Translate this page into:
Oral isotretinoin for treating mucocutaneous human papillomavirus infections: A systematic review and meta-analysis
2 Department of Dermatology, School of Medicine, College of Medicine, Taipei Medical University; Department of Dermatology, Taipei Medical University Hospital, Taipei, Taiwan
Correspondence Address:
Yu-Chen Huang
Department of Dermatology, Wan Fang Hospital, Taipei Medical University, 111, Hsing-Long Road Sec. 3, Wenshan District, Taipei City 116
Taiwan
| How to cite this article: Yang TH, Lee TH, Huang YC. Oral isotretinoin for treating mucocutaneous human papillomavirus infections: A systematic review and meta-analysis. Indian J Dermatol Venereol Leprol 2019;85:569-577 |
Abstract
Introduction: Some viral warts are refractory to treatment, some others tend to recur. Oral isotretinoin is useful against warts to varying degrees.
Objective: To determine the efficacy of oral isotretinoin for treating mucocutaneous human papillomavirus infections.
Methods: A systematic review and meta-analysis of studies published from the date of inception of the databases to December 30, 2017 were conducted. Randomized controlled trials or case series with ≥10 patients with mucocutaneous human papillomavirus infection who had received oral isotretinoin treatment were analyzed. The meta-analysis estimated the pooled odds ratio and pooled response rate.
Results: The review included eight studies. Trials of oral isotretinoin versus placebo treatment revealed that isotretinoin effectively treated mucocutaneous human papillomavirus infections (odds ratio: 43.8, 95% confidence interval: 9.7–198.8). The pooled estimate of the complete response rate of oral isotretinoin to mucocutaneous human papillomavirus was 67.7% (95% confidence interval: 49.5–81.7%). Another pooled estimation revealed that 83.9% (95% confidence interval: 59.7–94.9%) of patients exhibited at least 50% lesion clearance, whereas 12.3% with complete response experienced recurrence.
Limitations: This meta-analysis had a small sample size and high inter-study heterogeneity.
Conclusion: Oral isotretinoin is superior to placebo for treating mucocutaneous human papillomavirus infections, particularly plane warts. The recurrence rate and risk of severe side effects are low.
Introduction
Treatment of mucocutaneous human papillomavirus infections, or warts, can be extremely challenging, particularly in adult patients with relatively long disease duration and extensive distribution.[1] The most common first-line treatments for warts are topical salicylic acid and cryotherapy.[1] A recent meta-analysis indicated that salicylic acid has only a moderate therapeutic effect on nongenital warts, and trials comparing cryotherapy with placebo treatment have revealed no significant differences between the effectiveness of cryotherapy and that of placebo.[2] High-quality evidence for other treatment modalities such as topical caustic and antimitotic substances, intralesional bleomycin injections, surgical excision, or curettage and cautery is currently not available. None of these modalities appear safer or more effective than salicylic acid or cryotherapy.[2],[3],[4],[5] Hence, despite the therapeutic armamentarium available, some mucocutaneous human papillomavirus infections remain refractory to multiple treatments.
Oral retinoids were first used by Gelmetti et al.[6] in 1987 to treat various types of refractory cutaneous warts, and used by Olsen et al.[7] in 1989 to treat refractory genital warts. Subsequently, other researchers have reported treating mucocutaneous human papillomavirus infections with varying doses of isotretinoin and have achieved varying rates of complete clearance.[8],[9],[10],[11],[12],[13],[14] Theoretically, oral retinoids can affect epidermal growth and differentiation,[15] induce immunomodulation and downregulate human papillomavirus expression in infected cells,[16],[17] and thus appear to be a promising therapeutic choice. However, this modality has seldom been mentioned in the numerous treatment guidelines for warts because only a few studies with small sample sizes have reported the use of oral isotretinoin.[1],[5],[18],[19] The efficacy of oral isotretinoin for treating mucocutaneous human papillomavirus infections, as well as the optimal dose, ideal treatment durations, recurrence rates and safety profiles still require clarification. Our meta-analysis was conducted to determine current evidence for the efficacy of oral isotretinoin in treating mucocutaneous human papillomavirus infections.
Methods
A systematic review and meta-analysis were conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (http://www.prisma-statement.org/).
Data source and search strategy
We identified studies indexed in the PubMed, MEDLINE, Embase and Cochrane Library databases from the date of inception of the databases to December 30, 2017. The search parameters included the terms “wart,” “verruca” and “condyloma” combined with “isotretinoin,” “oral retinoid” and “systemic retinoid.” References within the search results (articles) were also reviewed to identify additional studies available.
Eligibility criteria and study selection
We analyzed randomized controlled trials where oral isotretinoin alone was used in one of the study arms, as well as a case series with ≥10 patients who had received oral isotretinoin for treating warts. Studies that used oral retinoids other than isotretinoin or in combination with other treatment modalities, with treatment durations of <6 weeks, and those that included participants with epidermodysplasia verruciformis or immunocompromise were excluded. Review articles, conference reports and case reports were also excluded. Two authors of the present study (Dr. YCH and Dr. THY) independently screened all article titles and abstracts. The full texts of relevant studies were accessed to determine their eligibility. Any disagreement was resolved by reaching a consensus.
Quality assessment
We adapted the methodological assessment tool known as “MINORS” from the studies of Slim et al. for the critical appraisal of studies on interventions.[20] The tool comprises 12 items graded on three-point scales (0–2) for controlled studies and eight items for case series. Two authors of the present study (Dr. YCH and Dr. THY) independently assessed the quality of the analyzed studies. In the case of a discrepancy, a third reviewer (Dr. THL) made the final decision.
Outcomes
The primary outcomes of the present study were the complete response rate to oral isotretinoin, defined as total clearance of lesions, and the partial response rate to oral isotretinoin, defined as lesion reduction in number or size by ≥50%. The secondary outcomes were severe adverse effects that required discontinuation of treatment and the recurrence rate defined as disease relapse after total clearance of skin lesions.
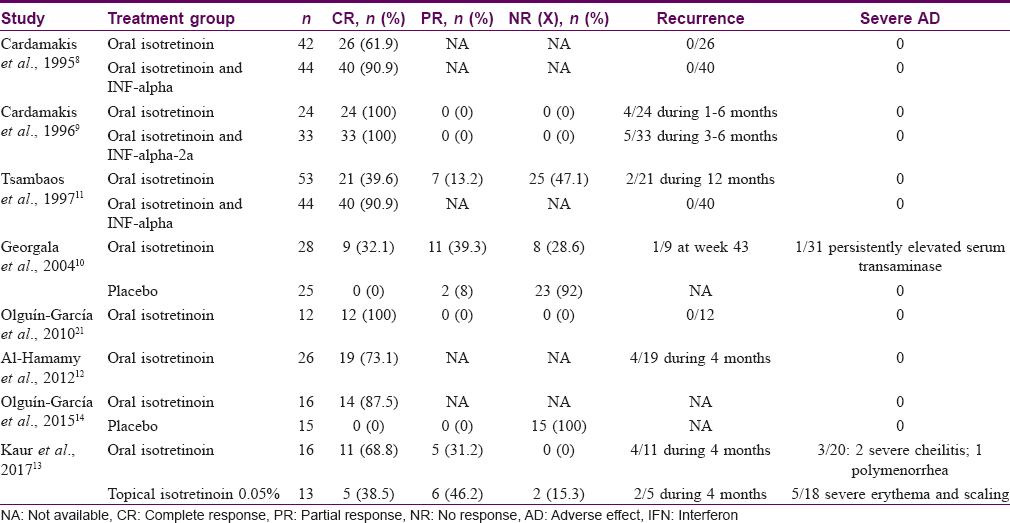
Data extraction
Data were independently extracted by two authors (Dr. YCH and Dr. THY). Any disagreement was resolved by reaching a consensus. Data on the following measures were extracted: study country, sample size, type of human papillomavirus infection, dosage and duration of medication, follow-up time and quality scores [Table - 1]. In addition, data on the complete response rate, partial response rate, recurrence rate and number of severe side effects requiring discontinuation of therapy were extracted [Table - 2]. In this meta-analysis, the patients who had received 0.5 and 1 mg/kg/day of isotretinoin were categorized into low- and high-dose groups respectively.

Data analysis
For the analyzed randomized controlled trials, we produced a pooled estimate of the complete response rate of patients treated with oral isotretinoin compared with that of the control group, if two or more studies categorized within the same control groups. The results are expressed as overall odds ratios with associated 95% confidence intervals. Randomized controlled trials that used oral isotretinoin for treatment were included as case series with data pooled from other case series to create a single-arm study for data analysis. We produced a pooled estimate of the complete response rate, as well as the combined complete response and partial response rate (corresponding to patients with ≥50% lesion reduction) of patients with mucocutaneous human papillomavirus infections. Subsequently, based on dosage and type of human papillomavirus infections, data were stratified into the following groups: (1) high- and low-dose; (2) condyloma acuminatum and plane warts. If two or more similar studies were categorized within the same group, separate pooled estimates of the complete response rate in each group were calculated using proportions (%). Homogeneity testing was conducted using the I[2] test, and a fixed-effects model was used if there was a lack of heterogeneity. If I[2] was> 50%, a random-effect model was used.[22] Publication bias was tested during the analysis of the response rates of all studies by using the Begg and Mazumdar test. Analyses were all performed using comprehensive meta-analysis version 3 (Biostat, Inc., Englewood, NJ, USA).
Results
Search results and trial characteristics
Of the 319 studies screened (by abstract), eight comprised a total of 217 patients with mucocutaneous human papillomavirus infections who had received oral isotretinoin treatment, thereby meeting the inclusion criteria [Figure - 1]. A summary of the characteristics of the included studies is provided in [Table - 1]. The eight eligible studies consisted of five randomized controlled trials and three case series. Except for those in one study, the patients in all analyzed studies were refractory to at least one of the treatment modalities for mucocutaneous human papillomavirus infections, and the disease durations of these patients varied from 3 months to 5 years before treatment.[13] Only two studies had conducted direct head-to-head comparisons of oral-isotretinoin-treated and placebo-treated groups.[10],[14] The quality scores of case series and randomized controlled trials were 9–14 and 19–21, respectively. The common factors that adversely affected the quality scores were the absence of a double-blind evaluation and loss to follow-up exceeding 5%.
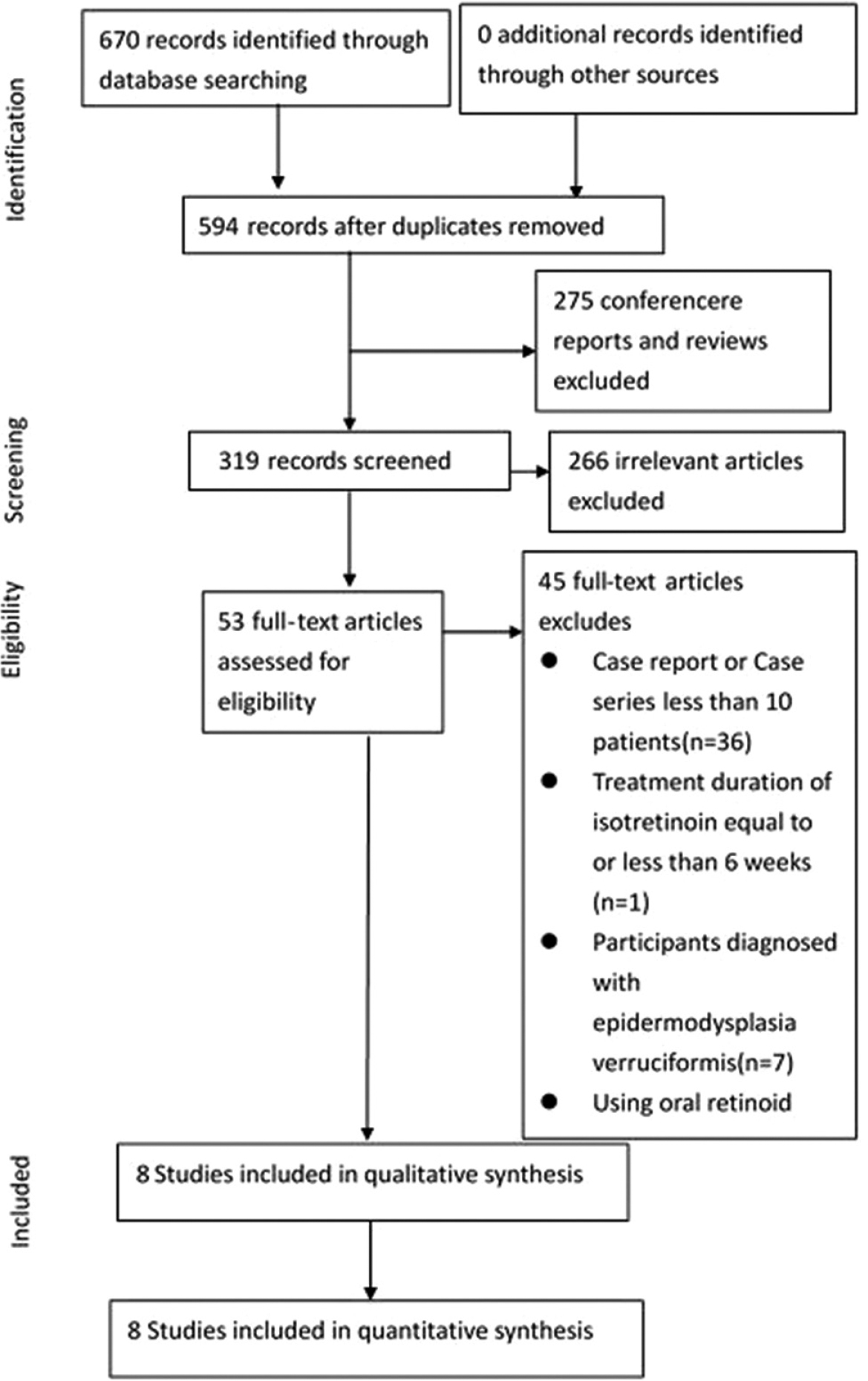 |
| Figure 1: Flowchart: Selection of studies included in the present systematic review and meta-analysis |
Complete response rate with oral isotretinoin versus placebo treatment
Two randomized controlled trials were available for evaluation. The patients analyzed had been diagnosed to have facial plane warts [14] or condyloma acuminatum of the cervix.[10] The complete response rate in the treatment group was significantly higher than that in the placebo group (odds ratio 43.1; 95% confidence interval, 9.9–186.8; I[2] = 3) [Figure - 2] and [Table - 3].
 |
| Figure 2: Comparison of the complete response rate between oral isotretinoin and placebo group. Pooled analysis of odds ratio and 95% confidence intervals. Two randomized controlled trials were available. Overall, odds ratio was 43.8 (95% confidence interval: 9.7–198.8%) |

Complete response rate with oral isotretinoin
The complete response rate with oral isotretinoin was 62.6% (136/217). A pooled estimation of the complete response rate was based on the eight studies that provided relevant data of 217 patients.[8],[9],[10],[11],[12],[13],[14],[21] The pooled complete response rate was 67.7% (95% CI: 49.5–81.7%) in all patients with mucocutaneous human papillomavirus infections [Figure - 3]a and [Table - 3]. Publication bias was noted (P = 0.019) in the estimation of pooled complete response rate [Figure - 3]b.
 |
| Figure 3: |
Combined complete response and partial response rate with oral isotretinoin
The combined complete response and partial response rate with oral isotretinoin was 75.1% (100/133). A pooled estimation of the combined complete response and partial response rate was based on five studies that provided relevant data.[9],[10],[11],[13],[21] The pooled combined complete response and partial response rate to oral retinoids was 83.9% [95% CI: 59.7–94.9%; [Figure - 4]a and [Table - 3]. A funnel plot did not reveal publication bias (P = 0.462) [Figure - 4]b.
 |
| Figure 4: |
Complete response rate of condyloma acuminatum
Four studies comprising 147 patients were available for the pooled estimation of the complete response rate with oral isotretinoin in patients with refractory condyloma acuminatum.[8],[9],[10],[11] The pooled complete response rate was 64.9% [95% CI: 41.7–82.7%; [Table - 3].
Complete response rate of plane warts
Four studies comprising 70 patients were available for the pooled estimation of the complete response rate with oral isotretinoin in patients with cutaneous human papillomavirus infections other than condyloma acuminatum.[12],[13],[14],[21] All patients in these four studies had extensive plane warts. In three of these four studies, the warts were on the patients' faces. The pooled complete response rate was 76.6% [95% CI: 64.3–85.6%; [Table - 3].
Rate of complete response to high-dose oral isotretinoin
A pooled estimation of rate of complete response to high-dose oral isotretinoin was based on three studies comprising 119 patients, where all patients had received diagnoses of condyloma acuminatum.[8],[9],[11] The treatment duration was 3 months for all patients. The pooled complete response rate was 63.7% [95% CI: 33.7–85.8%; [Table - 3].
Rate of complete response to low-dose oral isotretinoin
A pooled estimation of rate of complete response to low-dose isotretinoin was based on five studies comprising 98 patients.[10],[12],[13],[14],[21] All patients had been diagnosed with condyloma acuminatum of the cervix in one study and with plane warts in the other four studies.[10] The treatment duration was 3 months for all patients. The pooled complete response rate was 71.6% [95% CI: 45.1–88.5%; [Table - 3].
Discontinuation because of severe adverse effects
Of all the patients analyzed, only four discontinued oral retinoid treatment because of severe adverse effects. Two patients had severe cheilitis,[13] one had polymenorrhea [13] and one had persistently elevated serum transaminase.[10] All four had been treated with low-dose isotretinoin (0.5 mg/kg/day).
Recurrence rate
The follow-up timeframe was documented in all but one case series.[14] The follow-up period ranged from 3 to 20 months. Among all patients who exhibited complete response to oral isotretinoin (n = 122), 15 exhibited disease recurrence. Of 11 patients with plane warts, four had disease recurrence within a 4-month follow-up period.[13] Of nine patients one with cervical condyloma acuminatum had a recurrence at 43 weeks.[10] In four of 24 patients with condyloma acuminatum, disease recurrence was observed after 1–6 months of follow-up. 9 Of 19 patients with plane warts, four exhibited relapse during a 4-month follow-up period.[12] Of 21 patients with condyloma acuminatum, two had recurrence during a 12-month follow-up period.[11] The total recurrence rate of all mucocutaneous human papillomavirus infections after a complete response to oral retinoids was 12.3%.
Discussion
Our meta-analysis results revealed that oral isotretinoin is superior to placebo for treating refractory mucocutaneous human papillomavirus infections. Because the two studies analyzed in the meta-analysis evidently verified the superiority of isotretinoin treatment over placebo treatment, a substantial response rate was crucial.[10],[14] The overall pooled complete response rate and combined complete response and partial response rate were 67.7 and 83.9% respectively. When evaluating the response rate of any treatment modality for warts, the possibility of spontaneous resolution should be considered. Notably, most of the patients included in the analyzed studies had exhibited long durations of human papillomavirus infections and had failed to respond to at least one treatment modality. Previous studies have shown that warts that have persisted for long durations in adults are less likely to spontaneously resolve and are more refractory to treatment.[1],[23] Hence our study results were less likely to be influenced by the effect of spontaneous remission.
The pooled rates of complete response to oral isotretinoin in patients with condyloma acuminatum and those with plane warts were 64.9 and 76.6% respectively. These data suggest that plane warts, a troublesome condition for clinicians and patients, respond favorably to oral isotretinoin. The differences in the response rates of various types of human papillomavirus infections remain to be elucidated. Plane warts tend to be distributed extensively on the face, causing significant cosmetic disfigurement and psychological stress in patients. First-line treatments, including cryotherapy and topical trichloroacetic acid, may exacerbate cosmetic problems due to post-inflammatory hyperpigmentation and scarring. Further, the response rate and treatment duration are highly variable.[24] Our study results indicate that oral isotretinoin is a promising therapeutic choice in terms of response rate and cosmetic concerns for patients with refractory facial plane warts.
In our study, the pooled complete response rates to high-dose and low-dose isotretinoin were 63.7 and 71.6%, respectively. No head-to-head comparison was available for review in the literature. However, these data likely show that high-dose isotretinoin (1 mg/kg/day) is not more advantageous than low-dose isotretinoin (0.5 mg/kg/day) for treating mucocutaneous human papillomavirus infections.
Treatment duration is also worth noting. The shortest recorded response duration among the analyzed studies was 8 weeks.[13] Most patients in our meta-analysis had received a full treatment course of 3 months. Olsen et al. reported that all patients with condyloma acuminatum failed to respond to high-dose oral isotretinoin alone over a 6-week treatment period.[7] Other researchers have suggested that 6 weeks may not be a sufficiently long duration for isotretinoin treatment alone and a longer duration of treatment with this retinoid might improve therapeutic responses in patients.[11] Furthermore, Kaur et al. noted that relapse was more frequently observed in patients for whom treatment was stopped earlier because of early clearance.[13] Thus, extending treatment over a longer duration may reduce the risk of relapse. We believe that a treatment course of low-dose isotretinoin for 3 months is reasonable, whereas a treatment duration <8 weeks may be insufficient for inducing a response.
Although side effects of oral isotretinoin such as cheilitis, dry skin and dry eyes were commonly observed among the patients, they were manageable in most patients.[7],[8],[9],[10],[11],[12],[13],[14] Among the 217 patients who had received high- or low-dose oral retinoids, only four had discontinued treatment because of adverse side effects (number need to harm = 54.25). Notably, none of these four patients had received high-dose isotretinoin.
This study had some limitations. The meta-analysis had a small sample size and only a few studies were analyzed. Publication bias was noted in the estimation of pooled complete response rate. In addition, the pooled studies included patients with different types of human papillomavirus infections, treatment doses, sampling approaches and sample sizes. Moreover, the patients belonged to various regional and ethnic backgrounds. Publication bias might come from the inter-study variation. To address these potential differences, wherever possible, we stratified models according to dosage (high- or low-dose) and type of human papillomavirus infection (condyloma acuminatum or plane warts). No publication bias was noted in these subgroup analyses. However, considerable heterogeneity still existed in each subgroup. Nevertheless, because of a dearth of related trials, this was the best measure we could adopt to prevent biases. Larger randomized controlled trials are warranted.
Conclusion
Patients with mucocutaneous human papillomavirus infections treated using isotretinoin exhibited a higher complete response rate than did those treated with placebo. Patients with refractory mucocutaneous human papillomavirus infections responded favorably to oral isotretinoin, particularly those with plane warts, who exhibited a 76.6% complete response rate. High-dose isotretinoin (1 mg/kg/day) does not appear to be more advantageous than low-dose isotretinoin (0.5 mg/kg/day) for treating human papillomavirus infections. The recurrence rate was low and severe adverse effects occurred infrequently.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sterling JC, Handfield-Jones S, Hudson PM; British Association of Dermatologists. Guidelines for the management of cutaneous warts. Br J Dermatol 2001;144:4-11.
[Google Scholar]
|
| 2. |
Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev 2012;CD001781.
[Google Scholar]
|
| 3. |
Gibbs S, Harvey I. Topical treatments for cutaneous warts. Cochrane Database Syst Rev 2006;CD001781.
[Google Scholar]
|
| 4. |
Kwok CS, Holland R, Gibbs S. Efficacy of topical treatments for cutaneous warts: A meta-analysis and pooled analysis of randomized controlled trials. Br J Dermatol 2011;165:233-46.
[Google Scholar]
|
| 5. |
Lipke MM. An armamentarium of wart treatments. Clin Med Res 2006;4:273-93.
[Google Scholar]
|
| 6. |
Gelmetti C, Cerri D, Schiuma AA, Menni S. Treatment of extensive warts with etretinate: A clinical trial in 20 children. Pediatr Dermatol 1987;4:254-8.
[Google Scholar]
|
| 7. |
Olsen EA, Kelly FF, Vollmer RT, Buddin DA, Weck PK. Comparative study of systemic interferon alfa-nl and isotretinoin in the treatment of resistant condylomata acuminata. J Am Acad Dermatol 1989;20:1023-30.
[Google Scholar]
|
| 8. |
Cardamakis E, Kotoulas IG, Relakis K, Metalinos K, Michopoulos J, Stathopoulos E, et al. Comparative study of systemic interferon alfa-2a plus isotretinoin versus isotretinoin in the treatment of recurrent condyloma acuminatum in men. Urology 1995;45:857-60.
[Google Scholar]
|
| 9. |
Cardamakis EK, Kotoulas IG, Dimopoulos DP, Stathopoulos EN, Michopoulos JT, Tzingounis VA. Comparative study of systemic interferon alfa-2a with oral isotretinoin and oral isotretinoin alone in the treatment of recurrent condylomata accuminata. Arch Gynecol Obstet 1996;258:35-41.
[Google Scholar]
|
| 10. |
Georgala S, Katoulis AC, Georgala C, Bozi E, Mortakis A. Oral isotretinoin in the treatment of recalcitrant condylomata acuminata of the cervix: A randomised placebo controlled trial. Sex Transm Infect 2004;80:216-8.
[Google Scholar]
|
| 11. |
Tsambaos D, Georgiou S, Monastirli A, Sakkis T, Sagriotis A, Goerz G. Treatment of condylomata acuminata with oral isotretinoin. J Urol 1997;158:1810-2.
[Google Scholar]
|
| 12. |
Al-Hamamy HR, Salman HA, Abdulsattar NA. Treatment of plane warts with a low-dose oral isotretinoin. ISRN Dermatol 2012;2012:163929.
[Google Scholar]
|
| 13. |
Kaur GJ, Brar BK, Kumar S, Brar SK, Singh B. Evaluation of the efficacy and safety of oral isotretinoin versus topical isotretinoin in the treatment of plane warts: A randomized open trial. Int J Dermatol 2017;56:1352-8.
[Google Scholar]
|
| 14. |
Olguín-García MG, Jurado-Santa Cruz F, Peralta-Pedrero ML, Morales-Sánchez MA. A double-blind, randomized, placebo-controlled trial of oral isotretinoin in the treatment of recalcitrant facial flat warts. J Dermatolog Treat 2015;26:78-82.
[Google Scholar]
|
| 15. |
Jason J, Archibald LK, Nwanyanwu OC, Sowell AL, Buchanan I, Larned J, et al. Vitamin A levels and immunity in humans. Clin Diagn Lab Immunol 2002;9:616-21.
[Google Scholar]
|
| 16. |
Bartsch D, Boye B, Baust C, zur Hausen H, Schwarz E. Retinoic acid-mediated repression of human papillomavirus 18 transcription and different ligand regulation of the retinoic acid receptor beta gene in non-tumorigenic and tumorigenic HeLa hybrid cells. EMBO J 1992;11:2283-91.
[Google Scholar]
|
| 17. |
Faluhelyi Z, Rodler I, Csejtey A, Tyring SK, Ember IA, Arany I. All-trans retinoic acid (ATRA) suppresses transcription of human papillomavirus type 16 (HPV16) in a dose-dependent manner. Anticancer Res 2004;24:807-9.
[Google Scholar]
|
| 18. |
Drake LA, Ceilley RI, Cornelison RL, Dobes WL, Dorner W, Goltz RW, et al. Guidelines of care for warts: Human papillomavirus. Committee on guidelines of care. J Am Acad Dermatol 1995;32:98-103.
[Google Scholar]
|
| 19. |
Micali G, Dall'Oglio F, Nasca MR, Tedeschi A. Management of cutaneous warts: An evidence-based approach. Am J Clin Dermatol 2004;5:311-7.
[Google Scholar]
|
| 20. |
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J Surg 2003;73:712-6.
[Google Scholar]
|
| 21. |
Olguín-García MG, Cancela RG, Peralta-Pedrero ML. Estudio preexperimental para el tratamiento de verrugas planas faciales con isotretinoı'na oral. Dermatol Rev Mex 2010;54:267-72.
[Google Scholar]
|
| 22. |
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60.
[Google Scholar]
|
| 23. |
Bunney MH, Nolan MW, Williams DA. An assessment of methods of treating viral warts by comparative treatment trials based on a standard design. Br J Dermatol 1976;94:667-79.
[Google Scholar]
|
| 24. |
Stulberg DL, Hutchinson AG. Molluscum contagiosum and warts. Am Fam Physician 2003;67:1233-40.
[Google Scholar]
|
Fulltext Views
12,663
PDF downloads
3,055





