Translate this page into:
Hypopigmented and acneiform lesions: An unusual initial presentation of adult-onset multisystem Langerhans cell histiocytosis
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3 Department of Internal Medicine and Hematology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh - 160 012
India
| How to cite this article: Bishnoi A, De D, Khullar G, Parsad D, Handa S, Vishwajeet V, Saikia UN, Prakash G. Hypopigmented and acneiform lesions: An unusual initial presentation of adult-onset multisystem Langerhans cell histiocytosis. Indian J Dermatol Venereol Leprol 2018;84:621-626 |
Dear Sir,
Langerhans cell histiocytosis is a rare neoplasm of Langerhans cells.[1] Its incidence in pediatric population is 4–5 per million, whereas incidence in adults is approximately one-third of this.[2] The cutaneous involvement in adult-onset Langerhans cell histiocytosis commonly encountered in association with multisystem disease. Isolated cutaneous Langerhans cell histiocytosis is rare. Heterogeneous cutaneous manifestations, such as intertrigo, perianal erosions, centrofacial fleshy plaques and prurigo-like nodules, have been described in both multisystem and isolated cutaneous variants of adult-onset Langerhans cell histiocytosis.[3],[4] Here, we describe two adult patients presenting with hypopigmented and acneiform lesions finally being diagnosed as multisystem Langerhans cell histiocytosis.
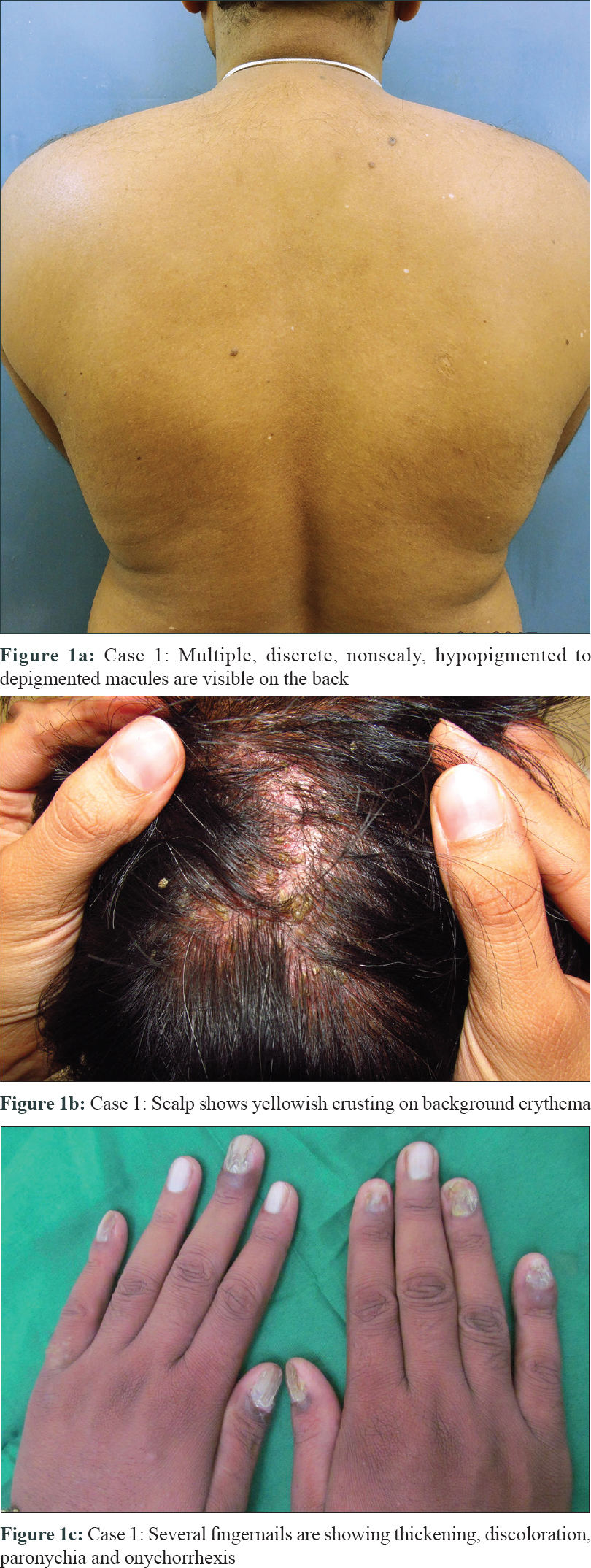
Case 1: A 35-year-old man presented with multiple, discrete, 2–3 mm, nonscaly, hypopigmented to depigmented macules on the back which were noticed recently [Figure - 1]a. He also had recalcitrant papulopustular lesions with crusting on scalp for 5 years [Figure - 1]b and nail dystrophy [Figure - 1]c. Several finger and toenails had thickening, discoloration, paronychia and onychorrhexis. Potassium hydroxide mount and fungal cultures were negative from nail clippings. Mucosae and hair were normal. There was no lymphadenopathy or hepatosplenomegaly.
 |
| Figure 1: |
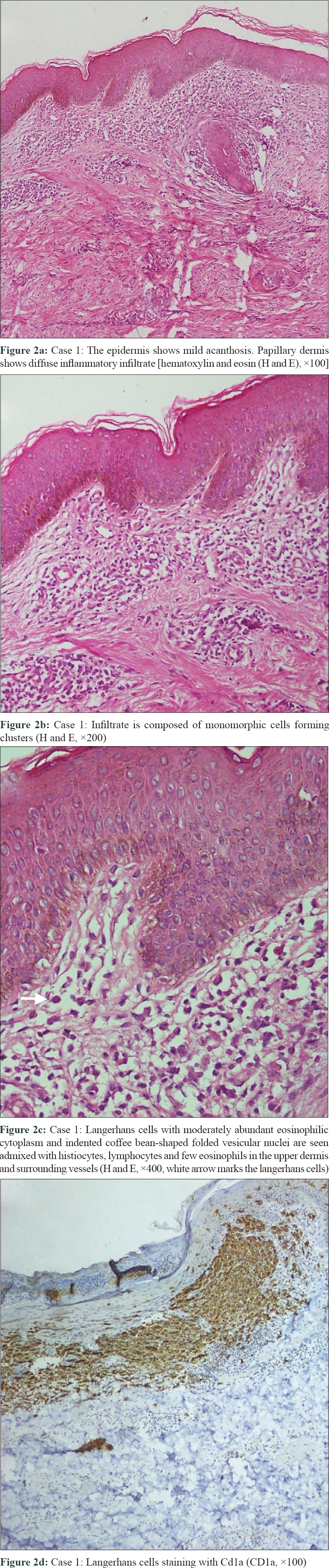
Biopsy from a hypopigmented lesion demonstrated large, pale cells with cleaved nuclei suggestive of Langerhans cells, infiltrating the papillary dermis [Figure - 2]a–c]. On immunohistochemistry, these cells were positive for CD1a. Epidermotropism was inconspicuous [Figure - 2]d. On further probing, patient admitted having dyspnea, polydipsia and polyuria for 1 year. There was no history of smoking. Laboratory investigations of complete blood count, liver and renal function tests were normal. Positron emission tomography scan and computed tomography of chest revealed left femoral condyle infiltrates and fibrotic nodules in upper and mid zones of both the lungs respectively. Bronchoalveolar lavage showed presence of Langerhans cells in the aspirate. Plasma osmolality was increased (value: 370 mOsm/kg), whereas urine osmolality was found to be decreased (value: 145 mOsm/kg), with urine to plasma osmolality ratio being <1. Magnetic resonance imaging of brain showed absence of normal pituitary hyperintensity signal suggesting presence of central diabetes insipidus. He was started on topical corticosteroids and referred to hematology services where vasopressin nasal spray, oral prednisolone and weekly intravenous vinblastine were initiated. After 3 months, skin lesions had resolved, nails were showing improvement and polyuria and polydipsia had subsided. Treatment was continued for 6 months. Post-treatment positron emission tomography scan showed resolution of disease activity in bones. Mild fibrotic changes on computed tomography chest persisted, though there was improvement in dyspnea. Patient was still receiving vasopressin at the time of writing this report.
 |
| Figure 2: |
Case 2: A 21-year-old man had papulopustular lesions on the face, scalp and back for 2 years. Examination revealed multiple, discrete, translucent, erythematous papulopustules of 2–3 mm size, having central umbilication and crusting, clustered on perinasal area and temporal scalp [Figure - 3]a. Lower gingiva had a firm, nontender, immobile swelling of around 1 × 1 cm in size [Figure - 3]b. Teeth and nails were normal. Submandibular lymph nodes were enlarged (maximum size, 3 × 2 cm), firm and non-matted. He was a nonsmoker and admitted having polydipsia and polyuria for last 6 months.
 |
| Figure 3: |
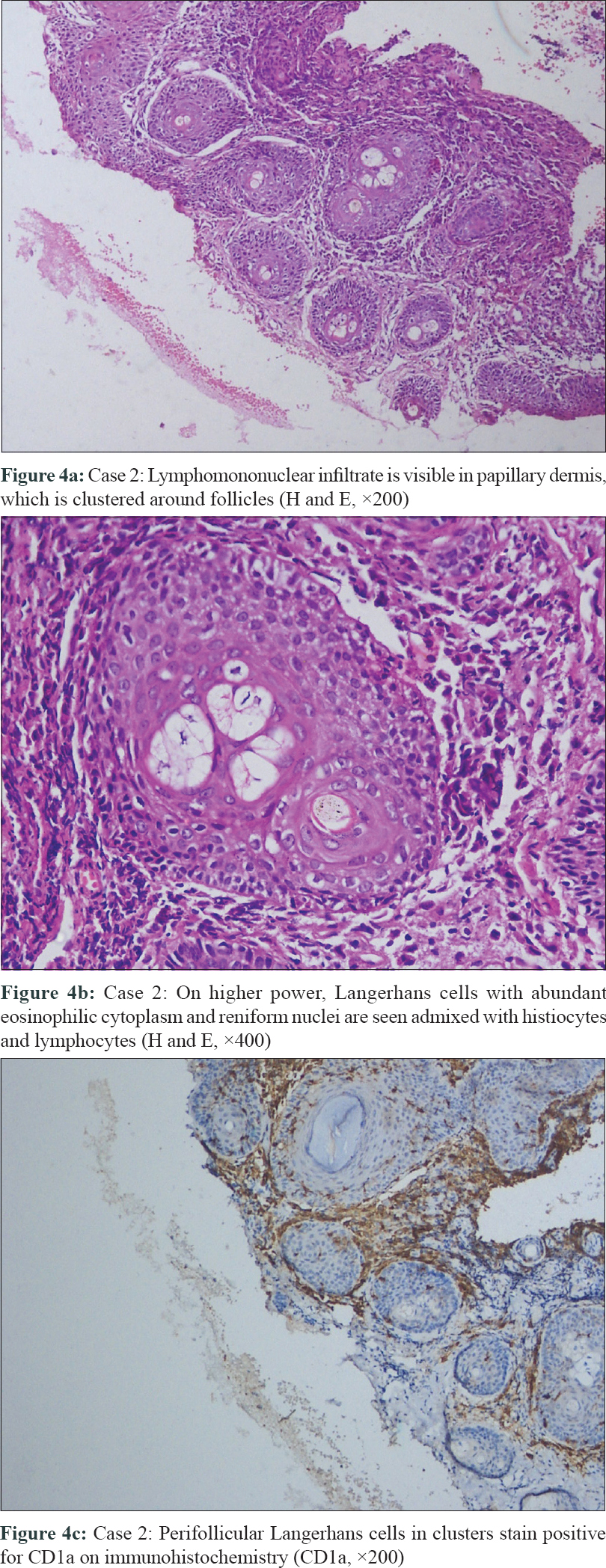
Biopsy from a facial papule revealed papillary dermal infiltration by Langerhans cells. On higher power, these cells were prominently clustered around hair follicles and stained positive for CD1a on immunohistochemistry [Figure - 4]a–c]. Systemic investigations revealed central diabetes insipidus, minimal pleural effusion and lytic areas in frontal skull, mandible and thoracic vertebrae. Patient was referred to hematology services and he lost to follow-up subsequently.
 |
| Figure 4: |
Langerhans cell histiocytosis is characterized by abnormal proliferation of Langerhans cells in various organ systems, and can be classified as single-system (unifocal or multifocal) or multisystem disease. Adult-onset Langerhans cell histiocytosis, though less well studied than its pediatric counterpart, can have variable presentations. Rapidly progressive form seen commonly in infants and children is less commonly observed in adults.[3],[5] Moreover, pulmonary involvement is distinctly more common in adult-onset disease and has significant association with smoking. In a large retrospective study, Arico and colleagues evaluated 274 patients with adult-onset Langerhans cell histiocytosis. In single-system disease, skin was the third most common organ of involvement constituting 7.01% cases, after lungs (51.1%) and bone (38.8%). In multisystem disease, skin was involved in 50.5% cases (third most commonly involved organ) after bone (66%) and lungs (61.7%).[6]
Diabetes insipidus was diagnosed in both of our patients and is a peculiar manifestation of Langerhans cell histiocytosis. Arico et al. observed it in 29.6% of the patients in their retrospective review.[6] The frequency of this irreversible sequela is almost similar in adults and children. Diabetes insipidus does not respond to routine Langerhans cell histiocytosis directed treatment and requires life-long vasopressin treatment.[6]
Langerhans cell histiocytosis is a rare, but potential mimicker of common dermatoses such as seborrheic dermatitis, folliculitis, acne and intertrigo. Therefore, cutaneous manifestations, though common at the time of presentation, are easily misdiagnosed or overlooked.[3] Moreover, multisystem Langerhans cell histiocytosis can present with both diffuse or localized skin involvement.[4],[7] Nail involvement is considered a marker of multisystem involvement and can present as paronychia, splitting and nail loss.[8] Though our patient did not give consent for nail biopsy, no response with antifungals, a negative fungal culture and appreciable response to systemic treatment supports the diagnosis of Langerhans cell histiocytosis in nails of the first patient.
Neoplastic Langerhans cells are predominantly present in papillary dermis and have a tendency to infiltrate epidermis, and rarely extend to reticular dermis.[9] However, none of our patients showed significant epidermotropism. Perinasal facial papules and predominant perifollicular infiltrate observed in histopathology of the second patient are similar to prior observations made in adult Langerhans cell histiocytosis that showed a clinical predilection for appendage-rich sites and a periappendageal affinity of the infiltrate on histopathology.[10],[11]
Clinical differential diagnoses considered for our patients were acne vulgaris, folliculitis and acne agminata for facial lesions and idiopathic guttate hypomelanosis and punctate/confetti-like vitiligo for depigmented lesions on trunk. But histopathology and immunohistochemistry clinched the accurate diagnosis.
Because of relative ease of obtaining skin biopsy, we emphasize on having a high degree of clinical suspicion for Langerhans cell histiocytosis and low threshold for skin biopsy in adults having recalcitrant acneiform lesions on centrofacial area and systemic symptoms. We also describe a novel cutaneous manifestation of adult-onset Langerhans cell histiocytosis in the form of hypopigmented/depigmented macules, which have been rarely described even in pediatric age group.[12-14]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood 2016;127:2672-81.
[Google Scholar]
|
| 2. |
Singh A, Prieto VG, Czelusta A, McClain KL, Duvic M. Adult Langerhans cell histiocytosis limited to the skin. Dermatology 2003;207:157-61.
[Google Scholar]
|
| 3. |
Aydogan K, Tunali S, Koran Karadogan S, Balaban Adim S, Turan H. Adult-onset Langerhans cell histiocytosis confined to the skin. J Eur Acad Dermatol Venereol 2006;20:890-2.
[Google Scholar]
|
| 4. |
Reddy IS, Gowrishankar S, Somani VK, Murthy DB. Adult onset Langerhans cell histiocytosis: Report of two patients. Indian J Dermatol Venereol Leprol 2014;80:560-2.
[Google Scholar]
|
| 5. |
Girschikofsky M, Arico M, Castillo D, Chu A, Doberauer C, Fichter J, et al. Management of adult patients with Langerhans cell histiocytosis: Recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis 2013;8:72.
[Google Scholar]
|
| 6. |
Aricò M, Girschikofsky M, Généreau T, Klersy C, McClain K, Grois N, et al. Langerhans cell histiocytosis in adults. Report from the international registry of the histiocyte society. Eur J Cancer 2003;39:2341-8.
[Google Scholar]
|
| 7. |
Querings K, Starz H, Balda BR. Clinical spectrum of cutaneous Langerhans' cell histiocytosis mimicking various diseases. Acta Derm Venereol 2006;86:39-43.
[Google Scholar]
|
| 8. |
Ashena Z, Alavi S, Arzanian MT, Eshghi P. Nail involvement in Langerhans cell histiocytosis. Pediatr Hematol Oncol 2007;24:45-51.
[Google Scholar]
|
| 9. |
Abbas O, Bhawan J. Epidermotropic lesions: A review. J Cutan Pathol 2009;36:1037-52.
[Google Scholar]
|
| 10. |
Helm KF, Lookingbill DP, Marks JG Jr. A clinical and pathologic study of histiocytosis X in adults. J Am Acad Dermatol 1993;29:166-70.
[Google Scholar]
|
| 11. |
Hancox JG, James AP, Madden C, Wallace CA, McMichael AJ. Adult onset folliculocentric Langerhans cell histiocytosis confined to the scalp. Am J Dermatopathol 2004;26:123-6.
[Google Scholar]
|
| 12. |
Kaddu S, Mulyowa G, Kovarik C. Hypopigmented scaly, scalp and facial lesions and disfiguring exopthalmus. Langerhans cell histiocytosis (LCH). Clin Exp Dermatol 2010;35:e52-3.
[Google Scholar]
|
| 13. |
Feroze K, Unni M, Jayasree MG, Seethalekshmy NV. Langerhans cell histiocytosis presenting with hypopigmented macules. Indian J Dermatol Venereol Leprol 2008;74:670-2.
[Google Scholar]
|
| 14. |
Mehta B, Amladi S. Langerhans cell histiocytosis presenting as hypopigmented papules. Pediatr Dermatol 2010;27:215-7.
[Google Scholar]
|
Fulltext Views
2,976
PDF downloads
1,794





