Translate this page into:
Gabapentin and pregabalin in dermatology
Correspondence Address:
Asit Mittal
Department of Dermatology, Venereology and Leprology, R. N. T. Medical College, Udaipur - 313 001, Rajasthan
India
| How to cite this article: Mittal A, Agarwal C, Balai M, Taneja A. Gabapentin and pregabalin in dermatology. Indian J Dermatol Venereol Leprol 2018;84:634-640 |
Introduction
The anticonvulsants gabapentin and pregabalin are of interest to dermatologists. The drugs have found uses in conditions that are frequently of interest to dermatologists and often primarily present to a dermatologist. These drugs are likely to find greater use in dermatology practice in future. This review is intended to familiarize dermatologists with these drugs.
History
Pregabalin was synthesized in 1990 as an anticonvulsant. It was invented by Richard Bruce Silverman at Northwestern University in Chicago, Illinois. The drug was approved in the European Union in 2004. The US received Food and Drug Administration approval for use in treating epilepsy, diabetic neuropathic pain and postherpetic neuralgia in December 2004. Gabapentin was originally approved by the U.S. Food and Drug Administration in December 1993 for use as an adjuvant medication to control partial seizures in adults; that indication was extended to children in 2000. In 2004, its use for treating postherpetic neuralgia (neuropathic pain following shingles) was approved.
Mechanism of Action
Gabapentin consists of a gamma amino butyric acid molecule covalently bound to a lipophilic cyclohexane ring (C9H17 NO2) [Figure - 1]. It is a centrally active gamma amino butyric acid agonist, with its high lipid solubility aimed at facilitating its transfer across the blood–brain barrier. Despite their design as gamma amino butyric acid agonists, neither gabapentin nor pregabalin mimics gamma amino butyric acid when iontophoretically applied to neurons in primary culture.[1] These compounds bind with a high affinity to a protein in cortical membrane with aminoacid sequence identical to that of calcium channel subunit α2δ-1.[2] It has been speculated that the anticonvulsant effect of gabapentin is mediated by α2δ-1 protein, but whether and how binding of gabapentin to this protein regulate neuronal activity remains unclear.[1] Pregabalin binding is reduced but not eliminated in mice carrying a mutation in α2δ-1 protein.[3] It is unclear whether the anticonvulsant and analgesic effect of gabapentin and pregabalin are mediated by affecting calcium currents, and if so how.
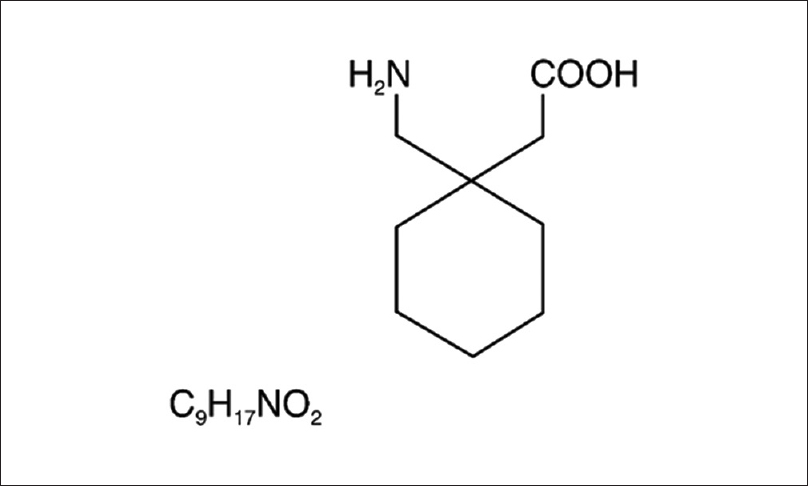 |
| Figure 1: Chemical structure of gabapentin |
Pharmacokinetics
Gabapentin is not metabolized. It is eliminated via renal mechanism and is excreted unchanged. It does not induce hepatic enzymes. Absorption is nonlinear and dose-dependent at very high doses, but the elimination kinetics is linear. The drug is not bound to plasma protein. Drug–drug interactions are negligible. The half-life is relatively short ranging from 5.0 to 8.0 hours, hence, it is administered two or three times per day.[4] It requires gradual adjustment of the dose. In contrast to gabapentin, pregabalin has linear and dose proportion absorption in therapeutic dose range (150 to 600 mg/d). It also has rapid onset of action and more limited dose range.[4] Similar to gabapentin, it is also not metabolized and is almost entirely excreted unchanged in the urine. It is not bound to plasma proteins and has virtually no drug–drug interaction, again resembling the characteristics of gabapentin. Similarly, other drugs do not affect the pharmacokinetics of pregabalin. The half-life of pregabalin ranges from approximately 4.5 hour to 7.0 hours, thus, requiring more than once daily dosing in most patients.[4]
Dosing
The initial dosage of gabapentin is 300 mg/d and can be increased up to 1200 mg three times a day.[5],[6] It can be started at its effective dose rather than gradually titrated upwards in dosage.[7] It should not be discontinued abruptly, but rather tapered gradually, because it can lead to withdrawal-related side-effects.[8] It has a high toxicity ratio, minimizing the chance of adverse effects with even very high overdoses,[9] hence, routine monitoring of clinical laboratory parameters is not required.[5] Pregabalin is started at an initial dose of 150 mg/d and can be increased up to 600 mg/d.[10]
Clinical Uses
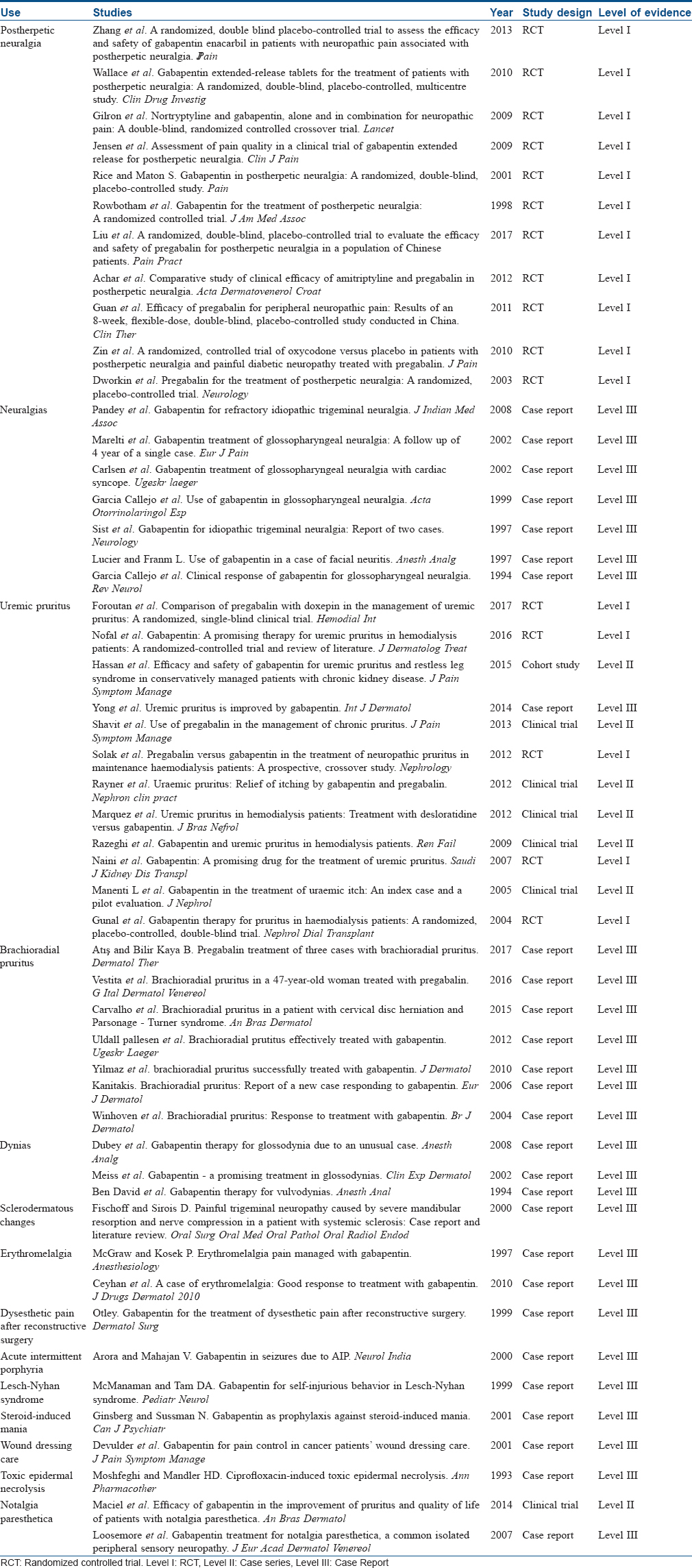
Postherpetic neuralgia and other similar neuropathies
Approximately 10–15% of herpes zoster patients will develop postherpetic neuralgia, which can persist for many years. Dermatologists are often the primary care providers for postherpetic neuralgia patients. Several trials conducted previously reported statistically significant reduction in average daily pain after gabapentin and pregabalin.[11],[12],[13],[14],[15],[16],[17] Gabapentin is the first oral medication approved in the USA for this condition.[5] Reviews of controlled studies showed that patients suffering from postherpetic neuralgia experienced a statistically significant reduction in average daily pain after treatment with gabapentin. The study also showed that those receiving gabapentin experienced improvement in sleep and overall quality of life.[11] Gabapentin is useful in the treatment of neuralgia in all areas of the body [Table - 1]. Its positive effect on neuralgia includes trigeminal neuralgia,[18] glossopharyngeal neuralgia refractory to the usual medical treatments[19] and facial neuritis.[20] It is also useful in treating inflammatory pain.[21] Gabapentin is also effective in the treatment of human immunodeficiency virus (HIV) neuropathy,[22] painful diabetic neuropathy[23] and diabetic neuropathic pain.[24] Of particular interest to dermatologist is the probable usefulness of this drug in decreasing the trophic ulcerations that results from neuropathy in diseases such as HIV, leprosy and diabetes that are prone to such ulcers.[5] Pregabalin is found to be efficacious in treating Red scrotum syndrome (poorly understood, chronic dysesthetic erythema primarily involving the anterior scrotum).[25]
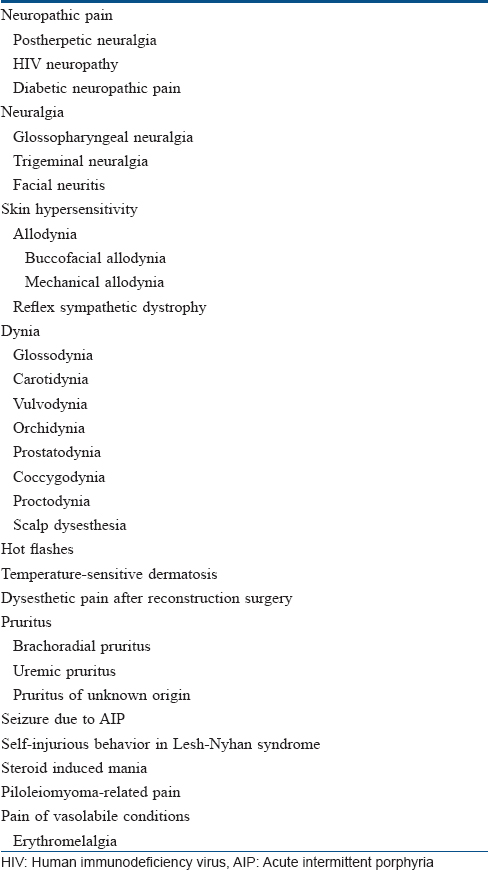
Pruritus
Generalized pruritus is a distressing symptom that can occur in several dermatologic and systemic disorders. Strong similarities exist between neural induction, transmission and processing of pruritus and pain. While itch is transmitted by a functionally distinct subset of neurons, overlap exists between the mediators and receptors involved in the pathogenesis of these sensations.[26] In addition, it is now clear that chronic itch is influenced by a phenomenon of neural hypersensitization in a process that parallels what has been observed in chronic pain.[27] In the wake of these discoveries, agents that target the neural system have emerged as effective antipruritic therapies.[28] Gabapentin has been reported to be an effective antipruritic agent in uremic pruritus,[29],[30],[31],[32],[33],[34],[35],[36] brachioradial pruritus,[9],[37],[38],[39],[40] pruritus associated with wound healing in burns[41] and notalgia paresthetica[42] and pruritus of unknown origin.[6],[43] Its effect in pruritus can be central and peripheral. It inhibits voltage-dependent calcium ion channels located in the spinal cord (with particular high density in the superficial laminae of the dorsal horn), inhibiting the release of excitatory neurotransmitters. Other mechanisms involved are increase in the synthesis of γ-aminobutyric acid from glutamate by altering the activity of glutamic acid decarboxylase in neurological tissue,[44] inhibition of the release of calcitonin gene-related peptide, a neuropeptide, described as an itch mediator.[45] Gabapentin also increases the threshold to experience nociception.[46] Related drug Pregabalin, a gamma amino butyric acid analogue of gabapentin, has been used in the treatment of uremic pruritus,[47],[48],[49],[50] brachioradial pruritus,[51],[52] pruritus in prurigo nodularis[53] and polycythemia vera-associated aquagenic pruritus.[54] It was hypothesized that the beneficial effect of Pregabalin in chronic pruritus may result from counteracting the effects on the central sensitizing processes involved in the generation of chronic itch.[55] It has also been reported to improve interleukin 2[56] and cetuximab-related[57] pruritus in cancer patients. However, at present there are insufficient data to conclude that these anticonvulsants can be an effective therapeutic alternative in the management of pruritus.
Gabapentin in various dynias
The “dynias” are a group of chronic, focal pain syndromes with a predilection for the orocervical and urogenital regions. They include glossodynia, carotidynia, scalp dysesthesia, vulvodynia, orchidynia, prostatodynia, coccygodynia and proctodynia [Table - 1].[5] In some cases, the dynia occur secondarily, but more often, despite an exhaustive evaluation, no etiology is found, and in these cases the cause of pain remains enigmatic. Sometimes, these patients initially present to dermatologist. These dynias are found responsive to gabapentin. Allodynia is a sensation of pain to slight touch. It is another complication of postherpetic neuralgia. It can be effectively treated by gabapentin which can block both the static and dynamic components of mechanical allodynia.[58] It also relieves cutaneous hyperalgesia after skin has been sensitized to pain.[58] Reflex sympathetic dystrophy is a condition involving persistent pain that results from nerve injury. It has a variety of cutaneous manifestations, including atrophy, edema, erythema, bullae, and ulcers.[59] Gabapentin has a role in the control of reflex sympathetic dystrophy-related pain in children[60] and adults.[61]
Other uses
Gabapentin has shown benefit in pain related to leiomyomas[5] in patients with painful sclerodermatous changes that have affected nerve conduction,[62] pain of the vasolabile condition and erythromelalgia.[63],[64] Gabapentin has also shown benefits in various conditions associated with neurologic problems and skin. It is useful in the treatment of dysesthetic pain after reconstructive surgery,[65] seizures due to acute intermittent porphyria,[66] self-injurious behavior in Lesch-Nyhan syndrome[67] and as a prophylaxis against steroid-induced mania.[68] Finally, gabapentin improves pain control during wound dressing of cancer patients,[69] suggesting that it might have a role in toxic epidermal necrolysis patients who complain of “painful skin.”[70] In a recent article, gabapentin was also found to be effective for Vismodegib-induced muscle cramps.[71] Pregabalin was also used for the treatment of painful hand-foot skin reaction associated with darafenib.[72] Studies showing effect of gabapentin and pregabalin in various dermatological conditions have been described briefly in [Table - 2].
Adverse Effects
These drugs are relatively safe with very few serious adverse effects [Table - 3]. The most frequently reported adverse event is drowsiness/sedation. This is seen during the first month of treatment.[5] This is also one of the most common cause for discontinuation of the drug.[6] Others causes include dizziness, malaise/lassitude and ataxia.
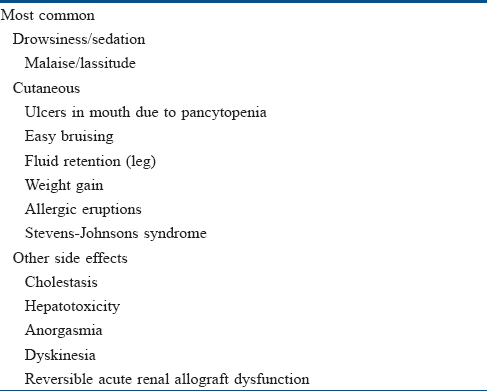
Rarely, they can cause pancytopenia, causing fever, sore throat and ulcers in the mouth, or unusual bleeding and easy bruising, fluid retention in the legs and weight gain.[5],[6] A few cases of allergic eruptions[73] and Stevens–Johnson's syndrome[74] have also been reported.
Very rarely gabapentin has induced cholestasis[75] and hepatotoxicity.[76] Studies conducted for its efficacy in pregnancy showed no congenital anomalies among the infants. However, the crude mortality rate was up to five times higher than in the general population.[77] There are a few isolated reports about anorgasmia in women taking gabapentin.[78]
Conclusion
Gabapentin and pregabalin are very promising medications in the treatment of painful conditions that often are domain of dermatologists such as postherpetic neuralgia, painful tumors, neuropathic ulcers or pain during dressing changes in conditions such as toxic epidermal necrolysis. Of great interest to a dermatologist is its use in chronic itch unresponsive to other medication. However, at present, there is insufficient data to suggest that these anticonvulsants can be an effective alternative to treat various types of skin sensitivities and pruritus. Future large randomized controlled studies are required that use behavioral methodology rather than subjective methodology. The chances of placebo effects are quite high with subjective methodologies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
MacNamara JO. Pharmacotherapy of the epileptics. In: Brunton LL, editor. Goodman & Gilman's the Pharmacological Basis of Therapeutics. 12th ed. China: McGraw-Hill Companies; 2011. p. 583-607.
[Google Scholar]
|
| 2. |
Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN, et al. The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem 1996;271:5768-76.
[Google Scholar]
|
| 3. |
Field MJ, Cox PJ, Stott E, Melrose H, Offord J, Su TZ, et al. Identification of the alpha2-delta-1 subunit of voltage-dependent calcium channels as a molecular target for pain mediating the analgesic actions of pregabalin. Proc Natl Acad Sci U S A 2006;103:17537-42.
[Google Scholar]
|
| 4. |
Porter RJ, Meldrum BS. Antiseizuer drug gabapentin and pregabalin. In: Katzung BG, Masters SB, Trevar AJ, editors. Basic and Clinical Pharmacology. 12th ed. New Delhi: Tata McGraw-Hill; 2012. p. 403-27.
[Google Scholar]
|
| 5. |
Scheinfeld N. The role of gabapentin in treating diseases with cutaneous manifestations and pain. Int J Dermatol 2003;42:491-5.
[Google Scholar]
|
| 6. |
Yesudian PD, Wilson NJ. Efficacy of gabapentin in the management of pruritus of unknown origin. Arch Dermatol 2005;141:1507-9.
[Google Scholar]
|
| 7. |
Ferrendelli JA. Concerns with antiepileptic drug initiation: Safety, tolerability, and efficacy. Epilepsia 2001;42 Suppl 4:28-30.
[Google Scholar]
|
| 8. |
Norton JW. Gabapentin withdrawal syndrome. Clin Neuropharmacol 2001;24:245-6.
[Google Scholar]
|
| 9. |
Winhoven SM, Coulson IH, Bottomley WW. Brachioradial pruritus: Response to treatment with gabapentin. Br J Dermatol 2004;150:786-7.
[Google Scholar]
|
| 10. |
US Food and Drug Administration. Lyrica (Pregabalin) full Prescribing Information.
[Google Scholar]
|
| 11. |
Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: A randomized controlled trial. JAMA 1998;280:1837-42.
[Google Scholar]
|
| 12. |
Rice AS, Maton S; Postherpetic Neuralgia Study Group. Gabapentin in postherpetic neuralgia: A randomised, double blind, placebo controlled study. Pain 2001;94:215-24.
[Google Scholar]
|
| 13. |
Dworkin RH, Corbin AE, Young JP Jr., Sharma U, LaMoreaux L, Bockbrader H, et al. Pregabalin for the treatment of postherpetic neuralgia: A randomized, placebo-controlled trial. Neurology 2003;60:1274-83.
[Google Scholar]
|
| 14. |
Zin CS, Nissen LM, O'Callaghan JP, Duffull SB, Smith MT, Moore BJ, et al. Arandomized, controlled trial of oxycodone versus placebo in patients with postherpetic neuralgia and painful diabetic neuropathy treated with pregabalin. J Pain 2010;11:462-71.
[Google Scholar]
|
| 15. |
Guan Y, Ding X, Cheng Y, Fan D, Tan L, Wang Y, et al. Efficacy of pregabalin for peripheral neuropathic pain: Results of an 8-week, flexible-dose, double-blind, placebo-controlled study conducted in China. Clin Ther 2011;33:159-66.
[Google Scholar]
|
| 16. |
Athanasakis K, Petrakis I, Karampli E, Vitsou E, Lyras L, Kyriopoulos J, et al. Pregabalin versus gabapentin in the management of peripheral neuropathic pain associated with post-herpetic neuralgia and diabetic neuropathy: A cost effectiveness analysis for the Greek healthcare setting. BMC Neurol 2013;13:56.
[Google Scholar]
|
| 17. |
Liu Q, Chen H, Xi L, Hong Z, He L, Fu Y, et al. Arandomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of pregabalin for postherpetic neuralgia in a population of Chinese patients. Pain Pract 2017;17:62-9.
[Google Scholar]
|
| 18. |
Sist T, Filadora V, Miner M, Lema M. Gabapentin for idiopathic trigeminal neuralgia: Report of two cases. Neurology 1997;48:1467.
[Google Scholar]
|
| 19. |
García Callejo FJ, Marco Algarra J, Talamantes Escribá F, Martínez Beneyto MP, Esparcia Navarro M, Morant Ventura A, et al. Use of gabapentin in glossopharyngeal neuralgia. Acta Otorrinolaringol Esp 1999;50:175-7.
[Google Scholar]
|
| 20. |
Lucier E, Franm L. Use of gabapentin in a case of facial neuritis. Anesth Analg 1997;85:1410.
[Google Scholar]
|
| 21. |
Werner MU, Perkins FM, Holte K, Pedersen JL, Kehlet H. Effects of gabapentin in acute inflammatory pain in humans. Reg Anesth Pain Med 2001;26:322-8.
[Google Scholar]
|
| 22. |
Newshan G. HIV neuropathy treated with gabapentin. AIDS 1998;12:219-21.
[Google Scholar]
|
| 23. |
Porta-Etessam J, García-Morales I, Martínez-Salio A, Berbel A, Benito-León J. Gabapentin in acute painful diabetic neuropathy. Eur J Neurol 2000;7:365.
[Google Scholar]
|
| 24. |
Pérez HE, Sánchez GF. Gabapentin therapy for diabetic neuropathic pain. Am J Med 2000;108:689.
[Google Scholar]
|
| 25. |
Miller J, Leicht S. Pregabalin in the treatment of red scrotum syndrome: A report of two cases. Dermatol Ther 2016;29:244-8.
[Google Scholar]
|
| 26. |
Roberson DP, Gudes S, Sprague JM, Patoski HA, Robson VK, Blasl F, et al. Activity-dependent silencing reveals functionally distinct itch-generating sensory neurons. Nat Neurosci 2013;16:910-8.
[Google Scholar]
|
| 27. |
Ikoma A, Steinhoff M, Ständer S, Yosipovitch G, Schmelz M. The neurobiology of itch. Nat Rev Neurosci 2006;7:535-47.
[Google Scholar]
|
| 28. |
Vinik AI. Clinical practice. Diabetic sensory and motor neuropathy. N Engl J Med 2016;374:1455-64.
[Google Scholar]
|
| 29. |
Gunal AI, Ozalp G, Yoldas TK, Gunal SY, Kirciman E, Celiker H, et al. Gabapentin therapy for pruritus in haemodialysis patients: A randomized, placebo-controlled, double-blind trial. Nephrol Dial Transplant 2004;19:3137-9.
[Google Scholar]
|
| 30. |
Manenti L, Vaglio A, Costantino E, Danisi D, Oliva B, Pini S, et al. Gabapentin in the treatment of uremic itch: An index case and a pilot evaluation. J Nephrol 2005;18:86-91.
[Google Scholar]
|
| 31. |
Naini AE, Harandi AA, Khanbabapour S, Shahidi S, Seirafiyan S, Mohseni M, et al. Gabapentin: A promising drug for the treatment of uremic pruritus. Saudi J Kidney Dis Transpl 2007;18:378-81.
[Google Scholar]
|
| 32. |
Razeghi E, Eskandari D, Ganji MR, Meysamie AP, Togha M, Khashayar P, et al. Gabapentin and uremic pruritus in hemodialysis patients. Ren Fail 2009;31:85-90.
[Google Scholar]
|
| 33. |
Marquez D, Ramonda C, Lauxmann JE, Romero CA, Vukelic VL, Martinatto C, et al. Uremic pruritus in hemodialysis patients: Treatment with desloratidine versus gabapentin. J Bras Nefrol 2012;34:148-52.
[Google Scholar]
|
| 34. |
Yong AS, Lee KY. Uremic pruritus is improved by gabapentin. Int J Dermatol 2014;53:e404-5.
[Google Scholar]
|
| 35. |
Cheikh Hassan HI, Brennan F, Collett G, Josland EA, Brown MA. Efficacy and safety of gabapentin for uremic pruritus and restless legs syndrome in conservatively managed patients with chronic kidney disease. J Pain Symptom Manage 2015;49:782-9.
[Google Scholar]
|
| 36. |
Nofal E, Farag F, Nofal A, Eldesouky F, Alkot R, Abdelkhalik Z, et al. Gabapentin: A promising therapy for uremic pruritus in hemodialysis patients: A randomized-controlled trial and review of literature. J Dermatolog Treat 2016;27:515-9.
[Google Scholar]
|
| 37. |
Kanitakis J. Brachioradial pruritus: Report of a new case responding to gabapentin. Eur J Dermatol 2006;16:311-2.
[Google Scholar]
|
| 38. |
Yilmaz S, Ceyhan AM, Baysal Akkaya V. Brachioradial pruritus successfully treated with gabapentin. J Dermatol 2010;37:662-5.
[Google Scholar]
|
| 39. |
Uldall Pallesen KA, Bygum A. Brachioradial pruritus effectively treated with gabapentin. Ugeskr Laeger 2012;174:1830-1.
[Google Scholar]
|
| 40. |
Carvalho S, Sanches M, Alves R, Selores M. Brachioradial pruritus in a patient with cervical disc herniation and parsonage-turner syndrome. An Bras Dermatol 2015;90:401-2.
[Google Scholar]
|
| 41. |
Mendham JE. Gabapentin for the treatment of itching produced by burns and wound healing in children: A pilot study. Burns 2004;30:851-3.
[Google Scholar]
|
| 42. |
Maciel AA, Cunha PR, Laraia IO, Trevisan F. Efficacy of gabapentin in the improvement of pruritus and quality of life of patients with notalgia paresthetica. An Bras Dermatol 2014;89:570-5.
[Google Scholar]
|
| 43. |
Park JM, Jwa SW, Song M, Kim HS, Ko HC, Kim MB, et al. Efficacy and safety of pregabalin for the treatment of chronic pruritus in Korea. J Dermatol 2012;39:790-1.
[Google Scholar]
|
| 44. |
Bennett MI, Simpson KH. Gabapentin in the treatment of neuropathic pain. Palliat Med 2004;18:5-11.
[Google Scholar]
|
| 45. |
Fehrenbacher JC, Taylor CP, Vasko MR. Pregabalin and gabapentin reduce release of substance P and CGRP from rat spinal tissues only after inflammation or activation of protein kinase C. Pain 2003;105:133-41.
[Google Scholar]
|
| 46. |
Gustafsson H, Flood K, Berge OG, Brodin E, Olgart L, Stiller CO, et al. Gabapentin reverses mechanical allodynia induced by sciatic nerve ischemia and formalin-induced nociception in mice. Exp Neurol 2003;182:427-34.
[Google Scholar]
|
| 47. |
Solak Y, Biyik Z, Atalay H, Gaipov A, Guney F, Turk S, et al. Pregabalin versus gabapentin in the treatment of neuropathic pruritus in maintenance haemodialysis patients: A prospective, crossover study. Nephrology (Carlton) 2012;17:710-7.
[Google Scholar]
|
| 48. |
Shavit L, Grenader T, Lifschitz M, Slotki I. Use of pregabalin in the management of chronic uremic pruritus. J Pain Symptom Manage 2013;45:776-81.
[Google Scholar]
|
| 49. |
Foroutan N, Etminan A, Nikvarz N, Shojai Shahrokh Abadi M. Comparison of pregabalin with doxepin in the management of uremic pruritus: A randomized single blind clinical trial. Hemodial Int 2017;21:63-71.
[Google Scholar]
|
| 50. |
Vestita M, Cerbone L, Calista D. Brachioradial pruritus in a 47-year-old woman treated with pregabalin. G Ital Dermatol Venereol 2016;151:727-8.
[Google Scholar]
|
| 51. |
Atış G, Bilir Kaya B. Pregabalin treatment of three cases with brachioradial pruritus. Dermatol Ther 2017;30:e12459.
[Google Scholar]
|
| 52. |
Yue J, Jiao S, Xiao Y, Ren W, Zhao T, Meng J, et al. Comparison of pregabalin with ondansetron in treatment of uraemic pruritus in dialysis patients: A prospective, randomized, double-blind study. Int Urol Nephrol 2015;47:161-7.
[Google Scholar]
|
| 53. |
Mazza M, Guerriero G, Marano G, Janiri L, Bria P, Mazza S, et al. Treatment of prurigo nodularis with pregabalin. J Clin Pharm Ther 2013;38:16-8.
[Google Scholar]
|
| 54. |
Ehrchen J, Ständer S. Pregabalin in the treatment of chronic pruritus. J Am Acad Dermatol 2008;58:S36-7.
[Google Scholar]
|
| 55. |
Ebrchen J, Stander S. Pregabalin: A new neuropathic disorder. Clin Neurol Neurosurg 2006;108:803-5.
[Google Scholar]
|
| 56. |
Lee SH, Baig M, Rusciano V, Dutcher JP. Novel management of pruritus in patients treated with IL-2 for metastatic renal cell carcinoma and malignant melanoma. J Immunother 2010;33:1010-3.
[Google Scholar]
|
| 57. |
Porzio G, Aielli F, Verna L, Porto C, Tudini M, Cannita K, et al. Efficacy of pregabalin in the management of cetuximab-related itch. J Pain Symptom Manage 2006;32:397-8.
[Google Scholar]
|
| 58. |
Dirks J, Petersen KL, Rowbotham MC, Dahl JB. Gabapentin suppresses cutaneous hyperalgesia following heat-capsaicin sensitization. Anesthesiology 2002;97:102-7.
[Google Scholar]
|
| 59. |
Sundaram S, Webster GF. Vascular diseases are the most common cutaneous manifestations of reflex sympathetic dystrophy. J Am Acad Dermatol 2001;44:1050-1.
[Google Scholar]
|
| 60. |
Tong HC, Nelson VS. Recurrent and migratory reflex sympathetic dystrophy in children. Pediatr Rehabil 2000;4:87-9.
[Google Scholar]
|
| 61. |
Mellick GA, Mellick LB. Reflex sympathetic dystrophy treated with gabapentin. Arch Phys Med Rehabil 1997;78:98-105.
[Google Scholar]
|
| 62. |
Fischoff DK, Sirois D. Painful trigeminal neuropathy caused by severe mandibular resorption and nerve compression in a patient with systemic sclerosis: Case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:456-9.
[Google Scholar]
|
| 63. |
McGraw T, Kosek P. Erythromelalgia pain managed with gabapentin. Anesthesiology 1997;86:988-90.
[Google Scholar]
|
| 64. |
Ceyhan AM, Gurses I, Yildirim M, Akkaya VB. A case of erythromelalgia: Good response to treatment with gabapentin. J Drugs Dermatol 2010;9:565-7.
[Google Scholar]
|
| 65. |
Otley CC. Gabapentin for the treatment of dysesthetic pain after reconstructive surgery. Dermatol Surg 1999;25:487-8.
[Google Scholar]
|
| 66. |
Arora A, Mahajan V. Gabapentin in seizures due to acute intermittent porphyria. Neurol India 2000;48:194-5.
[Google Scholar]
|
| 67. |
McManaman J, Tam DA. Gabapentin for self-injurious behavior in Lesch-Nyhan syndrome. Pediatr Neurol 1999;20:381-2.
[Google Scholar]
|
| 68. |
Ginsberg DL, Sussman N. Gabapentin as prophylaxis against steroid-induced mania. Can J Psychiatry 2001;46:455-6.
[Google Scholar]
|
| 69. |
Devulder J, Lambert J, Naeyaert JM. Gabapentin for pain control in cancer patients' wound dressing care. J Pain Symptom Manage 2001;22:622-6.
[Google Scholar]
|
| 70. |
Moshfeghi M, Mandler HD. Ciprofloxacin-induced toxic epidermal necrolysis. Ann Pharmacother 1993;27:1467-9.
[Google Scholar]
|
| 71. |
Caliskan E, Taşçı Ï, Bek S. Gabapentin for the management of vismodegib-induced muscle cramps. Indian J Dermatol Venereol Leprol 2017;83:505-6.
[Google Scholar]
|
| 72. |
Lilly E, Burke M, Kluger H, Choi J. Pregabalin for the treatment of painful hand-foot skin reaction associated with dabrafenib. JAMA Dermatol 2015;151:102-3.
[Google Scholar]
|
| 73. |
Available from: http://www.med.umich.edu/1libr/prescrpt/epil12.htm#side. [Last accessed on 2002 Oct 13].
[Google Scholar]
|
| 74. |
DeToledo JC, Minagar A, Lowe MR, Ramsay RE. Skin eruption with gabapentin in a patient with repeated AED-induced Stevens-Johnson's syndrome. Ther Drug Monit 1999;21:137-8.
[Google Scholar]
|
| 75. |
Richardson CE, Williams DW, Kingham JG. Gabapentin induced cholestasis. BMJ 2002;325:635.
[Google Scholar]
|
| 76. |
Lasso-de-la-Vega MC, Zapater P, Such J, Pérez-Mateo M, Horga JF. Gabapentin-associated hepatotoxicity. Am J Gastroenterol 2001;96:3460-2.
[Google Scholar]
|
| 77. |
Wilton LV, Shakir S. A postmarketing surveillance study of gabapentin as add-on therapy for 3,100 patients in England. Epilepsia 2002;43:983-92.
[Google Scholar]
|
| 78. |
Grant AC, Oh H. Gabapentin-induced anorgasmia in women. Am J Psychiatry 2002;159:1247.
[Google Scholar]
|
Fulltext Views
11,778
PDF downloads
3,471





