Translate this page into:
Co-occurrence of lichen striatus in twins
Correspondence Address:
Tapaswini Tripathy
Department of Dermatology, IMS and SUM Hospital, Bhubaneswar, Odisha
India
| How to cite this article: Tripathy T, Singh BS, Kar BR. Co-occurrence of lichen striatus in twins. Indian J Dermatol Venereol Leprol 2019;85:632-634 |
Sir,
Lichen striatus is a self-limiting inflammatory dermatosis commonly affecting children between 4 months and 15 years of age. It manifests in the form of pinkish to reddish flat topped closely set papules usually in a characteristic blaschkoid pattern. The exact etiology is not known. There are few reports of lichen striatus in siblings sharing a common environment suggesting a possible role of infectious agent.[1],[2] Herein, we report a case of co-occurrence of lichen striatus in twins.
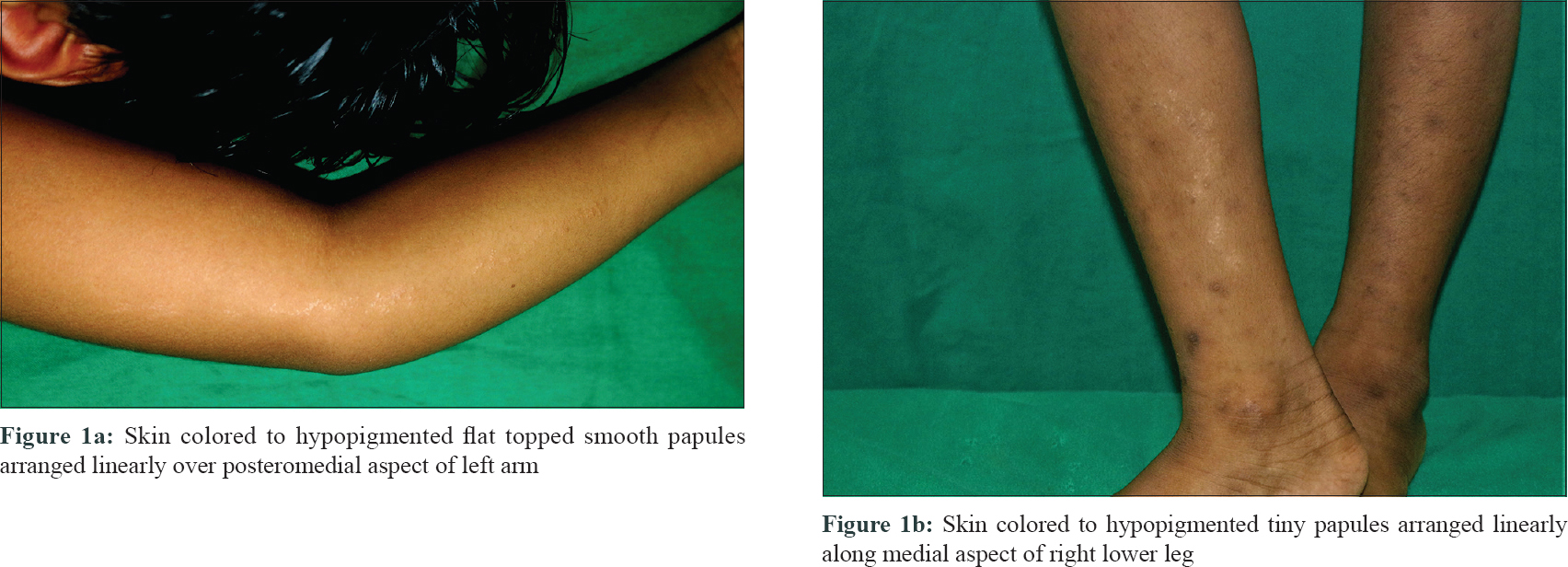
A 6-year-old, girl child born out of non-consanguineous marriage presented to the dermatology department of IMS and SUM Hospital, Bhubaneswar, with asymptomatic skin lesions in a linear distribution over the left arm for 6 months. On examination, there were skin colored to hypopigmented flat topped smooth papules arranged linearly over posteromedial aspect of the left arm [Figure - 1]a. The rest of the body, scalp, nails, and mucosae were normal. Systemic examination revealed no abnormality.
 |
| Figure 1: |
The twin sister of case 1 presented with similar skin colored to hypopigmented tiny papules arranged linearly along the medial aspect of the right lower leg without any surface change [Figure - 1]b. Lesions had started appearing approximately 1 week after case 1. The rest of body, scalp, nails and mucosa were unaffected. Systemic examination was within normal limit.
In both the cases, there was no history of preceding upper or lower respiratory tract infection or any other major illness. They also denied any vaccination prior to the episode. There was no personal or family history of atopy.
Histopathology study of punch biopsy specimen of both the cases showed parakeratosis and lichenoid infiltrate in the upper dermis with minimal spongiosis [Figure - 2]. On immunohistochemistry, the lichenoid infiltrates were predominantly composed of CD8+ T lymphocytes [Figure - 3]. Based on classical morphology and biopsy findings, a diagnosis of lichen striatus was made. Both the cases were treated with topical tacrolimus 0.03% ointment and lesions improved over the next 2 months with post inflammatory hypopigmentation.
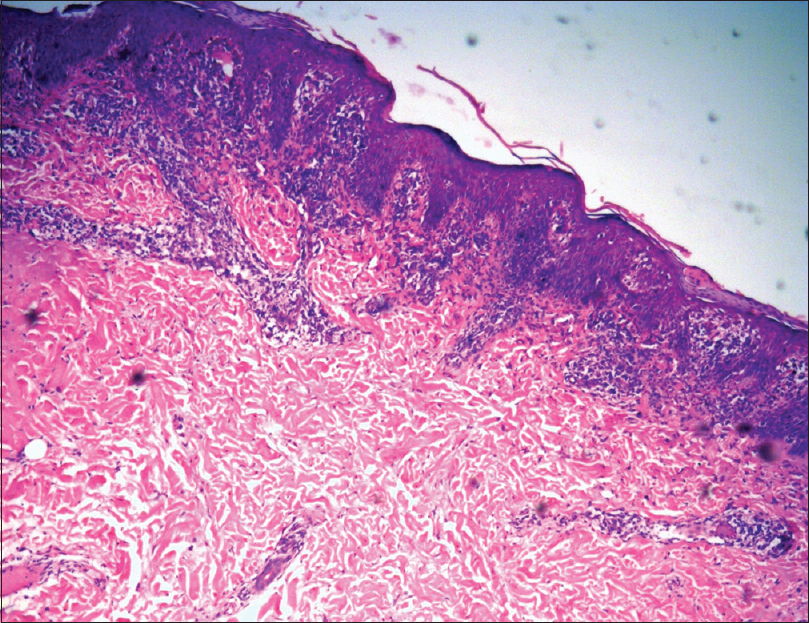 |
| Figure 2: Focal lichenoid infiltrate in the upper dermis with minimal spongiosis (H and E, ×100) |
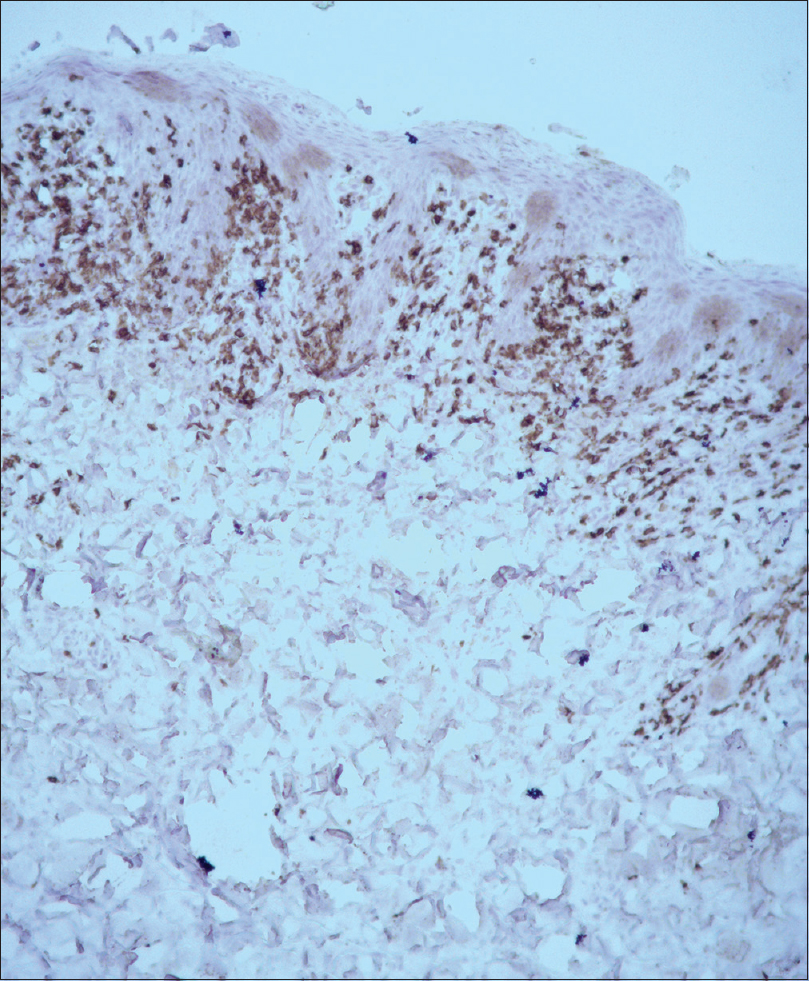 |
| Figure 3: Immunohistochemistry shows positivity for CD8+ T lymphocytes (×100) |
The etiopathogenesis of lichen striatus is incompletely understood. Due to its characteristic blaschkoid distribution, cutaneous mosaicism during embryonic period is implicated in its pathogenesis. Genetic mosaicism is a condition where two or more different genotypes exist in a zygote, usually due to somatic mutation occurring during embryonic period. Ultraviolet radiation, viral infection, environmental genotoxic agents, and errors during DNA replication are suggested as possible triggers for somatic mutation. The phenotypically distinct mutant clones give rise to lesions in patterns determined by the affected cell type. In lichen striatus, mutated keratinocytes derived from limited number of precursors produce visible abnormal growth. Although the mutations are present at birth, the mutated clones remain suppressed by immune tolerance mechanism of the body. Some acquired events like infection or environmental stress cause loss of immune tolerance, allowing the aberrant clones to express the neoantigen with a subsequent T-cell-mediated inflammatory response. This hypothesis is supported by histopathologic evidence of CD8+ T lymphocytes, activated Langerhans cell, and surrounding necrotic keratinocytes depicting an autoimmune response against some abnormal keratinocyte clones.[3] Histopathology of our patient also showed predominance of CD8+ lymphocytes.
Reports of familial clustering in siblings and in unrelated siblings staying together suggest a possible inflammatory response triggered by simultaneous exposure to same environmental trigger. Infections, trauma, vaccines, medications, and personal and family history of atopy in the form of bronchial asthma, atopic dermatitis, and allergic rhinitis have been proposed as predisposing factors by many authors.
Yaosaka et al. and Karempelis et al. reported the occurrence of the disease in mother and son proposing epigenetic mosaicism as a possible mechanism responsible for this entity.[4],[5] In contrast to genomic mosaicism that cannot be inherited, epigenetic mosaicism involves alteration of gene expression by retrotransposon insertion, methylation/demethylation, and imprinting and the latter one can be inherited.
In our case, both the twin sisters developed the cutaneous lesion within an interval of 1 week. A common in utero triggering factor may have induced mosaicism in both embryos predisposing them to development of skin lesions following a common environmental trigger after birth.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Patrizi A, Neri I, Fiorentini C, Chieregato C, Bonci A. Simultaneous occurrence of lichen striatus in siblings. Pediatr Dermatol 1997;14:293-5.
[Google Scholar]
|
| 2. |
Racette AJ, Adams AD, Kessler SE. Simultaneous lichen striatus in siblings along the same Blaschko line. Pediatr Dermatol 2009;26:50-4.
[Google Scholar]
|
| 3. |
Patrizi A, Neri I, Fiorentini C, Bonci A, Ricci G. Lichen striatus: Clinical and laboratory features of 115 children. Pediatr Dermatol 2004;21:197-204.
[Google Scholar]
|
| 4. |
Yaosaka M, Sawamura D, Iitoyo M, Shibaki A, Shimizu H. Lichen striatus affecting a mother and her son. J Am Acad Dermatol 2005;53:352-3.
[Google Scholar]
|
| 5. |
Karempelis PS, Cely SJ, Davis LS. Lichen striatus in a mother and son. Int J Dermatol 2014;53:e366.
[Google Scholar]
|
Fulltext Views
2,648
PDF downloads
1,494





