Translate this page into:
Cutaneous epithelioid hemangioendothelioma: A rare presentation
Correspondence Address:
S Rekha
Department of Dermatology, Venereology and Leprosy, Dr. S N Medical College, Jodhpur, Rajasthan
India
| How to cite this article: Kumar V, Kachhawa D, Rekha S, Jain V. Cutaneous epithelioid hemangioendothelioma: A rare presentation. Indian J Dermatol Venereol Leprol 2018;84:739-742 |
Sir,
Epithelioid hemangioendothelioma is a rare malignant tumor of vascular endothelial origin. Initially, it was described as a tumor of intermediate malignant potential, but recently it has been classified as a neoplasm with full malignant potential.[1] It usually arises in the superficial and deep soft tissues, liver, lung, bones and muscles of the extremities. Underlying bone tumors are commonly associated with cutaneous epithelioid hemangioendotheliomas. Skin-limited epithelioid hemangioendothelioma is an extremely rare entity, with less than 15 cases reported worldwide. To the best of the authors' knowledge, this is first such case being reported in India.
A 15-year-old man from Jodhpur presented with a 6-month history of an asymptomatic, gradually enlarging mass on the margin of the left external nares. There was no history of pain, itching, epistaxis, eye pain, nasal obstruction, breathing difficulty or anosmia.
On examination, the 6 × 5 cm mass had a proximal firm verrucous portion, extending 1 cm into the left nasal cavity, and a distal hard indurated part that extended until the margin of the upper lip [Figure - 1]. There was no clinical evidence of spread into the nasopharynx, paranasal sinuses or attachment to underlying bone or soft tissue. Routine examinations including hemogram, liver and renal function tests and urine examination were within normal limits. Scintigraphy and computed tomography did not reveal any connection to the underlying bone. Imaging studies of the chest, abdomen and pelvis did not reveal any distant metastases.
 |
| Figure 1: Partly verrucous, partly indurated mass on the margin of the left external nares |
Clinically, based on the long standing history and indurated appearance of the lesion, numerous differential diagnoses were suspected. Deep mycotic infection, cutaneous leishmaniasis, cutaneous tuberculosis (tuberculosis verrucosa cutis), sarcoidosis, cutaneous lymphoma, verrucous angioma and other vascular tumors were included in the differential diagnoses.
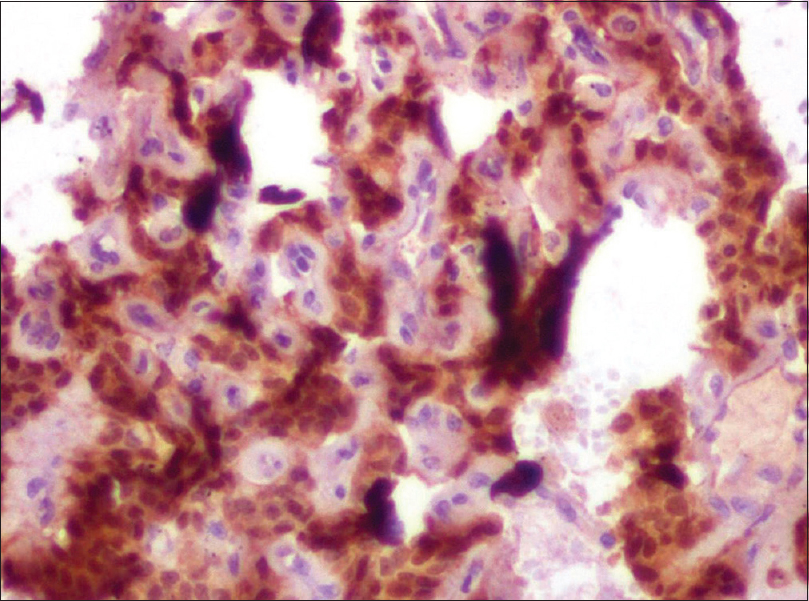
Two punch biopsies were taken, one each from verrucous and indurated regions and the histopathology revealed diffuse infiltration by the tumor cells up till the deep dermis. On higher magnification, expanded sinusoids lined by large epithelioid tumor cells [Figure - 2] and occasional mitotic figures were seen. Not only were tumor cells seen within sinusoids, but single cells and small group of cells were seen embedded within the stroma [Figure - 3]. No well-formed vascular channels were seen. Occasional intracytoplasmic erythrocytes were also seen.
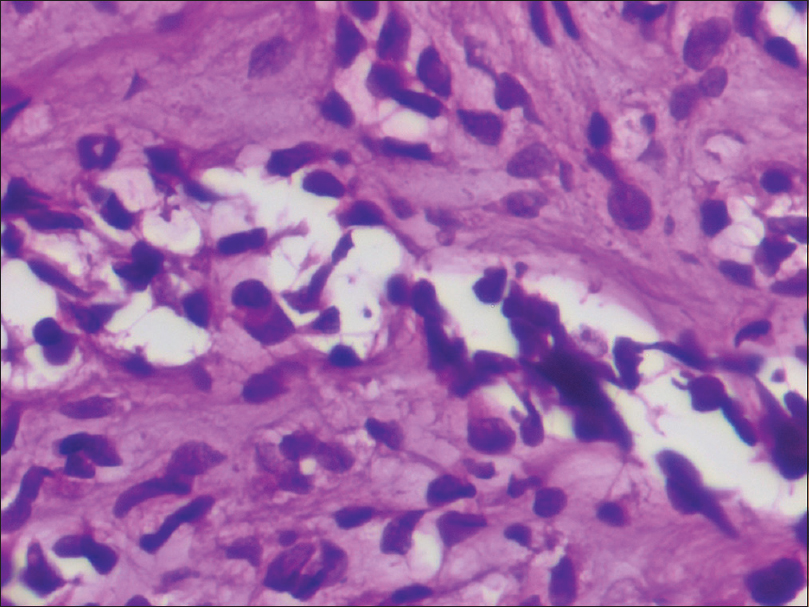 |
| Figure 2: Expanded sinusoids lined by large epithelioid tumor cells (hematoxylin and eosin, ×400) |
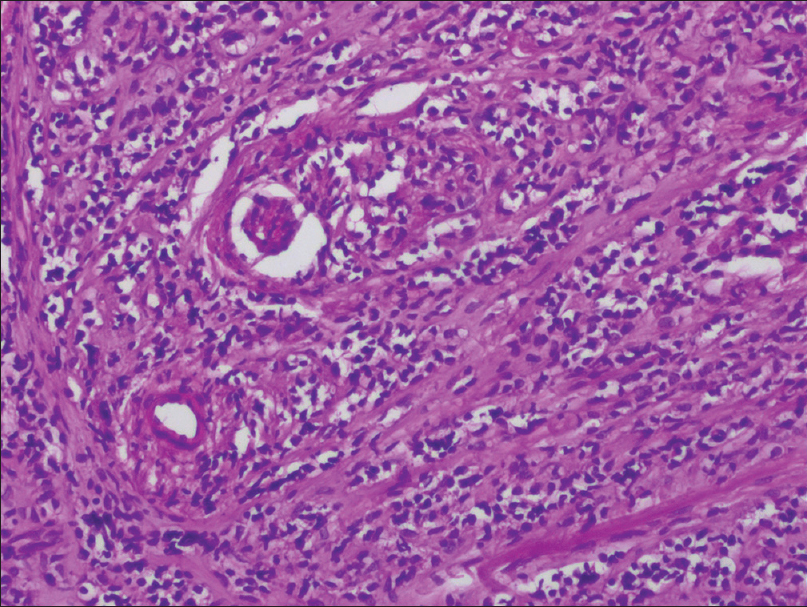 |
| Figure 3: Tumor cells within the sinusoids as well as single and small group of cells embedded within the stroma (hematoxylin and eosin, ×100) |
On immunohistochemistry, the tumor cells stained positive for CD31, CD34 and Fli-1 [Figure - 4], [Figure - 5], [Figure - 6]. Histological and immunohistochemical findings led to the diagnosis of epithelioid hemangioendothelioma. The patient was referred to surgery department for further follow-up and treatment.
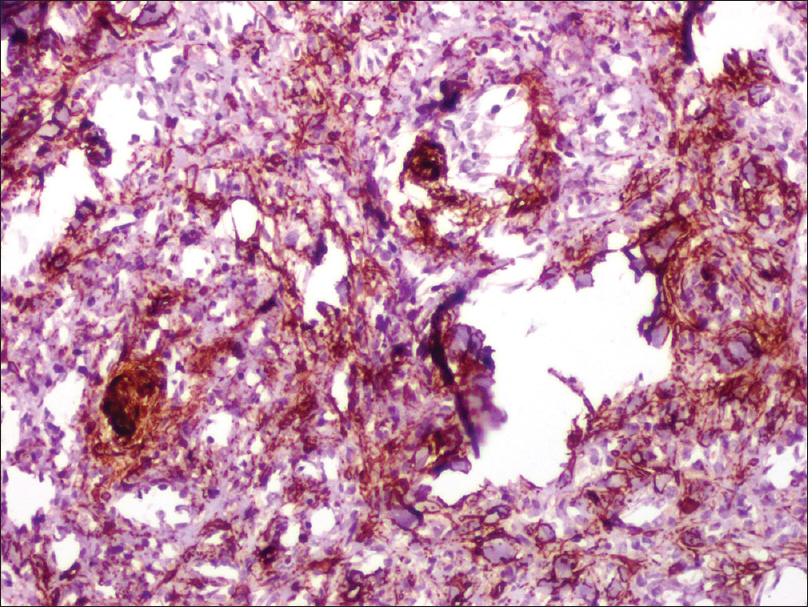 |
| Figure 4: CD31 positive staining of tumor cells, in typical sinusoidal pattern |
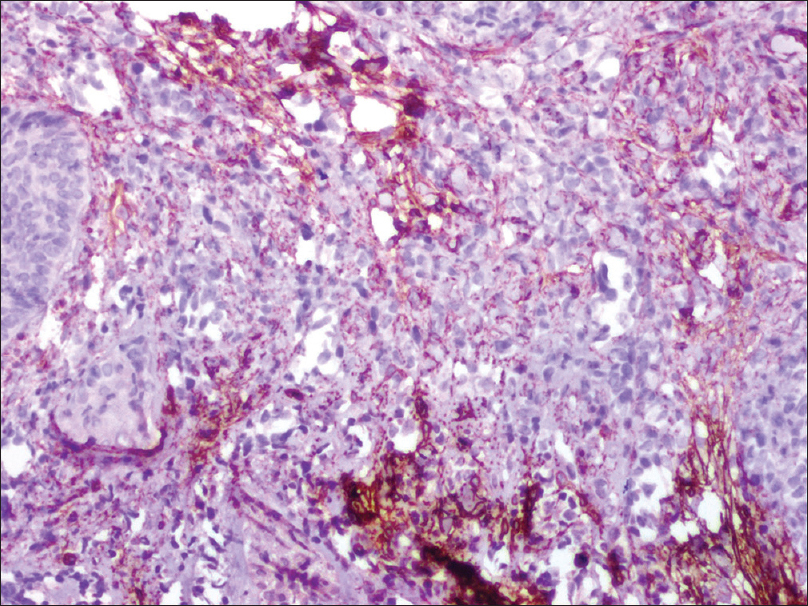 |
| Figure 5: Tumor cells staining positive for CD34 |
 |
| Figure 6: Tumor cells are nuclear positive for Fli-1 with immunohistochemical staining |
Epithelioid hemangioendothelioma is a rare vascular tumor of full malignant potential[1] that was first described by Dail and Liebow in 1975 as an aggressive bronchoalveolar cell carcinoma.[2] In 1982, Weiss and Enzinger described 41 cases in a series published in 1982.[3] The prevalence of epithelioid hemangioendothelioma has been estimated to be less than 1 case per million.[4] Epithelioid hemangioendothelioma most frequently presents in the liver, lungs and bones, while skin-limited epithelioid hemangioendothelioma is an exceedingly rare occurrence. Dissemination can be hematogenous or via lymphatics, and the most frequent sites of metastases include the liver and bones.[4]
Both sexes are affected equally. Cytogenetic studies have shown the role of a reciprocal translocation t(1;3)(p36.3;q25) resulting in a fusion gene WWTR1-CAMTA1.[4] A recent hypothesis has suggested the role of chronic bartonella infection in the pathogenesis of epithelioid hemangioendothelioma.[4] Cutaneous epithelioid hemangioendothelioma may present as a solitary erythematous mass, multiple dome-shaped masses or dermal nodules over the extremities. It may also present as a nonhealing ulcer or a scar.[5],[6],[7]
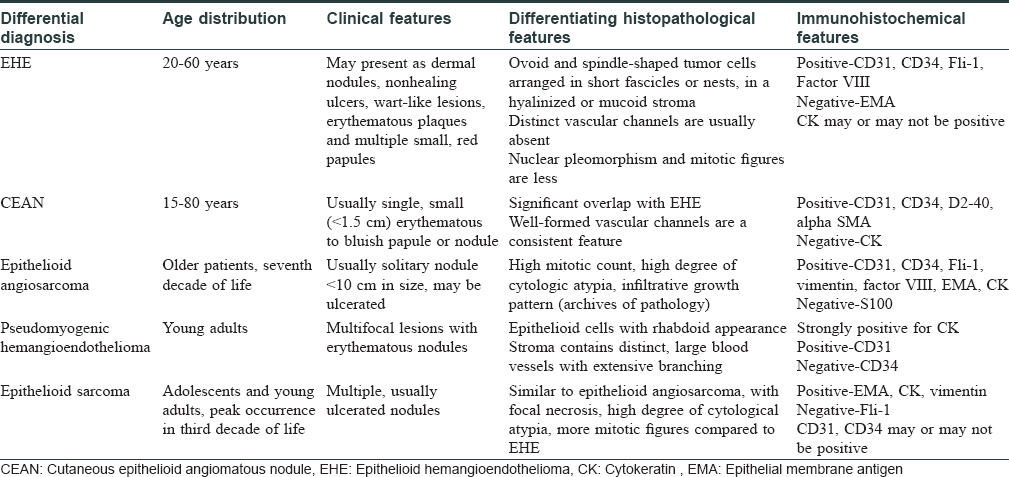
Histopathologically, it shows ovoid and spindle-shaped tumor cells with eosinophilic cytoplasm. The cells are arranged in short fascicles or nests, in a hyalinized or mucoid stroma. Distinct vascular channels are usually absent, but intracytoplasmic vacuoles with occasional erythrocytes are considered as a characteristic feature. Nuclear pleomorphism and mitotic figures are less or absent.[1] Histopathological differentials and their differentiating features have been tabulated in [Table - 1].[8],[9],[10]
Epithelioid hemangioendothelioma is notorious for high rates of infiltrative growth, and the prognosis is uncertain.[5] The recurrence rate of epithelioid hemangioendothelioma has been reported to range from 10 to 15%, and the rate of lymphatic and systemic metastasis has been reported to be between 20 and 30%.[5]
Imaging studies are a must to rule out tumor extension to underlying bone or soft tissue as the prognosis of skin-limited epithelioid hemangioendothelioma seems better than systemic epithelioid hemangioendothelioma, or cutaneous epithelioid hemangioendothelioma with underlying soft tissue/bone involvement.
Simple surgical excision is the mainstay of treatment. Mohs micrographic surgery has been used in a single case with good cosmetic outcome.[5]
Carboplatin plus etoposide, interferon 2, azathioprine, mesna, doxorubicin, ifosfamide, dacarbazine regimen, bevacizumab and nanoparticle albumin-bound paclitaxel (nab-paclitaxel) have shown variable benefit in systemic epithelioid hemangioendothelioma, but their role in skin-limited epithelioid hemangioendothelioma is debatable, where complete surgical excision is feasible. Radiotherapy has shown to be of limited use, due to the slow growth rate of the tumor.[4]
We report this case due to its extreme rarity and unusual site of presentation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Vascular tumors: Tumors and tumor-like conditions of blood vessels and lymphatics. In: Lever's Histopathology of the Skin. 10th ed. Philadelphia: Wolters Kluwer; 2009. p. 1039-42.
[Google Scholar]
|
| 2. |
Dail DH, Liebow AA. Intravascular bronchioloalveolar tumor. Am J Pathol 1975;78:6a-7a.
[Google Scholar]
|
| 3. |
Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer 1982;50:970-81.
[Google Scholar]
|
| 4. |
Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M. Epithelioid hemangioendothelioma: An overview and update on a rare vascular tumor. Oncol Rev 2014;8:259.
[Google Scholar]
|
| 5. |
Park SM, Kim HS, Ko HC, Kim BS, Kim MB, Mun JH. Cutaneous epithelioid hemangioendothelioma treated with Mohs micrographic surgery. Int J Dermatol 2017;56:97-9.
[Google Scholar]
|
| 6. |
Kikuchi K, Watanabe M, Terui T, Ohtani N, Ohtani H, Tagami H. Nail-destroying epithelioid haemangioendothelioma showing an erythematous scar-like appearance on the finger. Br J Dermatol 2003;148:834-6.
[Google Scholar]
|
| 7. |
Forschner A, Harms D, Metzler G, Sönnichsen K, Ulmer A, Rassner G, et al. Ulcerated epithelioid hemangioendothelioma of the foot in childhood. J Am Acad Dermatol 2003;49:113-6.
[Google Scholar]
|
| 8. |
Mobini N. Cutaneous epithelioid angiosarcoma: A neoplasm with potential pitfalls in diagnosis. J Cutan Pathol 2009;36:362-9.
[Google Scholar]
|
| 9. |
Requena L, Kutzner H. Hemangioendothelioma. Semin Diagn Pathol 2013;30:29-44.
[Google Scholar]
|
| 10. |
Hart J, Mandavilli S. Epithelioid angiosarcoma: A brief diagnostic review and differential diagnosis. Arch Pathol Lab Med 2011;135:268-72.
[Google Scholar]
|
Fulltext Views
4,205
PDF downloads
1,423





