Translate this page into:
Oral sex related knowledge and oral sex behavior among homosexual and heterosexual men in Belgrade: A cross-sectional study
2 Faculty of Medicine, Institute of Epidemiology, University of Belgrade, Belgrade, Serbia
Correspondence Address:
Hristina D Vlajinac
Institute of Epidemiology, Faculty of Medicine, University of Belgrade, Visegradska 26, 11000 Belgrade
Serbia
| How to cite this article: Bjekic MD, Sipetic-Grujicic SB, Vlajinac HD, Nikolic AM. Oral sex related knowledge and oral sex behavior among homosexual and heterosexual men in Belgrade: A cross-sectional study. Indian J Dermatol Venereol Leprol 2018;84:563-568 |
Abstract
Background: Although the risk of sexually transmitted infections is far greater during vaginal and anal sex than during oral sex, increasing practice of oral sex and low rates of barrier method use will probably increase the relative importance of oral sex as a route of transmission for genital pathogens.
Aims: The aim of this study was to evaluate knowledge and attitudes about oral sex and sexually transmitted infections, as well as oral sex practices, both among heterosexuals and homosexual men and to compare those two groups.
Materials and Methods: In this cross-sectional study, data were collected from consecutive sexually active male patients who ever had oral sex and who attended counselling for sexually transmitted infections at the City Institute for Skin and Venereal Diseases in Belgrade from March to June 2016. One dermatologist interviewed all participants.
Results: The study included 359 men who ever had oral sex, 95 (26.5%) homosexual and 264 (73.5%) heterosexual men. In comparison with heterosexual men, homosexual men had considerably more lifetime sexual partners and oral sex partners during the past 3 months, and significantly more frequently practiced oral-anal sex. Oral-sex related knowledge of all participants was unsatisfactory [correct answers were given by 95 (26.5%) to 277 (77.2%) participants], but it was significantly better in homosexual men than in heterosexual. Frequency of condom use and human immunodeficiency virus testing was also significantly higher in the case of homosexual than heterosexual men.
Limitations: The study was not performed in representative sample of population. It was restricted to the patients. Consequently it is questionable whether the results obtained could be generalized.
Conclusion: Oral sex related knowledge deficits and risky oral sex practice exist in both homosexual and heterosexual men. These findings indicate a need for effective public health campaign and patient education about the risks of unprotected oral sex.
Introduction
Sexually transmitted infections are infectious diseases transmitted from person to person during sexual contact not only through vaginal intercourse. Among men who have sex with men, unprotected receptive anal sex poses the highest risk of HIV transmission.[1] Although the risk of HIV transmission by oral sex is small, it is well established that oral-genital and oral-anal sex may lead to the transmission of a wide variety of nonviral and viral sexually transmitted infections.[2],[3],[4]
Oral sex involves giving or receiving oral stimulation to the penis (fellatio), the vagina (cunnilingus), and/or the anus (anilingus). Some men who were engaged in oral sex believed that they were practicing safe sex and were surprised when they received a venereal disease diagnosis.[5] Because the risk of HIV transmission through oral sex is much lower than during anal or vaginal sex, persons might wrongly consider that unprotected oral sex is safe or a no-risk sexual practice.[6]
Oral sex is commonly practiced by sexually active male-female and same-gender couples of various ages, including adolescents. People may engage in oral sex as part of foreplay before sexual intercourse or during or following intercourse. The National Survey of Family Growth, a survey of 15–44-year-olds in the United States, found that 48% of males aged 15–19 had oral sex with a female partner, whereas among 20–24-year-old men this percentage was 80%.[7] In the same study, among adults aged 25–44, 90% of men had oral sex with an opposite-sex partner. Another study has shown that higher percentage of boys aged 15–19 reported receiving oral sex (47%) than giving oral sex (35%) and among males aged 15–24, 24% had first oral sex before their first intercourse.[8]
According to the study of Rosenberg et al. conducted in the United States, the most commonly reported sexual behaviors during the most recent sexual event among homosexual men was kissing a partner on the mouth (74.5%), followed by oral sex (72.7%), whereas anal intercourse occurred among 37.2%.[9]
Although we do not possess data regarding oral sex practices in our country, during an outbreak of early syphilis in Belgrade in 2011, the majority of patients acquired syphilis infection through oral sex.[10] Unprotected oral sex is a risky behavior and bad oral health and oral lesions increase the chances of transmission of sexual pathogens.[11]
The aim of this study was to evaluate our patient's knowledge and attitudes about oral sex and sexually transmitted infections, and their oral sex practices, both among heterosexuals and homosexual men and to compare those two groups to identify any distinct need with regard to the prevention of venereal diseases contracted by oral sex.
Materials and Methods
In this cross-sectional study, data were collected from consecutive sexually active male patients who had oral sex and attended counselling for sexually transmitted infections at the City Institute for Skin and Venereal Diseases in Belgrade.
The study was conducted between 1 March and 30 June 2016. It covered 264 heterosexual and 95 homosexual men. One dermatologist interviewed all participants. The following data were obtained using a questionnaire: demographic characteristics included age, educational level, and marital status, while sexual history data included sexual activity, age at first sexual intercourse, number of sexual partners, condom use during vaginal and anal intercourse, oral sex practices, use of condoms or dental dams during oral sex, and history of sexually transmitted infections. The questionnaire also included questions about oral sex, sexually transmitted infections, and HIV, as well as questions about their oral health.
The research was approved by the Ethics Committee of the City Institute for Skin and Venereal Diseases in Belgrade.
Data were presented as numbers and percentages. Chi-square test or Fisher's exact P test were used to assess differences between heterosexual and homosexual men.
Results
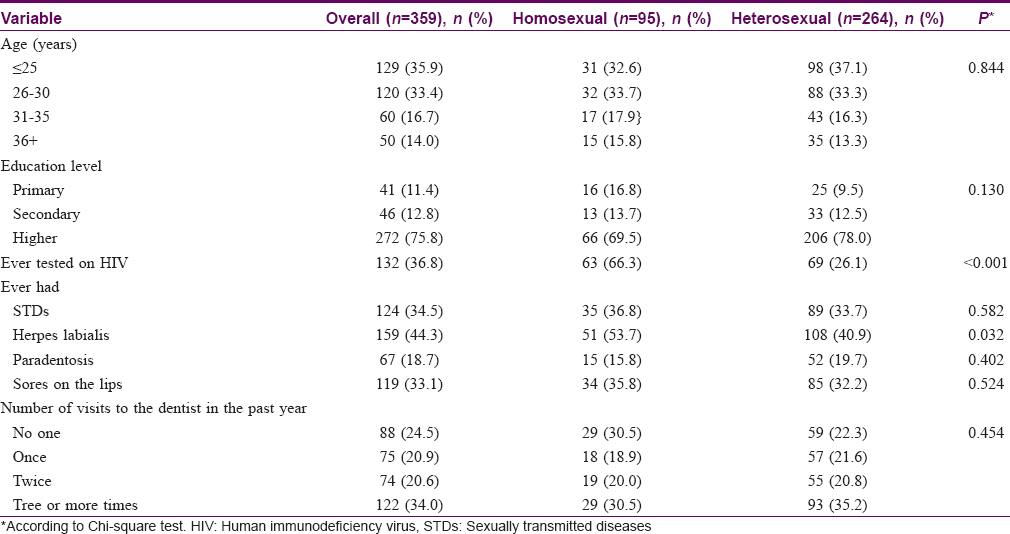
The study included 359 men who had oral sex – 95 (26.5%) homosexual and 264 (73.5%) heterosexual [Table - 1]. Majority of participants, 249 (69.3%), were up to 30 years old and 272 (75.8%) had higher education. Sexually transmitted disease in personal history was reported by 124 (34.5%) participants, bleeding gums (paradentosis) by 67 (18.7%), and prevalence of sores on the lips by 119 (33.1%). Homosexual and heterosexual men did not significantly differ by age and education level. Similarly, percentage of participants who reported sexually transmitted diseases and oral infections in their past histories was similar in both groups. Exception was herpes labialis considerably more frequently reported by homosexual then by heterosexual men [51 (53.7%) vs. 108 (40.9%), P = 0.032]. Homosexual men were also more likely than heterosexual to be tested for HIV [63 (66.3%) vs. 69 (26.1%), P < 0.001]. Compared groups did not significantly differ in the number of visits to the dentist during the past year.
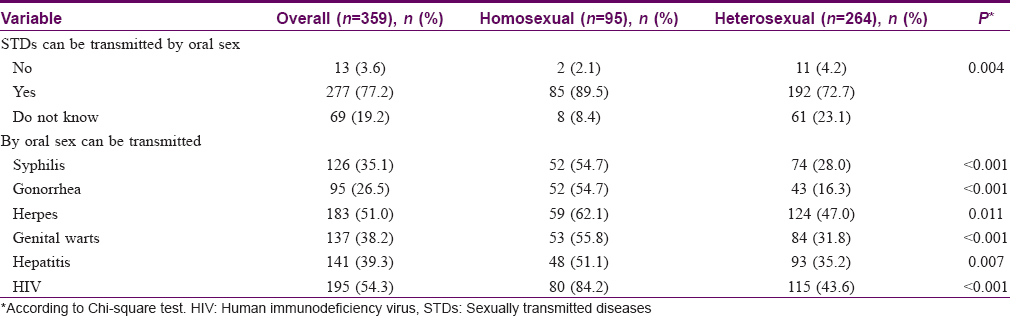
Oral sex-related knowledge of study participants is presented in [Table - 2]. It shows that 277 (77.2%) participants knew that sexually transmitted diseases can be transmitted by oral sex. Oral sex as a risk factor for transmission of single sexually transmitted disease was recognized by 126 (35.1%) participants for syphilis, 95 (26.5%) for gonorrhoea, 183 (51.0%) for herpes, 137 (38.2%) for genital warts, 141 (39.3%) for hepatitis, and 195 (54.3%) for HIV infection. Oral sex-related knowledge was significantly better in homosexual men than in heterosexual (P values from 0.011 to <0.001).
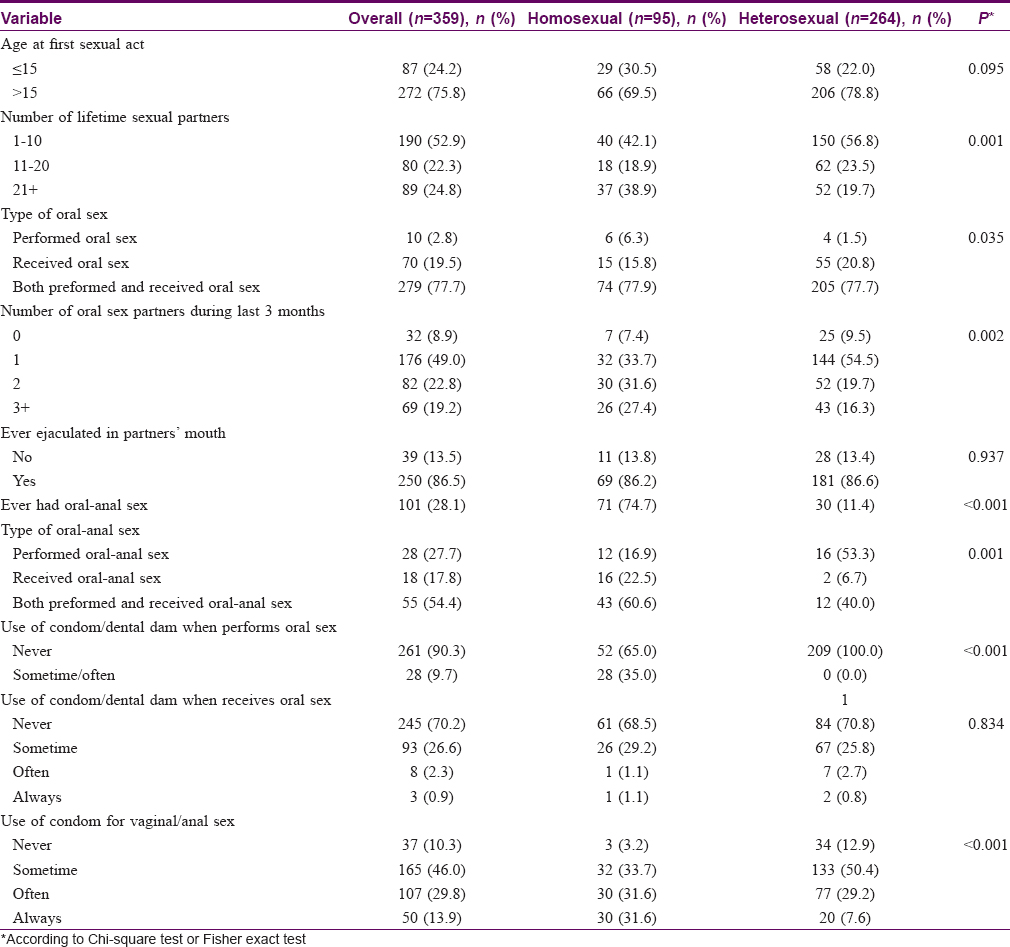
Sexual debut was most frequent after 15 years of age [Table - 3], similarly in homosexual and heterosexual men [66 (69.5%) vs. 206 (78.8%)], but homosexual men reported greater number of lifetime sexual partners (P = 0.001). Number of oral sex partners during the last 3 months was also higher among homosexual men (P = 0.002). In comparison with heterosexual men, homosexual men more frequently performed than received oral sex (P = 0.035), but the majority of both groups used both types of oral sex [74 (77.9%) vs. 205 (77.7%)] and reported ejaculating in the partner's mouth [69 (86.2%) vs. 181 (86.6%)]. Ever having oral-anal sex was reported by 101 (28.1%) participants, significantly more frequently by homosexual than heterosexual men [71 (74.7%) vs. 30 (11.4%) P < 0.001]. In comparison with heterosexual men, homosexual men significantly more frequently received than performed oral-anal sex or used both types of it (P = 0.001). Condom has not been used for performing oral sex by 52 (65.0%) homosexual and 209 (100.0%) heterosexual, the difference being significant (P < 0.001). Use of condom for receiving oral sex did not differ between the compared groups. Majority of participants, 245 (70.2%), never used it and only 3 (0.9%) always used it. For vaginal/anal sex, condom was used significantly more frequently by homosexual than heterosexual men (P < 0.001). It was always used by 30 (31.6%) homosexual vs. 20 (7.6%) heterosexual men often used by 30 (31.6%) homosexual and 77 (29.2%) heterosexual men, and was never or sometimes used by 35 (36.9%) homosexual and 167 (63.3%) of heterosexual men.
Discussion
In the present study, in comparison with heterosexual men, homosexual men had considerably more lifetime sexual partners and oral sex partners during the past 3 months, and significantly more frequently practiced oral-anal sex. Oral sex-related knowledge of all participants was unsatisfactory [correct answers were given by 95 (26.5%) to 277 (77.2%) participants], but it was significantly better in homosexual men than in heterosexual. Frequency of condom use and HIV testing was also significantly higher in the case of homosexual than heterosexual men.
In this study, special attention was paid to homosexual men because, according to literature data, they more frequently suffer from sexually transmitted infections, including HIV in comparison to heterosexual men.[12],[13] According to the Centre for Disease Control and Prevention estimates, HIV and early syphilis rates among homosexual men are more than 40 times higher than those among heterosexuals.[12] Glick et al. reported that homosexual men have higher periods at partnership acquisition, higher prevalence of partnership concurrency, and more age-disassortative mixing than heterosexuals.[13] This helps to explain higher HIV/sexually transmitted infections rates among homosexual men. In recent years, in Serbia, increasing trend of reported sexual transmission was notified among newly diagnosed HIV cases (88% in 2011 versus 15% in 1991). In addition, when it comes to HIV transmission categories among newly diagnosed HIV-infected people reported during 2002–2011 in Serbia, there is a clear increasing trend among homosexual men (57% of all reported HIV cases in 2011 versus 26% in 2002).[14] Men accounted for most cases of syphilis in Belgrade, the capital of Serbia, during 2010–2014, with the vast majority of those cases occurring among homosexual men.[10] In the present study, similar percentage of men in compared groups reported sexually transmitted diseases in personal history, but we have no data about their lifetime frequency of sexually transmitted diseases.
Oral sex is a common practice both in homosexual and heterosexual men, but former are more frequently engaged in this activity.[7],[8],[9] This study included only men (homosexual and heterosexual) who had oral sex. According to the results obtained, homosexual men reported greater number of lifetime sexual partners as well as greater number of oral sex partners during the last 3 months. Oral sex with ejaculation was perceived as more risky than oral sex without ejaculation, and the risk of HIV transmission from exposure to saliva is considerably smaller than the risk from exposure to semen.[15] Majority of our participants in both groups (86.5%) did not avoid ejaculating into their partner's mouth and more than 2/3 of participants did not use condom when receiving oral sex, although seminal fluid may be the reservoir for sexually transmitted pathogens including HIV. None of heterosexual men used a dental dam (rectangular squares of latex) when performing oral sex. Moreover, they had never heard of a dental dam. In the study conducted in the United Kingdom, 20% of all young people who have reported fellatio had used a condom.[16] The most common reasons given by men for not using a condom were that fellatio feels better without a condom and that they simply had no thought about using one. In our study, homosexual men reported more consistent condom use during anal sex than heterosexuals reported condom use during vaginal sex, which is in line with the results of the study by Glick et al.[13]
Oral sex, including oral-anal sex, carries risk of transmitting HIV and other sexually transmitted infections.[2],[3] Although the risk of sexually transmitted infections is far greater during vaginal and anal sex than during oral sex, increasing practice of oral sex and low rates of barrier method use will probably increase the relative importance of oral sex as a route of transmission for genital pathogens.[2],[3] During an outbreak of early syphilis among homosexual men in Belgrade, 59.3% patients acquired syphilis infection through unprotected oral sex.[10] Outbreaks of syphilis reported in Brighton and Manchester, United Kingdom showed that one-third of homosexual men included in the study acquired syphilis through oral sex.[17] Homosexual men have low awareness of transmission of sexually transmitted infections due to diverse types of sexual behavior other than anal intercourse.
The present study is the first one that attempted to examine awareness of sexually transmitted infections/HIV transmission by oral sex among men in Belgrade. Our results show that almost one-fourth of study participants did not know that oral sex could be a mode for transmission of venereal diseases. Better oral sex-related knowledge was among homosexual men. One of possible explanations could be the fact that our homosexual men significantly more frequently had voluntary confidential counselling and testing for HIV. This is a widespread preventive practice that is believed to have the potential to affect increase of knowledge, change of attitudes, and decrease of risky behavior for HIV and other sexually transmitted infections.[18] Other explanation for better knowledge among homosexual men could be the fact that prevalence of syphilis and HIV infection in our country is significantly higher in this group, wherefore they received education from physicians during the course of treatment. These facts suggest that health care providers play a valuable role in health education.
Not using a condom (never or sometimes) when receiving oral sex was reported by more than 95% of participants in both groups, although homosexual men had better knowledge and knew that oral sex poses risks for transmission of venereal diseases. This is in line with the results of Stone et al.[16] Better knowledge of sexually transmitted infections prevention is insufficient to motivate the adoption or maintenance of safer sexual behavior.[19] In our opinion, an already established sexual behavior is difficult to change even after sexually transmitted infection, which emphasizes the importance of early sexual education. In our country, sexual education is not a part of the education system.
In various acts of oral sex there is a risk of infections since pre-seminal and seminal fluid, vaginal and rectal secretions, and menstrual blood can get into the mouth. Oral lesions and oral diseases (candidiasis, herpes simplex virus infection, aphtous ulcers, bleeding gums) may be a port of entrance of sexual pathogens. Periodic oral health check-up is mandatory among the people frequently involved in oral sex.
The study has some limitations. The main one is that it was not performed in representative sample of population. Instead, the study included patients who attended the counselling for sexually transmitted infections at the City Institute for Skin and Venereal Diseases in Belgrade, and consequently it is questionable whether the result obtained could be generalized. In addition, the cross-sectional data in this study were prone to potential recall bias. Further, we did not collect data about number of lifetime sexually transmitted infections in history of participants and so we could not evaluate connection between their frequency and participants' sexual behavior and oral-sex related knowledge.
Summary
Sexually transmitted infections are among the world's most common diseases and their burden on the health care system and healthcare expenditure is great especially in the lower-middle-income countries because of lower educational and socioeconomic status and inadequacies in health service provision and health care seeking.[20] The results of the present study showed that oral sex-related knowledge deficits and risky oral sex practice exists in both homosexual and heterosexual men. These findings indicate a need for effective public health campaign with emphasis on early sexual education as well as patient education about the risks of unprotected oral sex. Physicians should advise patients to use condoms or dental dams when performing or receiving oral sex especially with a partner whose sexually transmitted infection/HIV status is unknown.
Financial support and sponsorship
This study was supported by the Ministry of Education, Science and Technological Development, Republic of Serbia, through Contract No. 175042.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP, et al. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. Am J Epidemiol 1999;150:306-11.
[Google Scholar]
|
| 2. |
Edwards S, Carne C. Oral sex and transmission of non-viral STIs. Sex Transm Infect 1998;74:95-100.
[Google Scholar]
|
| 3. |
Edwards S, Carne C. Oral sex and the transmission of viral STIs. Sex Transm Infect 1998;74:6-10.
[Google Scholar]
|
| 4. |
Hawkins DA. Oral sex and HIV transmission. Sex Transm Infect 2001;77:307-8.
[Google Scholar]
|
| 5. |
Centers for Disease Control and Prevention (CDC). Transmission of primary and secondary syphilis by oral sex – Chicago, Illinois, 1998-2002. MMWR Morb Mortal Wkly Rep 2004;53:966-8.
[Google Scholar]
|
| 6. |
Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW. Reducing the risk of sexual HIV transmission: Quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use. Sex Transm Dis 2002;29:38-43.
[Google Scholar]
|
| 7. |
Chandra A, Mosher WD, Copen C, Sionean C. Sexual behavior, sexual attraction, and sexual identity in the United States: Data from the 2006-2008 National Survey of Family Growth. Natl Health Stat Report 2011;36:1-36.
[Google Scholar]
|
| 8. |
Copen CE, Chandra A, Martinez G. Prevalence and timing of oral sex with opposite-sex partners among females and males aged 15-24 years: United States, 2007-2010. Natl Health Stat Report 2012;56:1-14.
[Google Scholar]
|
| 9. |
Rosenberger JG, Reece M, Schick V, Herbenick D, Novak DS, Van Der Pol B, et al. Sexual behaviors and situational characteristics of most recent male-partnered sexual event among gay and bisexually identified men in the United States. J Sex Med 2011;8:3040-50.
[Google Scholar]
|
| 10. |
Bjekić M, Šipetić S. An outbreak of early syphilis in patients registered at City Institute for Skin and Venereal Diseases in Belgrade from 2010 to 2012: A case series of 86 patients. Serb J Dermatol Venereol 2013;5:65-71.
[Google Scholar]
|
| 11. |
Saini R, Saini S, Sharma S. Oral sex, oral health and orogenital infections. J Glob Infect Dis 2010;2:57-62.
[Google Scholar]
|
| 12. |
Purcell DW, Johnson C, Lansay A, Prejean J, Stein R, Denning P, et al. Calculating disease rates for risk groups: Estimating the national population size of men who have sex with men (abstract) paper presented at: National STD Prevention Conference. Atlanta, Georgia; 2010.
[Google Scholar]
|
| 13. |
Glick SN, Morris M, Foxman B, Aral SO, Manhart LE, Holmes KK, et al. Acomparison of sexual behavior patterns among men who have sex with men and heterosexual men and women. J Acquir Immune Defic Syndr 2012;60:83-90.
[Google Scholar]
|
| 14. |
Institute of Public Health of Serbia, Dr Milan Jovanovic Batut. Center for Disease Control and Prevention: Report of Infectious Diseases in the Republic of Serbia. Belgrade: Institute of Public Health of Serbia, Dr Milan Jovanovic Batut; 2012.
[Google Scholar]
|
| 15. |
Rothenberg RB, Scarlett M, del Rio C, Reznik D, O'Daniels C. Oral transmission of HIV. AIDS 1998;12:2095-105.
[Google Scholar]
|
| 16. |
Stone N, Hatherall B, Ingham R, McEachran J. Oral sex and condom use among young people in the United Kingdom. Perspect Sex Reprod Health 2006;38:6-12.
[Google Scholar]
|
| 17. |
Increased transmission of syphilis in Brighton and greater Manchester among men who have sex with men. Commun Dis Rep CDR Wkly 2000;10:383, 386.
[Google Scholar]
|
| 18. |
Coovadia HM. Access to voluntary counseling and testing for HIV in developing countries. Ann N Y Acad Sci 2000;918:57-63.
[Google Scholar]
|
| 19. |
Diclemente RJ, Wingood GM, Sionean C, Crosby R, Harrington K, Davies S, et al. Association of adolescents' history of sexually transmitted disease (STD) and their current high-risk behavior and STD status: A case for intensifying clinic-based prevention efforts. Sex Transm Dis 2002;29:503-9.
[Google Scholar]
|
| 20. |
Terris-Prestholt F, Vyas S, Kumaranayake L, Mayaud P, Watts C. The costs of treating curable sexually transmitted infections in low- and middle-income countries: A systematic review. Sex Transm Dis 2006;33:S153-66.
[Google Scholar]
|
Fulltext Views
10,621
PDF downloads
1,612





