Translate this page into:
Do primary care physicians require training in core clinical dermatology? A cross sectional needs assessment study from Western India
2 Department of Community Medicine, GMERS Medical College, Vadodara, Gujarat, India
Correspondence Address:
Paragkumar D Chavda
Department of Community Medicine, GMERS Medical College, Gotri, Vadodara, Gujarat
India
| How to cite this article: Thakkar SH, Chavda PD, Mehta KG. Do primary care physicians require training in core clinical dermatology? A cross sectional needs assessment study from Western India. Indian J Dermatol Venereol Leprol 2019;85:380-387 |
Abstract
Background: Primary care physicians play a crucial role in managing patients with common skin disorders who form around one-third of outpatient attendees.
Aim: This study aimed to assess the need for dermatology training among primary care physicians by assessing their knowledge, self-perception of ability to diagnose and manage skin disorders, and their difficulties in managing these patients.
Methods: A descriptive, cross-sectional, needs assessment study was done among primary care physicians (n = 61) of rural (n = 34) and urban (n = 27) areas of Vadodara district. A pre-validated semi-structured questionnaire (for self-rating of the ability to diagnose/manage skin disorders and difficulties faced in managing patients) was used along with a photo-quiz (for knowledge assessment) while approaching primary care physicians during their monthly review meeting with prior permission. Data were analyzed by Epi InfoTM software and manual content analysis.
Results: The mean score on the photo-quiz was 4.1/10. Forty-three (70.5%) participants rated their ability to diagnose/manage skin disorders as 'average' on a five-point Likert scale. Various difficulties (n = 89) narrated by participants were related to their knowledge/skill, disease factors, patients and administrative aspects. Three-fourths of the participants managed difficulties by referring patients to dermatologists. One-third suggested conducting training in common skin disorders.
Limitations: The study population included primary care physicians from the government healthcare setup only. Knowledge assessment was done using a short ten-item photo-quiz instead of actual patients.
Conclusions: Primary care physicians had poor knowledge of skin disorders, and a majority overrated their own ability for clinical management of these disorders. Most common difficulties faced were related to clinical management. There is a need for training on common skin disorders.
Introduction
Patients with common skin disorders make up 25–35% of all patients attending primary health centres where they are managed by primary care physicians.[1] The rural population (around 80% of the total population of India) has no easy access to a dermatologist.[2]
Primary care physicians working in a government setup have access to training in various national health programs including sexually transmitted infections/human immunodeficiency virus (STI/HIV) and leprosy, which relate to dermatology.[3] However these training modules do not cover common skin disorders.
We found only a few studies on the need for clinical dermatology training at the primary healthcare level,[4],[5] and no Indian studies on the need for primary care physicians' training in common skin disorders.
The aim of this study was to determine the training need in dermatology among primary care physicians. Study objectives were (i) to evaluate among primary care physicians their knowledge and self-perception of the ability to diagnose and manage common skin disorders and (ii) to explore the difficulties faced by them in managing common skin disorders.
Methods
Ethical issues
The study was started after taking approval from Institutional Human Ethics Committee of GMERS Medical College and Hospital, Vadodara, Gujarat, India.
Study design
This was a descriptive cross-sectional, needs assessment study.
Study setting
The study was done among urban and rural primary care physicians of Vadodara district in central Gujarat, from May 2016 to July 2016.
Study participants
Primary care physicians working in the government healthcare setup were included. Primary care physicians from rural areas were working as medical officers either at the primary health centres or community health centres; and those from the urban areas, were working as medical officers at urban primary health centres. We excluded doctors in administrative posts such as taluka health officers, zonal officers, medical superintendents and AYUSH (Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homoeopathy) officers. After this, we had 52 and 34 eligible primary care physicians from rural and urban areas respectively. Out of these, we could collect responses from 34 rural and 27 urban primary care physicians, yielding a total sample size of 61.
Study instrument
The study instrument was a semi-structured questionnaire. The first draft of the study instrument was validated for content by two dermatologists and two public health experts. This version was pilot-tested on a group of five medical officers from another district before using it in the present study.
The questionnaire was divided into two parts. Part I comprised a photo-quiz. Part 2 focused on self-rating of skills and the difficulties faced by primary care physicians in managing skin disorders. A part of the questionnaire also included their perception of dermatology teaching in undergraduate training, which is not presented in this paper.
The photo-quiz contained 10 image-based multiple-choice questions, each having only one correct answer out of given choices. The questions on diagnosis, management and referral need were placed at random in an even/odd fashion with the weightage of 4:4:2. As primary care physicians are expected to know only basic dermatology, the items selected for the photo-quiz pertained to core clinical dermatology, as per the Medical Council of India undergraduate curriculum.[6] We included common skin disorders viz., scabies, tinea, herpes zoster, vitiligo, leprosy and sexually transmitted infections.
Photographs were taken from the personal image-bank of the first author. Photographs along with the question and possible answers were displayed on a PowerPoint slide. A sample photo-quiz question is shown in [Figure - 1]. Participants were asked to indicate their answer on individual paper-based response sheets. We checked for post-test reliability of the photo-quiz using Cronbach's alpha, which was 0.44.
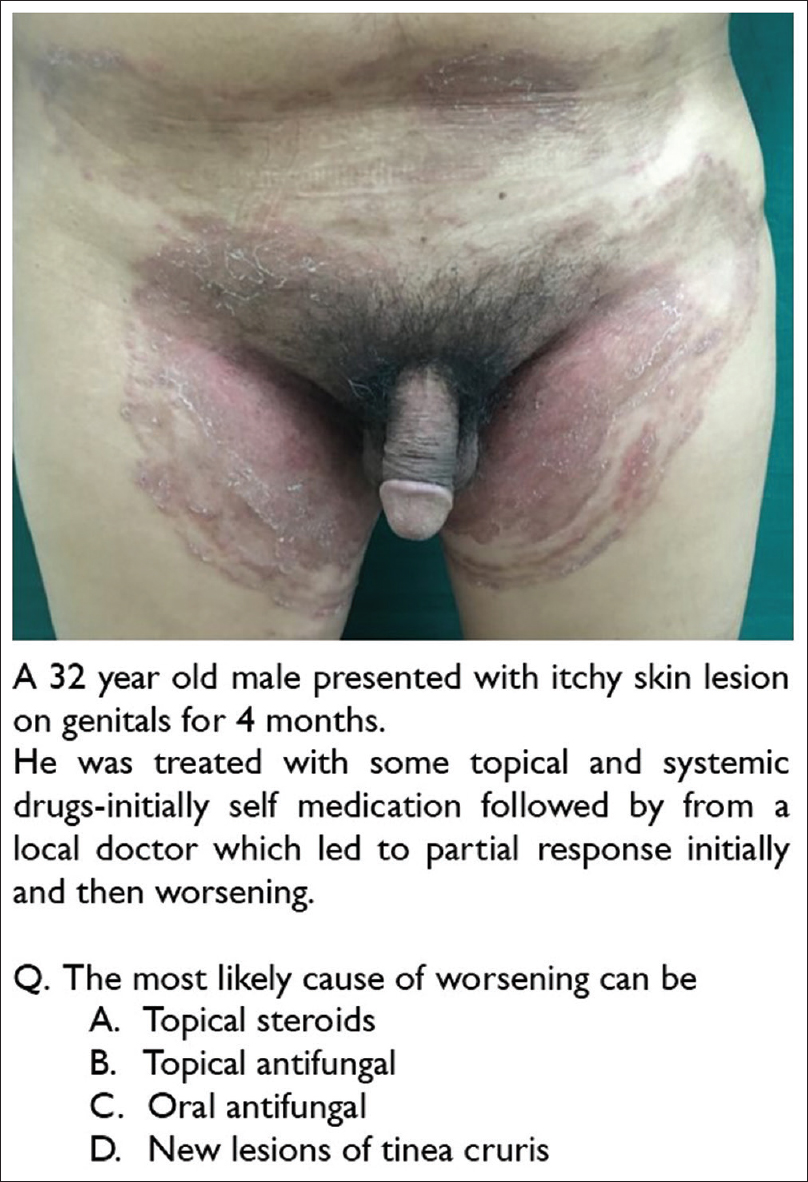 |
| Figure 1: A sample question from the photo-quiz |
In part II of questionnaire, participants' self-rating of their ability to diagnose and manage common skin disorders was collected on a five-point Likert scale (very bad/bad/average/good/very good). We also asked them the frequency of referral to a dermatologist on a five-point Likert scale (always/usually/sometimes/rarely/never).
The part II of the questionnaire also contained three open-ended questions as follows: (1) What are the difficulties that you face in managing patients with skin problems? (2) How do you handle it currently? (3) Any suggestions to overcome these difficulties? The responses were provided by participants in their own handwriting in English in the open space provided in the questionnaire.
Data collection
The rural and urban health authorities routinely conduct monthly review meetings with medical officers. We utilized this opportunity to obtain access to the medical officers for collecting the data for this study. Prior permission was taken from the Chief District Health Officer for rural areas and the Chief Medical Officer for urban areas. The data were collected in two sessions each for rural and urban primary care physicians. The data collection was done by both the first and second author. It was ensured that participants should not use any educational material or smart phones/any other gadgets during the session.
The data collection process for this study was divided in four parts. The same sequence was followed for both rural and urban sessions. As the first step, a verbal informed consent was taken from the study participants. Second step was conducting photo-quiz on power-point, run by first author and facilitated by second author. Third step was completing the part II of the questionnaire self-administered by participants in English. Fourth step was sharing the correct answers of photo-quiz with the participants and solving their queries regarding the same. This was done to provide the physicians an opportunity to clear their concepts and/or bridge their knowledge gaps.
Data analysis
The answer-sheets of photo-quiz were evaluated manually by first author giving score out of ten where each correct answer scored one mark. Quantitative data were entered in a Microsoft Office Excel spreadsheet and analyzed by Epi Info™ software version 6.04d. Analysis of the qualitative information was carried out by the first author (female, dermatologist) and the second author (male, public health expert, trained and experienced in qualitative research). A manual content analysis was performed independently by both these authors to identify emerging themes. Thus, themes were derived from the data (inductive approach). Later, this analysis was reviewed by the third author. The differences between the researchers were resolved through discussion. This analysis is presented in a tabular form.
Results
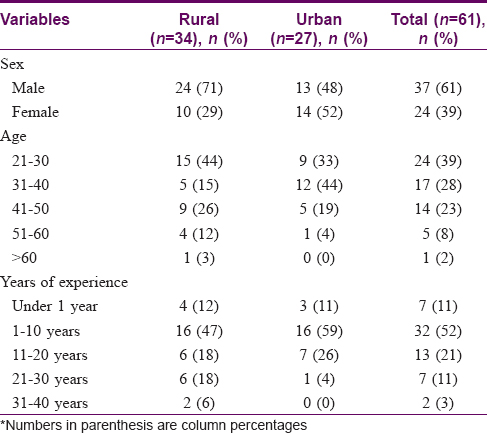
Of the 61 study participants, 37 were males and 24 were females, with a mean age of 36 years. The youngest participant was 23 years old, and 24 (39%) participants were under 30 years of age. Nearly half of the participants had less than 10 years of clinical experience [Table - 1]. Except for two physicians who had worked in the skin department of a tertiary centre for 3 and 9 months respectively, participants had not received any prior training related to common skin disorders. Six of them had taken training related to sexually transmitted diseases/HIV and six in leprosy.
The self-reported average number of total daily outpatients seen by participants was 46.7 (range, 20–100), while the average number of patients presenting daily with skin disorders was 8 (range, 1–35). The proportion of patients with skin disorders was about 17% of total outpatients seen.
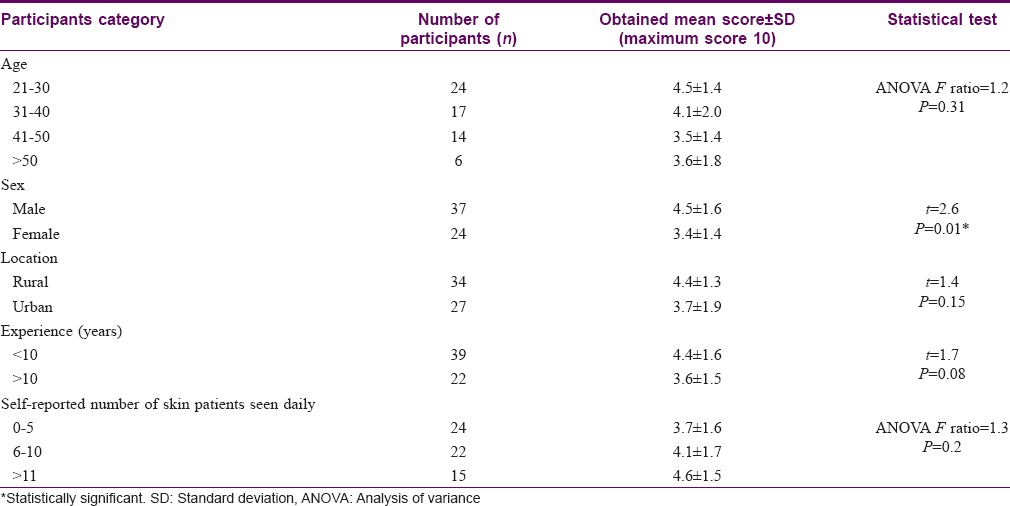
The mean (±SD) score achieved by all participants (n = 61) in the photo-quiz was 4.1 (±1.7) out of 10. Mean (±SD) scores in diagnosis, management and referral knowledge were 2.1 (±1.1), 1.2 (±1.0) and 0.8 (±0.5) out of 4, 4 and 2 marks respectively. In all, 54 (88.5%) participants scored 50% or less marks.
On analyzing the scores in different subgroups among the participants, it was observed that younger participants (those with less than 10 years' experience) had marginally better (statistically non significant) scores compared to more senior participants. Similarly, rural participants had marginally better (statistically non significant) scores compared to their urban counterparts. The mean score of male participants was significantly higher than that of female participants. Participants who saw a higher number of skin patients also had a marginally better score [Table - 2].
Analyzing the answers to individual questions on photo-quiz, the highest correct response was obtained for a question on tinea (78.7%), followed by one on a drug reaction (Stevens–Johnson syndrome, 75.4%) and then one on acne (72.1%). Most of the participants could not correctly answer questions related to scabies, pellagra and sexually transmitted infections [Table - 3]. A total of 91.8% of the participants could not identify the need for referral when they were not clear regarding diagnosis of the condition shown in the quiz. In this question of photo-quiz, despite the possibility of the condition being infective 37 (60.6%) of the participants intended to use combination therapy including topical corticosteroids.
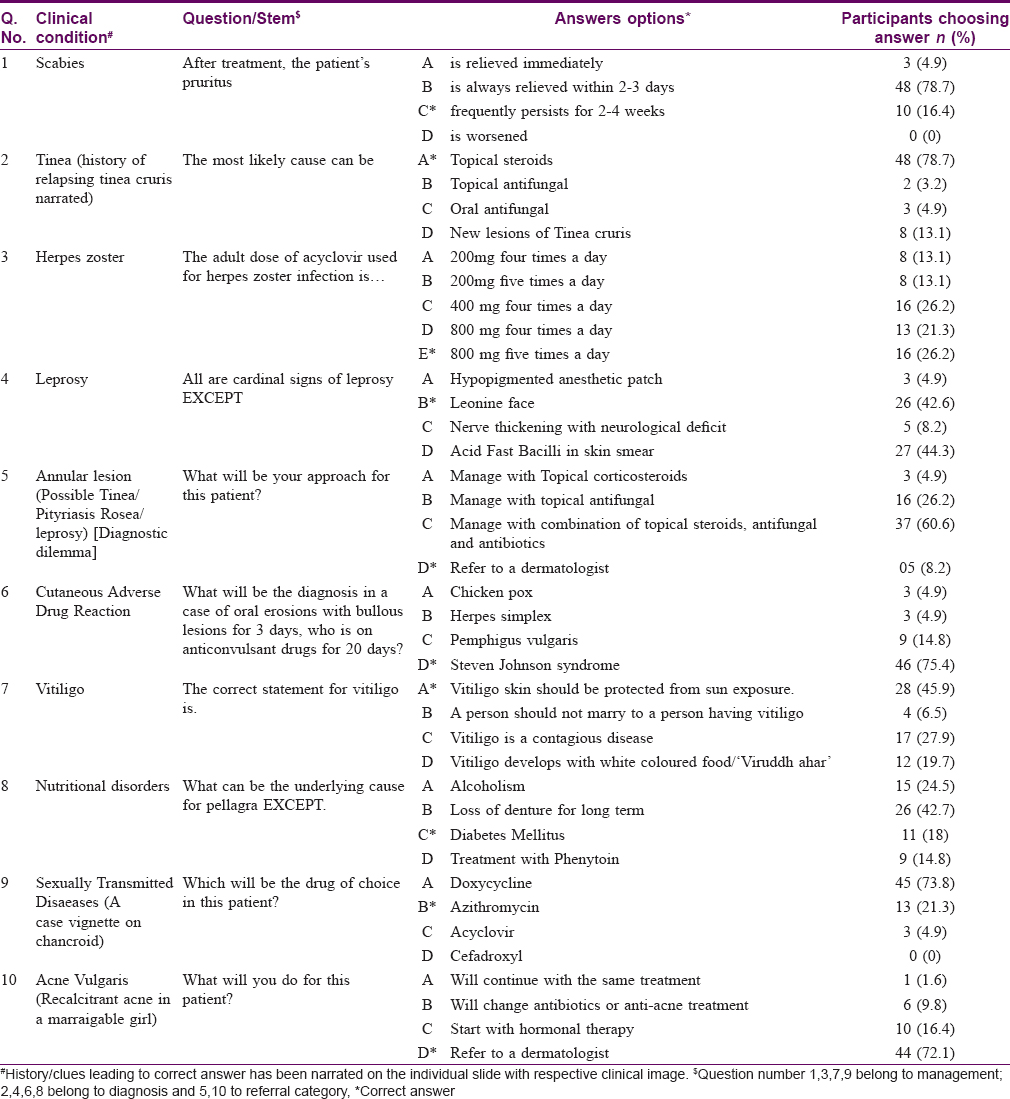
Forty-three (70.5%) participants rated their ability for both diagnosis and management as average on Likert scale [Figure - 2]. The correlation coefficient (r) for photo-quiz scores and self-rating of ability to diagnose and manage skin disorders was 0.01 and 0.2 respectively, indicating poor correlation.
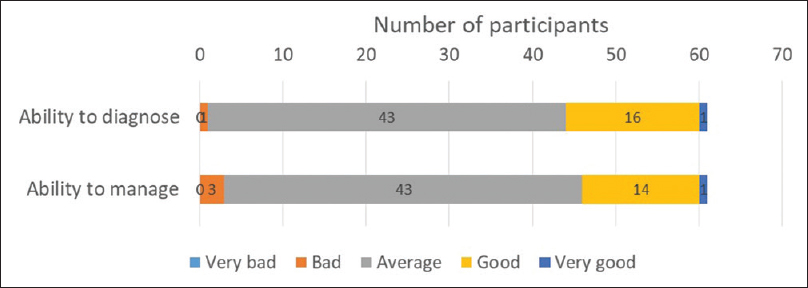 |
| Figure 2: Self-rating by study participants on their ability to diagnose/manage patients with skin problems (n = 61) |
On a Likert scale, 17 (27.8%) participants indicated that they 'usually' referred skin patients to a dermatologist while the rest said 'sometimes.'
In response to an open-ended question, 55 of the 61 participants mentioned difficulties in dealing with skin patients. In all, 89 difficulties were mentioned. Forty-seven participants (67 responses) mentioned various ways they handled these difficulties, and 39 participants (53 responses) suggested different ways to overcome these difficulties [Table - 4]. We could identify four common themes among these difficulties: 'knowledge/skill-related,' 'disease-related,' 'patient-related' and 'administrative aspects.'
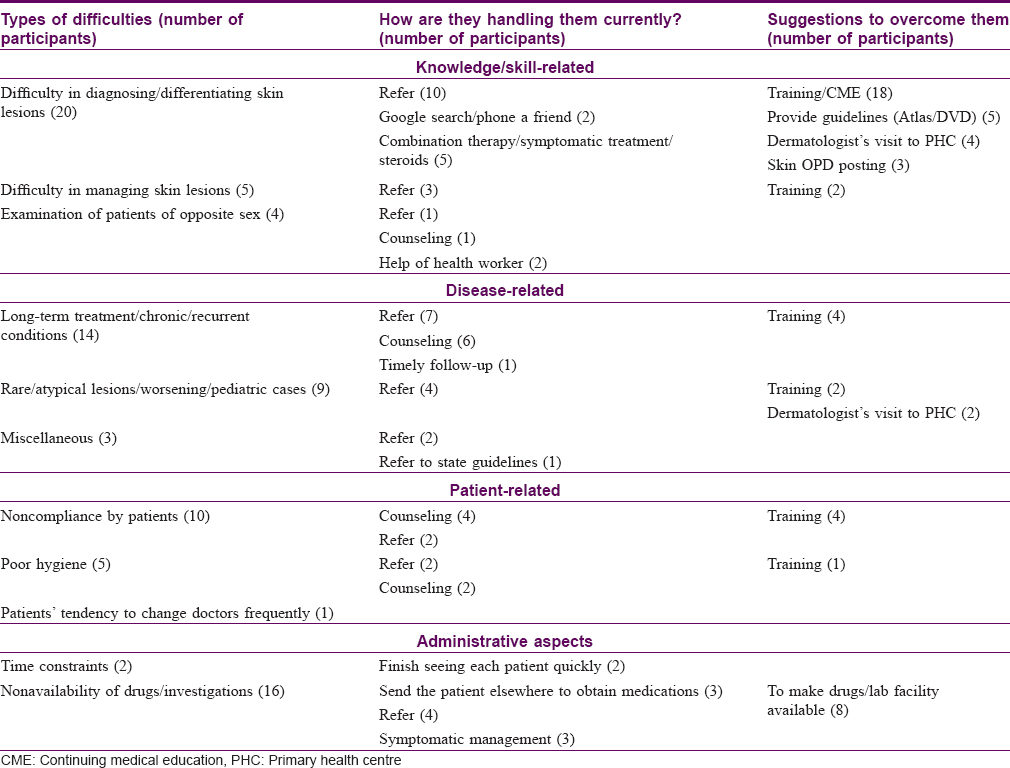
A total of 29 difficulties were grouped under the category 'knowledge/skill.' Most responses in this category were related to difficulties in arriving at a differential diagnosis in skin disorders and difficulties in managing skin patients.
Difficulties (26) under the 'disease' category included skin diseases requiring chronic treatment or recurrent lesions, atypical or rare lesions as well as skin disorders in the pediatric age group. Certain diseases were sub-classified as 'miscellaneous' under these disease related difficulties, including mixed infections, allergic disorders and diabetes-associated skin disorders.
Difficulties (16) mentioned under the category 'patient' were related to noncompliance with treatment by patients and poor personal hygiene maintained by them. Difficulties (18) in the 'administrative' area pertained to the non availability of certain drugs and investigations required for skin disorders.
As regards handling these difficulties, a majority of the participants (35/47) reported that they refer patients to a dermatologist or higher centre when in a dilemma. Other ways of handling difficulties were managing associated conditions, giving rational therapy whenever possible and timely follow-up.
When suggestions for improvement were sought, a majority of the participants (36/55) suggested that training or continuing medical education programs should be conducted. Some suggested providing guidelines/color atlases and treatment protocols to in-service doctors. There were also suggestions for dermatologist visits to primary health centres, and primary care physicians' posting in specialist skin outpatient departments at the referral centre for hands-on training.
Discussion
Primary care physicians are the backbone of the healthcare system. Their knowledge and competence play a vital role in treating skin disorders. Understanding the issues they face and identifying gaps in the management of patients with skin disorders can help strengthen the healthcare system.
The self-reported proportion of patients presenting with skin disorders out of the total outpatient attendees was 17% in this study which correlates with figures in other studies. Some studies reported this proportion as ranging between 11 and 24%, whereas others reported it to be 8-15%.[7],[8],[9]
On evaluating knowledge with the photo quiz, 88.5% of our participants scored less than 50% marks. They scored better in the diagnostic area than in management and referral areas. Al-Zahrani et al. also showed that 69.5% of primary healthcare physicians had insufficient knowledge of common skin disorders.[10] Another study from Mali, reported in a WHO bulletin, stated that primary care workers were unclear about the diagnosis for almost one-third of skin patients, leading to inadequate treatment.[11]
We found an interesting dichotomy in the physicians' response to clinical dilemma as reported by them on open ended question versus what was observed on photo-quiz. On open ended questions most physicians reported that in case of clinical dilemma they referred the case to dermatologist or prescribed rational treatment. However, on a particular photo-quiz question checking their knowledge for the referral need as high as two third participants chose to prescribe a combination therapy including topical corticosteroids despite the possibility of the condition being infective. Previously Shaffer et al. have shown disproportionate use of topical clotrimazole/betamethasone by family physicians in the United States.[12] Bahelah et al., in a study from Yemen, also observed that 50% of primary care physicians intended to use corticosteroids in fungal infections.[13] This practice of cocktail therapy by primary care physicians in cases of diagnostic difficulty has also been frequently observed by the first author of this study, with patients referred to the skin department. Such therapy using topical steroids with antimicrobials can lead to irreversible side effects, recurrences of disease, resistant infections and transmission to others. Misuse of topical corticosteroids also alters the presentation of skin lesions, making it more difficult to be diagnosed or managed by primary care physicians and even for the dermatologist.
We observed a poor correlation between the physicians' objective score on the photo-quiz and their self-perception (self-rating) of ability to diagnose/manage patients with skin disorders. Even those who had a poor score in the photo-quiz rated their ability to diagnose/manage skin disorders at 3 or 4 on a five-point Likert scale. Evans et al. have documented that self-perception of doctors in general does not necessarily correlate with clinical competence.[14] However, contrary to these findings, Bahelah et al., and Kirsner and Federman found objective and subjective assessments correlating in their studies.[13],[15]
The difficulties reported by participants in this study were related to clinical management and administration. Difficulties in clinical management were related to the knowledge/ability of clinicians (29), patients' attitude (14) and disease-specific problems (23). One-third of the participants narrated difficulties related to their own competence in managing skin disorders. Most of the participants said that they managed patients by referring them to a dermatologist, using a Google search, or with the help of a colleague. They also tried to counsel the patients as and when needed.
As suggested by a majority of the participants, training in dermatology can help them cope with many of their difficulties. A few of them suggested the need for periodic updating of knowledge. Kerr et al. also found the need for training in 80% of primary care physicians, which should be followed by regular (e.g., five-yearly) updates.[16] In the present study, nine participants felt that they should either be posted in a tertiary centre or a dermatologist should visit the primary health centre for better patient management. In a study by Vallikunnu et al., 66% of the doctors indicated the usefulness of their interaction with specialists in secondary and tertiary care hospitals.[17] A study among general practitioners in the UK by Harlow and Burton suggested several areas where a dermatology department could help primary care physicians viz., conducting continuing education programs (including practical skills), preparing guidelines and protocols for primary care physicians, and providing them updated information regularly, among others.[18]
Conclusions
Primary care physicians scored poorly on their knowledge of common skin disorders. However they perceived their ability to diagnose/manage skin disorders as average. They reported difficulties related to clinical management and administrative aspects while dealing with patients having skin diseases. Training pertaining to common skin disorders was one of the common suggestions made by them to help them increase their clinical competence.
Limitations
The study population essentially included primary care physicians from the government healthcare setup only. The value of Cronbach's alpha was low for the photo-quiz, indicating poor reliability. One reason for this could be the small size of the photo-quiz. While deciding the number of items for this test, we had to strike a balance between covering the curriculum and the feasibility of data collection. Due to the limited time available for data collection, we could include only 10 items in the quiz. Photographs were used instead of actual patients for knowledge assessment, which may be another limitation.
Recommendations
There is no formal training program available to in-service primary care physicians covering common dermatology disorders, and this study brings attention to the need for such a training program to address the needs of the current pool of primary care physicians. As a long-term solution to this issue, it would be prudent to increase the focus on dermatology in the undergraduate medical curriculum.
Acknowledgement
This study has been done as part of Advance Course in Medical Education (ACME) at MCI Nodal Centre for Faculty Development at the NHL Medical College, Ahmedabad for the first author. We would like to thank the ACME faculty and colleagues for their guidance and help. A special thanks to Dr. P. V. Vijayaraghavan, for his valuable help in conceptualization of this study. We would like to thank Dr. Chhari, Chief District Health Officer, Vadodara and Dr. Devesh Patel, Medical Officer of Health, Vadodara Municipal Corporation for providing access to primary care physicians for conducting this study during their scheduled meetings. We thank Dr. Raksha Patel and Dr. Roshni Vahora from the Department of Dermatology, GMERS Medical College, Vadodara for their help in conducting this study. We thank Dr. Neena Doshi for rendering valuable help in language editing of the article.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kaur P, Singh G. Community dermatology in India. Int J Dermatol 1995;34:322.
[Google Scholar]
|
| 2. |
Verma S. Nonclinical challenges of Indian dermatology – Cities vs. villages, poverty, and lack of awareness. Int J Dermatol 2007;46 Suppl 2:42-5.
[Google Scholar]
|
| 3. |
Indian Public Health Standards (IPHS) Guidelines for Primary Health Centres Revised 2012. New Delhi: Directorate General of Health Services Ministry of Health and Family Welfare Government of India; 2012. Available from: http://www.nhm.gov.in/images/pdf/guidelines/iphs/iphs-revised-guidlines-2012/primay-health-centres.pdf. [Last accessed on 2018 May 27].
[Google Scholar]
|
| 4. |
Hansra NK, O'Sullivan P, Chen CL, Berger TG. Medical school dermatology curriculum: Are we adequately preparing primary care physicians? J Am Acad Dermatol 2009;61:23-90.
[Google Scholar]
|
| 5. |
Kar S, Ahmad S, Pal R. Current knowledge attitudes, and practices of healthcare providers about leprosy in Assam, India. J Glob Infect Dis 2010;2:212-5.
[Google Scholar]
|
| 6. |
Regulations on Graduate Medical Education. New Delhi: Medical Council of India; 1997. Available from: https://www.old.mciindia.org/Rules-and-Regulation/GME_REGULATIONS.pdf. [Last accessed on 2018 May 27].
[Google Scholar]
|
| 7. |
Schofield JK, Fleming D, Grindlay D, Williams H. Skin conditions are the commonest new reason people present to general practitioners in England and Wales. Br J Dermatol 2011;165:1044-50.
[Google Scholar]
|
| 8. |
Whiting G, Magin P, Morgan S, Tapley A, Henderson K, Oldmeadow C, et al. General practice trainees' clinical experience of dermatology indicates a need for improved education: A cross-sectional analysis from the Registrar Clinical Encounters in Training Study. Australas J Dermatol 2017;58:e199-206.
[Google Scholar]
|
| 9. |
Lam TP, Yeung CK, Lam KF. What are the learning outcomes of a short postgraduate training course in dermatology for primary care doctors? BMC Med Educ 2011;11:20.
[Google Scholar]
|
| 10. |
Al-Zahrani M, Nahar S, Al-Zahrani S, Al-Zahrni R. Knowledge, attitude, and practice of primary care physicians regarding common dermatological disorders in Abha City, Kingdom of Saudi Arabia. IOSR J Pharm 2017;7:89-110.
[Google Scholar]
|
| 11. |
Mahé A, Faye O, N'Diaye HT, Konaré HD, Coulibaly I, Kéita S, et al. Integration of basic dermatological care into primary health care services in Mali. Bull World Health Organ 2005;83:935-41.
[Google Scholar]
|
| 12. |
Shaffer MP, Feldman SR, Fleischer AB Jr. Use of clotrimazole/betamethasone diproprionate by family physicians. Fam Med 2000;32:561-5.
[Google Scholar]
|
| 13. |
Bahelah S, Bahelah R, Bahelah M, Albatineh A, Schumacher U. Primary care physicians' knowledge and self-perception of competency in dermatology: An evaluation study from Yemen. Cogent Med 2015;2:1119948.
[Google Scholar]
|
| 14. |
Evans AW, McKenna C, Oliver M. Self-assessment in medical practice. J R Soc Med 2002;95:511-3.
[Google Scholar]
|
| 15. |
Kirsner RS, Federman DG. Lack of correlation between internists' ability in dermatology and their patterns of treating patients with skin disease. Arch Dermatol 1996;132:1043-6.
[Google Scholar]
|
| 16. |
Kerr OA, Walker J, Boohan M. General practitioners' opinions regarding the need for training in dermatology at undergraduate and postgraduate levels. Clin Exp Dermatol 2006;31:132-3.
[Google Scholar]
|
| 17. |
Vallikunnu V, Kumar SG, Sarkar S, Kar SS, Harichandrakumar KT. A qualitative study on working experience of rural doctors in Malappuram district of Kerala, India. J Family Med Prim Care 2014;3:141-5.
[Google Scholar]
|
| 18. |
Harlow ED, Burton JL. What do general practitioners want from a dermatology department? Br J Dermatol 1996;134:313-8.
[Google Scholar]
|
Fulltext Views
4,154
PDF downloads
1,880





