular degeneration leading to alopecia. Clinically, lesions present as single or multiple well-defined, erythematous, alopecic plaques with occasional scaling and follicular papules on the surface, usually involving the face and scalp. The follicular ostia may be dilated with keratin, and mucin may be squeezed out from the plaques.[1]
Atypical clinical presentations simulating folliculitis, alopecia areata, scarring alopecia, chronic eczema, acne, urticaria and erythroderma have been reported. The histopathology demonstrates mucin deposition within the external root sheath and sebaceous gland along with an infiltrate of lymphocytes and eosinophils surrounding hair follicles.
There are two main clinicopathological variants: primary follicular mucinosis and lymphoma-associated follicular mucinosis. The primary variant usually affects children and young adults, whereas the lymphoma-associated variant is seen in adults. However, both forms show significant overlap of clinical and histological features.[2] Lymphocytes with enlarged hyperchromatic nuclei with irregular contours were significantly more frequent in the lymphoma-associated variant, whereas deposition of mucin in cystic spaces within hair follicles was significantly more frequent in the primary variant.[3] Further, in lymphoma-associated follicular mucinosis, 60% had dense lymphoid infiltrates with some features of epidermotropism of lymphocytes compared with 47% in the primary follicular mucinosis group, suggesting a cutaneous lymphoproliferative process.[3]
There are no standard recommendations for the treatment of follicular mucinosis. Primary follicular mucinosis resolves spontaneously in 2–24 months. Therapeutic modalities include topical corticosteroids, topical retinoids, oral isotretinoin, dapsone, indomethacin, minocycline, psoralen ultraviolet-A, narrow-band ultraviolet-B, cyclophosphamide and methotrexate, but none showed consistent efficacy.[4],[5] Treatment of lymphoma-associated follicular mucinosis involves treatment of the underlying disorder.
Our patient was counselled regarding the prognosis and was treated with 0.1% tacrolimus cream on the lesions and showed almost complete clearance of lesions over the next two months. At a subsequent visit two months later, he reported three new similar plaques on the cheek and neck.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Passos PC, Zuchi MF, Fabre AB, Martins LE. Follicular mucinosis – Case report. An Bras Dermatol 2014;89:337-9.
[Google Scholar]
|
| 2. |
Cerroni L, Fink-Puches R, Bäck B, Kerl H. Follicular mucinosis: A critical reappraisal of clinicopathologic features and association with mycosis fungoides and Sézary syndrome. Arch Dermatol 2002;138:182-9.
[Google Scholar]
|
| 3. |
Rongioletti F, De Lucchi S, Meyes D, Mora M, Rebora A, Zupo S, et al. Follicular mucinosis: A clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides-associated follicular mucinosis. J Cutan Pathol 2010;37:15-9.
[Google Scholar]
|
| 4. |
Parker SR, Murad E. Follicular mucinosis: Clinical, histologic, and molecular remission with minocycline. J Am Acad Dermatol 2010;62:139-41.
[Google Scholar]
|
| 5. |
Kim KR, Lee JY, Kim MK, Yoon TY. Successful treatment of recalcitrant primary follicular mucinosis with indomethacin and low-dose intralesional interferon alpha. Ann Dermatol 2009;21:285-7.
[Google Scholar]
|
Fulltext Views
3,096
PDF downloads
2,233





