Translate this page into:
Nevus sebaceus on the face: Experience with photodynamic therapy in adults and children
Correspondence Address:
Oscar Mu�oz Moreno-Arrones
Ramón y Cajal University Hospital, Ctra, De Colmenar Viejo, Km. 9100, 28034 Madrid
Spain
| How to cite this article: Moreno-Arrones OM, Perez-Garcia B. Nevus sebaceus on the face: Experience with photodynamic therapy in adults and children. Indian J Dermatol Venereol Leprol 2019;85:440 |
Sir,
Nevus sebaceus is a rare hamartoma of the skin that can grow and thicken during puberty and in some cases undergo malignant transformation. It has been linked to somatic mosaic mutations in either the KRAS (Kirsten Rat Sarcoma Viral Oncogene Homolog) or HRAS (Harvey Rat Sarcoma Viral Oncogene Homolog) genes. Sebaceous nevi typically present as yellow-orange oval or linear well-defined plaques affecting predominantly the scalp. Unfortunately, sebaceous nevi also have a tendency to appear on the face leading to patients experiencing low self-esteem due to esthetic considerations. Although risk of malignancy is the main reason for removal of these lesions, incidence of malignant transformation has not been established yet and remains a topic of controversy.[1],[2] Nevertheless, sebaceous nevi may also require treatment to improve esthetics. Despite the fact that complete excision of the lesion is curative, it may leave disfiguring scars. For this reason, other therapeutic approaches such as photodynamic therapy, carbon dioxide laser or dermabrasion have been proposed with mixed results.[3],[4],[5] A previous report studied the efficacy and safety of photodynamic therapy on 12 sebaceous nevi with promising results (58% patients showed moderate improvement, 25% showed mild improvement and 17% had a marked improvement).[5] However, before each photodynamic therapy session, the authors performed carbon dioxide laser ablation on the lesions. As some patients received numerous photodynamic therapy and carbon dioxide laser sessions, it may be incorrect to conclude that the efficacy of the treatment was solely due to photodynamic therapy.
This study describes the clinical outcome and adverse effects of photodynamic therapy applied to sebaceous nevi affecting esthetically concerning areas such as the eyelids or the face. The rationale behind using photodynamic therapy for sebaceous nevi is the selectivity of methyl aminolevulinate for the sebaceous glands. This fact is further evidenced by observing the greater fluorescence of these lesions in relation to the surrounding healthy skin after the application of the photosensitizer [Figure - 1].
 |
| Figure 1: Nevus sebaceus on the left cheek. Clinical and ultraviolet pictures of the lesion and results after the last photodynamic therapy session. Note the decrease in fluorescence due to the improvement of the nevus sebaceous |
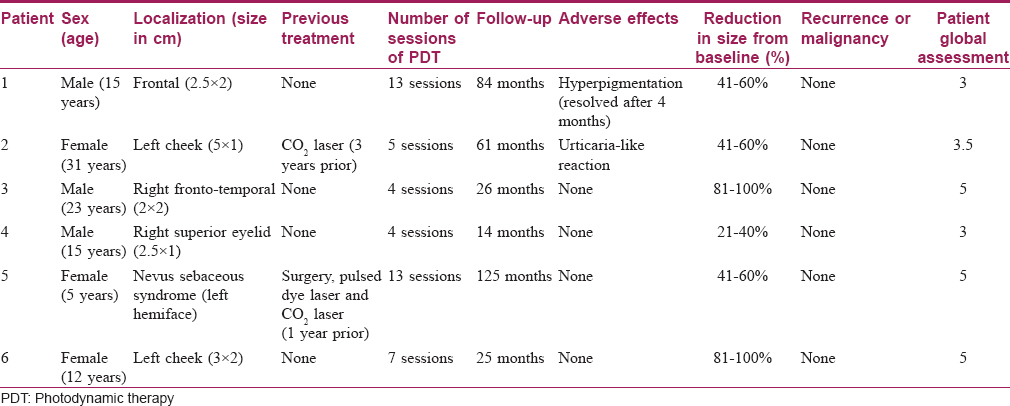
A retrospective descriptive study of six patients with sebaceous nevi on the face treated with photodynamic therapy was conducted at our hospital. A dermatologist not involved in the study visually assessed clinical improvement. Efficacy was evaluated at the end of the treatment. In addition, patients subjectively evaluated the treatment based on pain during procedure, esthetic outcome and treatment duration. This was graded from 0 (“awful treatment”) to 5 (“excellent treatment”).
Procedure consisted of the application of a photosensitizer, topical methyl aminolevulinate (Metvix®, Galderma, France), to the lesions, followed by occlusion with a polyurethane film. Incubation time was 3 h. Total light dose was 37 J/cm2. Depending on post-treatment inflammation and high fluorescence, incubation time was reduced in the following sessions to 2 h. After incubation, the lesions were irradiated with a 630 nm light emitting diode device without anesthesia.
Time between each photodynamic therapy session was 3 weeks. Treatment was stopped when either the patient was satisfied with the clinical result or demanded surgical removal of the lesion.
[Table - 1] summarizes the results of the study. Mean age of patients was 16.8 years (range 5–31). Two patients had received laser treatment in the past. Five patients (83.3%) achieved significant improvement (at least a 50% reduction in size) at the end of their treatment [Figure - 1], two of them experienced more than 80% reduction in size compared to baseline. The patient with sebaceous nevi affecting the eyelid experienced only minor improvement (30% reduction in size). Mean score for patient's satisfaction was 4.08 (range 3–5). Mean number of sessions per patient was 7.6 (4–13). Adverse events were rare and transient: One patient experienced an urticaria-like reaction and other suffered temporary hyperpigmentation. Neither recurrence nor malignant transformation was observed during the follow-up (14–125 months, mean 55.8). All the patients tolerated the treatment well. It is interesting to highlight that the patients that achieved significant improvement did so after at least three sessions. Only one patient demanded surgical removal of the lesion.
This study shows that photodynamic therapy offers good clinical response with a low risk of adverse events and could be considered as an adjuvant or alternative therapy in sebaceous nevi affecting esthetically concerning areas. Main limitations of this study were the low number of patients involved, the absence of a control group or comparison between topical photosensitizers, different intensities of light and other treatments. Better-designed controlled studies are needed to characterize optimal therapeutic approach for these cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rosen H, Schmidt B, Lam HP, Meara JG, Labow BI. Management of nevus sebaceous and the risk of basal cell carcinoma: An 18-year review. Pediatr Dermatol 2009;26:676-81.
[Google Scholar]
|
| 2. |
Moody MN, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol 2012;29:15-23.
[Google Scholar]
|
| 3. |
Kim HS, Jun JH, Lee JY. Photodynamic therapy of facial nevus sebaceous. Photodermatol Photoimmunol Photomed 2010;26:98-100.
[Google Scholar]
|
| 4. |
Calzavara-Pinton PG, Rossi MT, Sala R; Italian Group for Photodynamic Therapy. A retrospective analysis of real-life practice of off-label photodynamic therapy using methyl aminolevulinate (MAL-PDT) in 20 Italian dermatology departments. Part 2: Oncologic and infectious indications. Photochem Photobiol Sci 2013;12:158-65.
[Google Scholar]
|
| 5. |
In SI, Lee JY, Kim YC. Topical photodynamic therapy for nevus sebaceous on the face. Eur J Dermatol 2010;20:590-2.
[Google Scholar]
|
Fulltext Views
3,481
PDF downloads
1,704





