Translate this page into:
A review of pulse therapy in 74 patients with pemphigus
Correspondence Address:
Gillian Roga
Dr. Gillian's Skin, Hair, Laser & Cosmetology Clinic, Near Chetana Nursing Home, Mallandur Road, Chikmagalur - 577 101, Karnataka
India
| How to cite this article: Roga G, Augustine M. A review of pulse therapy in 74 patients with pemphigus. Indian J Dermatol Venereol Leprol 2018;84:331-333 |
Sir,
Pemphigus, an autoimmune bullous dermatosis, has an incidence of 0.1–1.8%. Pemphigus foliaceus is usually regarded as having a better prognosis than pemphigus vulgaris. In this study, we compared the clinical course and time taken for controlling the disease activity of pemphigus vulgaris and pemphigus foliaceous on pulse therapy as well as the efficacy of pulse regimens – dexamethasone cyclophosphamide pulse and dexamethasone pulse with azathioprine.
A retrospective study was conducted at the dermatology department of St. John's Medical College and Hospital, Bengaluru on 74 pemphigus patients from January 2009 to February 2015. The diagnosis was confirmed by a Tzanck smear, histopathology and direct immunofluorescence. According to Murrell et al.,[1] control of disease activity is defined as the interval from the baseline to the time at which new lesions cease to form and established lesions begin to heal. Relapse of disease activity is defined by the appearance of three or more new lesions in a month that do not heal spontaneously within 1 week, or by the extension of established lesions, in a patient who has achieved disease control.[1]
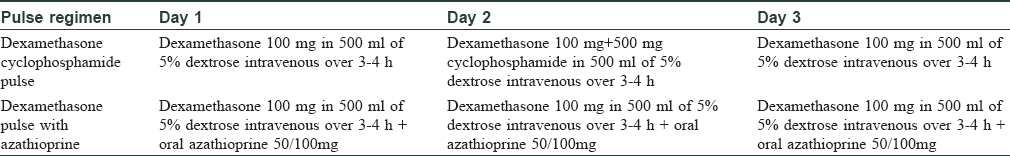
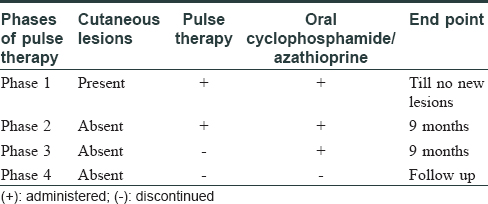
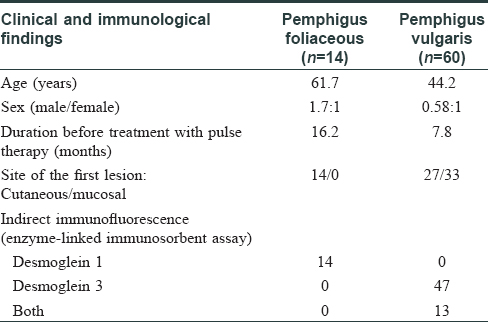
A total of 78 patients were evaluated, of which 4 were lost to follow-up. Of the remaining 74 cases (60 pemphigus vulgaris, 14 pemphigus foliaceus), 31 (41.8%) were males and 43 (58.1%) females, with a male-to-female ratio of 1:1.3. Average age of patients ranged from 41–60 years (52.7%). The patients were administered dexamethasone cyclophosphamide pulse/dexamethasone pulse with azathioprine regimen [Table - 1] and [Table - 2], and were followed up regularly for a period of 3–5 years.[2]
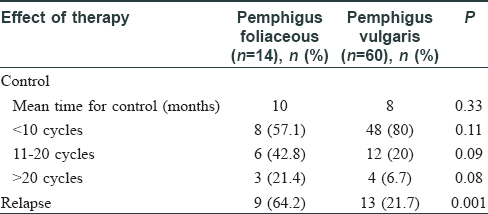
The mean time taken for control of pemphigus was 8.2 months (8 months for pemphigus vulgaris and 10 months for pemphigus foliaceus). We found that 20% of pemphigus vulgaris and 42.8% of pemphigus foliaceus took more than 10 cycles to achieve control (P = 0.09). Further, 6.7% pemphigus vulgaris and 21.4% pemphigus foliaceus patients took more than 20 cycles to achieve control (P = 0.08). Thus, pemphigus foliaceus took longer to achieve control of disease activity than pemphigus vulgaris. Although pemphigus foliaceus is generally thought to have a better prognosis than pemphigus vulgaris, some studies have shown inadequate remission, treatment failure, relapse and steroid dependence in pemphigus foliaceus.[3] However, Zaraa et al.[4] noted no significant difference in age, sex, extent of body surface area involvement, treatment response, rates of relapse, complications or mortality between pemphigus vulgaris and pemphigus foliaceus. Pemphigus vulgaris being clinically more severe tends to be treated earlier, which may be a contributing factor to the better response and lesser relapse in pemphigus vulgaris compared to pemphigus foliaceus.
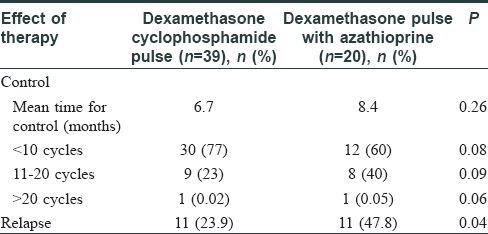
The mean time taken for control of activity was 6.7 months with dexamethasone cyclophosphamide pulse and 8.4 months with dexamethasone pulse with azathioprine. Among patients on dexamethasone cyclophosphamide pulse, 2.5% took more than 20 cycles to achieve control, which was comparable to the results reported by Thappa et al. According to Hassan et al.,[5] dexamethasone pulse with azathioprine took longer than dexamethasone cyclophosphamide pulse to achieve disease control. The time taken for control of disease activity by dexamethasone cyclophosphamide pulse and dexamethasone pulse with azathioprine, in both pemphigus vulgaris and pemphigus foliaceus, showed that in pemphigus vulgaris there was not much difference between time taken for control with dexamethasone cyclophosphamide pulse and dexamethasone pulse with azathioprine. However, in pemphigus foliaceus, dexamethasone pulse with azathioprine took much longer than dexamethasone cyclophosphamide pulse to achieve disease control. Not many studies have been conducted comparing the two types of pemphigus and their response to pulse therapy (dexamethasone cyclophosphamide pulse versus dexamethasone pulse with azathioprine).
The relapse rate seen in pemphigus vulgaris and pemphigus foliaceus were 13 (21.6%) and 9 (64.2%), respectively (P = 0.01), and based on the type of pulse therapy, it was found to be 11 (23.9%) with dexamethasone cyclophosphamide pulse and 11 (47.8%) with dexamethasone pulse with azathioprine (P = 0.04). Both results were statistically significant. The main features of our pemphigus vulgaris and pemphigus foliaceus patients are summarized in [Table - 3], [Table - 4], [Table - 5].
According to Olszewska et al.[6] and Sardana et al.,[7] daily oral cyclophosphamide was found to have faster clinical and immunological remission compared to daily oral azathioprine. Olszewska et al.[6] noted that relapse was faster for azathioprine than cyclophosphamide. Sardana et al.[7] found that, even though a faster onset of remission was noted with cyclophosphamide as compared to azathioprine, the results at the end of 6 months for both drugs was similar. This led to the conclusion that azathioprine should be preferred in view of its safer profile over cyclophosphamide. The “Guidelines for the management of pemphigus vulgaris” proposed by the British Journal of Dermatology also recommend both drugs as adjuvants, with cyclophosphamide considered as an alternative to azathioprine in view of its side-effect profile. In dexamethasone cyclophosphamide pulse, the pulse dose of cyclophosphamide being used, unlike in dexamethasone pulse with azathioprine where only daily dose of azathioprine is used might explain the better response to dexamethasone cyclophosphamide pulse as compared to dexamethasone pulse with azathioprine. The limitations of the study were that it was retrospective and that the patients were not matched for age, disease severity and other confounding factors.
In conclusion, our study suggested that the time taken for control of disease activity and the relapse rate were more in pemphigus foliaceus compared to pemphigus vulgaris. Dexamethasone cyclophosphamide pulse showed a better response with respect to faster control of disease activity and fewer relapses than dexamethasone pulse with azathioprine. Although pemphigus foliaceus was earlier regarded as a milder disease with better prognosis, it was found to be associated with a prolonged course, lower treatment response and higher relapse rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Murrell DF, Dick S, Ahmed AR, Amagai M, Barnadas MA, Borradori L, et al. Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus. J Am Acad Dermatol 2008;58:1043-6.
[Google Scholar]
|
| 2. |
Abraham A, Roga G, Job AM. Pulse therapy in pemphigus: Ready reckoner. Indian J Dermatol 2016;61:314-7.
[Google Scholar]
|
| 3. |
Perry HO. Pemphigus foliaceus. Arch Dermatol 1961;83:52-72.
[Google Scholar]
|
| 4. |
Zaraa I, Mokni M, Hsairi M, Boubaker S, Sellami M, Zitouni M, et al. Pemphigus vulgaris and pemphigus foliaceus: Similar prognosis? Int J Dermatol 2007;46:923-6.
[Google Scholar]
|
| 5. |
Hassan I, Sameem F, Masood QM, Majid I, Abdullah Z, Ahmad QM, et al. Non comparative study on various pulse regimens (DCP, DAP and DMP) in pemphigus: Our experience. Indian J Dermatol 2014;59:30-4.
[Google Scholar]
|
| 6. |
Olszewska M, Kolacinska-Strasz Z, Sulej J, Labecka H, Cwikla J, Natorska U, et al. Efficacy and safety of cyclophosphamide, azathioprine, and cyclosporine (ciclosporin) as adjuvant drugs in pemphigus vulgaris. Am J Clin Dermatol 2007;8:85-92.
[Google Scholar]
|
| 7. |
Sardana K, Agarwal P, Bansal S, Uppal B, Garg VK. A comparative effectiveness research of azathioprine and cyclophosphamide on the clinical and serological response in pemphigus vulgaris. Indian J Dermatol 2016;61:418-26.
[Google Scholar]
|
Fulltext Views
4,767
PDF downloads
2,603





