Translate this page into:
Differential expression of capecitabine-induced hand foot syndrome on paretic limb
Correspondence Address:
Bhabani ST P Singh
Department of Dermatology, IMS and SUM Hospital, Bhubaneswar, Odisha
India
| How to cite this article: Tripathy T, P Singh BS, Behera D, Kar BR. Differential expression of capecitabine-induced hand foot syndrome on paretic limb. Indian J Dermatol Venereol Leprol 2018;84:720-722 |
Sir,
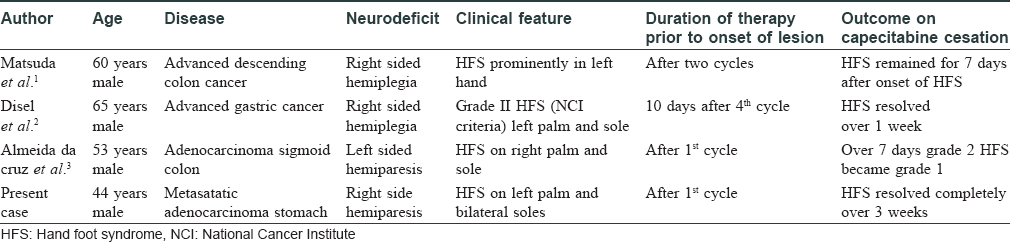
Hand foot syndrome is a localized toxic reaction seen secondary to several chemotherapeutic drugs such as capecitabine, pegylated doxorubicin, 5 fluorouracil, cytarabine, docetaxel, sorafenib and sunitinib. It is manifested by painful erythema over palms and soles. Blistering and erosions may accompany depending upon clinical severity. The pathogenesis of this entity is not well understood. Atypical presentations such as involvement of scar sites, scrotum and penis have been reported, the reports hypothesizing different mechanisms for this toxic event. We found few reports of hand foot syndrome sparing the hemiplegic side [Table - 1].[1],[2],[3] Here, we report a case of capecitabine-induced hand foot syndrome with differential severity expressed on the paretic limb.
A 44-year-old man of type IV skin, known to be suffering from right-sided hemiparesis, who was diagnosed with metastatic adenocarcinoma of stomach, was initiated on chemotherapy with palliative intent. He received four cycles of docetaxel and oxaliplatin once every 14 days. No cutaneous side effects were observed during this period. Due to disease progression despite therapy, the patient was prescribed capecitabine 750 mg/sq m orally twice daily in addition to the above drugs. After 15 days of capecitabine intake, the patient developed sudden burning sensation and pain over both palms and soles. In the subsequent two days, he developed erythema followed by hyperpigmentation over bilateral soles and left palm. Strikingly, the patient's right hand was spared from the cutaneous changes. A bulla developed on the dorsum of the left hand with subsequent spontaneous rupture. The patient was unable to perform his routine activities due to severe pain. He gave history of identical and symmetrical sweating from his palms and soles prior to initiation of chemotherapy. He was a known hypertensive for the past five years. Over these years, there was near complete gain of motor power in his right lower limb. However, muscle power of his right upper limb did not improve.
On examination, well-demarcated erythematous to hyperpigmented, tender patches were seen symmetrically over the convexities of bilateral soles. The concave parts were spared [Figure - 1]. The left hand showed hyperpigmentation covering the entire palm as well as the dorsum. There was a large ruptured bulla with a necrotic base of approximate size 4 × 4 sq cm on the dorsum of the left hand [Figure - 2]. Nails were spared. The patient also had mucositis in the oral cavity. All the muscles of the right hand had grade 1 power as revealed by voluntary muscle testing. There was no miosis, ptosis or anhidrosis in any part of the body, as seen in Horner syndrome. Sweat test could not be performed as the patient became sick and was shifted to the intensive care unit. Nerve conduction study of the upper and lower limb nerves revealed mild decrease in compound muscle action potential in right median and ulnar nerve with normal sensory nerve action potential. Total erythrocyte count and total leukocyte count was 3.5 million/dl and 4,000/dl, respectively. There was thrombocytopenia with platelet count of 10,000/dl. The patient had deranged hepatic function test with liver enzymes raised three times above baseline. Based on history and clinical examination, a diagnosis of hand foot syndrome was made. His Naranjo causality score was 4. Capecitabine was stopped and the lesions improved over the next 2–3 weeks.
 |
| Figure 1: Erythematous to hyperpigmented patches over the bilateral soles and left palm |
 |
| Figure 2: Hyperpigmentation with ruptured bulla over the dorsum of left hand with sparing of right hand |
The index case had differential degree of severity on both hands. The paretic limb had grade 1 hand foot syndrome, whereas the other limb had grade 4 severity according to the World Health Organization criteria.
The pathogenesis of capecitabine-induced hand foot syndrome is poorly understood. Direct release of the drug into the skin via the eccrine ducts, causing toxic injury is one pathomechanism explaining this event.[4] Increased thymidine phosphorylase enzyme activity converting capecitabine to the more toxic 5-fluorouracil and free radical-induced damage have also been proposed. Abnormal regulation of the autonomic nervous system has been known to occur after a cerebrovascular accident. The cortical and subcortical inhibitory effects on vasomotor neurons are reduced. This increases the vessel wall tone, thereby reducing temperature and cutaneous blood flow to the paretic side.[5] This could be a possible cause for the finding in our case. The relative less use of the paretic hand in comparison to the other hand and feet for daily activities could also be responsible for the differential presentation in our patient. All previous reports of unilateral hand foot syndrome are from western literature. We were unable to find any such reports from India. The findings in our case highlights the neural and vascular mechanism contributing to the pathogenesis of hand foot syndrome in contrast to the commonly accepted mechanism of it being caused by secretion of the drug in the sweat into palms and soles.
Avoidance of strenuous activities, involving friction over the palms and soles, e.g. long walking, lifting objects and using ill-fitting footwear, could reduce the severity of this reaction. Physicians should be aware that patients on drugs causing hand foot syndrome and coexisting neurological disease might manifest the same in an atypical manner. Future studies exploring neural pathomechanisms mediating hand foot syndrome should be undertaken.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Matsuda S, Koketsu H, Hayakawa M, Nagata N. Unilateral capecitabine-related hand-foot syndrome. Intern Med 2015;54:2779.
[Google Scholar]
|
| 2. |
Disel U, Gürkut O, Abali H, Kaleağasi H, Mertsoylu H, Ozyilkan O, et al. Unilateral hand-foot syndrome: An extraordinary side effect of capecitabine. Cutan Ocul Toxicol 2010;29:140-2.
[Google Scholar]
|
| 3. |
Almeida da Cruz L, Hoff PM, Ferrari CL, Riechelmann RS. Unilateral hand-foot syndrome: Does it take sides? Case report and literature review. Clin Colorectal Cancer 2012;11:82-4.
[Google Scholar]
|
| 4. |
Miller KK, Gorcey L, McLellan BN. Chemotherapy-induced hand-foot syndrome and nail changes: A review of clinical presentation, etiology, pathogenesis, and management. J Am Acad Dermatol 2014;71:787-94.
[Google Scholar]
|
| 5. |
Al-Qudah ZA, Yacoub HA, Souayah N. Disorders of the autonomic nervous system after hemispheric cerebrovascular disorders: An update. J Vasc Interv Neurol 2015;8:43-52.
[Google Scholar]
|
Fulltext Views
3,142
PDF downloads
1,294





