Translate this page into:
Flexural scaly papules and plaques
Correspondence Address:
Arun C Inamadar
Department of Dermatology, Venereology and Leprosy, SBMP Medical College, Hospital and Research Center, BLDE University, Bijapur - 586 103, Karnataka
India
| How to cite this article: Adya KA, Inamadar AC, Palit A. Flexural scaly papules and plaques. Indian J Dermatol Venereol Leprol 2018;84:703-705 |
A 16-year-old female presented with slightly erythematous scaly papules involving both the axillae since the past 3 months. The lesions were episodically pruritic precipitated by sweating on exertion or warm weather. In addition, she had similar lesions involving both the cubital fossae and groins. There was no personal or family history of atopy. The lesions were predominantly discrete papules but had coalesced at places to form plaques with fine scaling [[Figure - 1], black circle]. The lesions partially remitted with topical agents (self-medicated by the patient) but never completely healed. Rest of the cutaneous examination was unremarkable. A potassium hydroxide preparation of the scales did not show any fungal elements. A discretely located scaly papule was biopsied for histopathological analysis [Figure - 2] and [Figure - 3].
 |
| Figure 1: Erythematous papules involving the left axilla with fine adherent scaling |
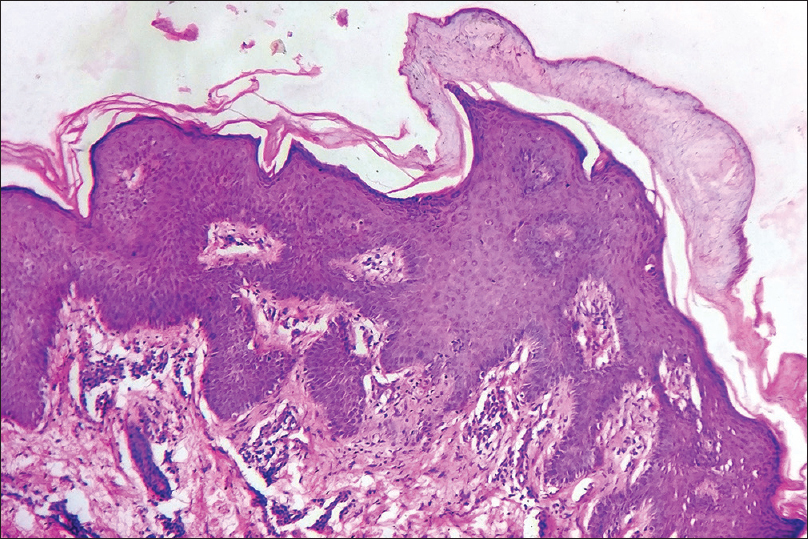 |
| Figure 2: Compact parakeratosis, epidermal hyperplasia, and dermal perivascular infiltrate is seen at lower magnification. Note the prominent granular layer (H and E, ×100) |
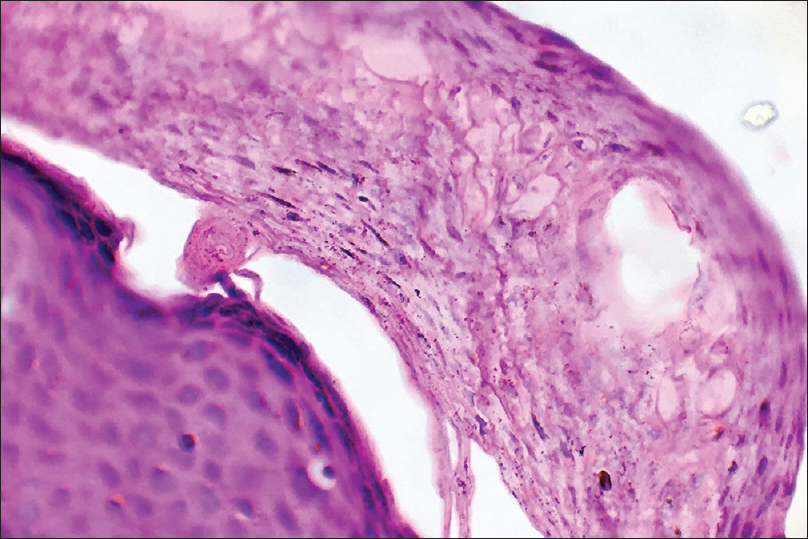 |
| Figure 3: Higher magnification of the epidermis shows compact parakeratotic stratum corneum with retention of keratohyalin granules within the cells and a prominent stratum granulosum (H and E, ×400) |
What is Your Diagnosis?
Answer
Granular parakeratosis.
Discussion
Granular parakeratosis (intertriginous granular parakeratosis, zombie patch) is an uncommon acquired pruritic disorder of the flexures. It was first described by Northcutt et al. in 1991 as “axillary granular parakeratosis.” It affects all ages and both sexes, although a slight female preponderance is noted. Involvement of other flexures and nonflexural areas has also been described.[1] Typical lesions are itchy and erythematous to brownish keratotic scaly papules that may coalesce into verrucous plaques. The exact etiopathogenesis of granular parakeratosis is unclear. The disorder is possibly an irritant response to antiperspirants, deodorants, and excessive use of soaps and creams. However, the current consensus is that such agents aggravate but do not induce granular parakeratosis.[2] Recent studies have assigned this entity to the group of acquired keratinization disorders as a defect in the processing of profilaggrin to filaggrin impairing the normal cornification process demonstrated previously.[3] Hoste et al. observed that mice deficient in caspase-14 (a vital enzyme necessary for the formation of an adequately functional epidermal barrier) were more prone to develop parakeratosis than control mice. Exploring this phenomenon in humans may help unravel the exact etiopathogenesis of granular parakeratosis.[4] Co-occurrence of dermatophytosis and granular parakeratosis that responded effectively to antifungal treatment has been reported, suggesting the possible role of fungi in the disease.[5] Hence, histopathological analysis should also include periodic acid Schiff and Giemsa staining to examine fungal elements.
Histopathology shows compact parakeratosis, psoriasiform epidermal hyperplasia, and the pathognomonic retention of keratohyaline granules within areas of parakeratosis with persistent granular layer. The process may also involve follicular and eccrine ostia.[6]
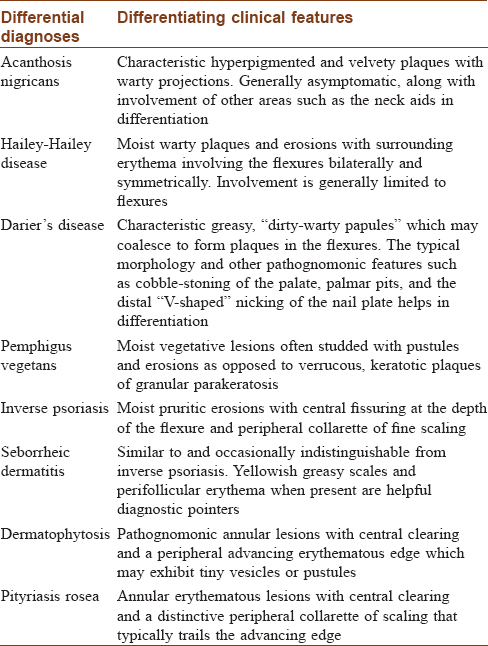
Treatment options include topical steroids, topical calcipotriol, topical calcineurin inhibitors, and ammonium lactate. Oral isotretinoin is useful in refractory cases.[7] Spontaneous resolution, as well as relapse after treatment are not uncommon. An infantile form, attributed to diaper wearing, has been described which may present in one of the two forms – linear bilateral keratotic plaques in the inguinal folds and erythematous geographical plaques underneath pressure points.[8] Our patient was treated satisfactorily with topical tacrolimus 0.1% ointment. Granular parakeratosis resembles a host of other flexural dermatoses [Table - 1]; hence, Ding et al. suggested reappraisal of this disorder merely as a reaction pattern rather than a distinct condition.[9]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Joshi R, Taneja A. Granular parakeratosis presenting with facial keratotic papules. Indian J Dermatol Venereol Leprol 2008;74:53-5.
[Google Scholar]
|
| 2. |
Southwell B, Lockshin BN, Blyumin ML, Khachemoune A. What Caused These Axillary Changes? Available from: http://www.the-dermatologist.com/content/what-caused-these-axillary-changes. [Last accessed on 2017 Apr 22].
[Google Scholar]
|
| 3. |
Scheinfeld NS, Mones J. Granular parakeratosis: Pathologic and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol 2005;52:863-7.
[Google Scholar]
|
| 4. |
Hoste E, Denecker G, Gilbert B, Van Nieuwerburgh F, van der Fits L, Asselbergh B, et al. Caspase-14-deficient mice are more prone to the development of parakeratosis. J Invest Dermatol 2013;133:742-50.
[Google Scholar]
|
| 5. |
Resnik KS, Kantor GR, DiLeonardo M. Dermatophyte-related granular parakeratosis. Am J Dermatopathol 2004;26:70-1.
[Google Scholar]
|
| 6. |
Weedon D, editor. Disorders of epidermal maturation and keratinization. In: Weedon's Skin Pathology. 3rd ed. Edinburgh: Churchill Livingstone Elsevier; 2010. p. 248-79.
[Google Scholar]
|
| 7. |
Compton AK, Jackson JM. Isotretinoin as a treatment for axillary granular parakeratosis. Cutis 2007;80:55-6.
[Google Scholar]
|
| 8. |
Chang MW, Kaufmann JM, Orlow SJ, Cohen DE, Mobini N, Kamino H. Infantile granular parakeratosis: Recognition of two clinical patterns. J Am Acad Dermatol 2004;50 5 Suppl: S93-6.
[Google Scholar]
|
| 9. |
Ding CY, Liu H, Khachemoune A. Granular parakeratosis: A comprehensive review and a critical reappraisal. Am J Clin Dermatol 2015;16:495-500.
[Google Scholar]
|
Fulltext Views
5,593
PDF downloads
1,506





