Translate this page into:
Transepidermal elimination: Historical evolution, pathogenesis and nosology
2 Department of Dermatology, Government Medical College and Hospital, Haldwani, Uttarakhand, India
3 Department of Dermatology, Katihar Medical College, Katihar, Bihar, India
Correspondence Address:
Piyush Kumar
Katihar Medical College, Katihar, Bihar
India
| How to cite this article: Shah H, Tiwary AK, Kumar P. Transepidermal elimination: Historical evolution, pathogenesis and nosology. Indian J Dermatol Venereol Leprol 2018;84:753-757 |
Introduction
Dermoepidermal junction is the most complex structural and functional microscopic zone of the skin that enables both epidermal and dermal units to interact in many complex ways in order to perform various functions. Elimination of exogenous foreign substances or altered dermal constituents from dermis to the skin surface via epidermal channel is one of the functions of this zone which has been the mainstay in the pathogenesis of various perforating dermatoses.
Historical Aspects
The first case of perforating dermatosis was described by Josef Kyrle[1] in 1916 who termed it as “hyperkeratosis follicularis et parafollicularis in cutem penetrans.” In 1927, Fisher[2] described a patient with circinate papular eruption on neck containing perforating amorphous plugs but he did not elaborate further and considered it as an atypical presentation of what Kyrle had described before. The phenomenon of expulsion of such materials via epidermis was first observed in detail by Freudenthal[3] in 1930 who identified it as amyloid in his own case. In the subsequent years, many such cases were reported and then in 1958, the term “elastosis perforans serpiginosa” was given for a particular variant of perforating disorder by Dammert and Putkonen.[4] Mehregan[5] also described a similar perforating disorder and coined them as “reactive perforating collagenosis.” In 1968, Mehregan described a series of 11 cases of “elastosis perforans serpiginosa” and based on such descriptions, he first proposed the concept of “transepidermal elimination” in 1970.[6],[7]
Definition
Transepidermal elimination is a purposeful, pathologic, dermoepidermal reactive phenomenon incited by exogenous substances or altered dermal constituents (of inflammatory, metabolic or neoplastic origin) and characterized by pseudoepitheliomatous hyperplasia of epidermis and/or follicular epithelium and formation of multiple transepithelial perforating channels, facilitating the extrusion of the altered dermal material or foreign substances to the exterior.
Concept of Transepidermal Elimination and Pathogenesis
During the conceptual formulation of transepidermal elimination, Mehregan described three types of epidermal reaction to foreign materials in the dermis.[7] Those were:
- Type 1 reaction that includes the trapping and upward epidermal migration and desquamation of “inert particles” or “nonmotile cells” such as hemosiderin or amyloid and erythrocytes, respectively, which are not capable of eliciting sufficient dermal reaction.
- Type 2 reaction that involves migration of microorganisms and motile cells such as Treponema pallidum and leukocytes into the epidermal spaces to be carried upward with physiological desquamation process.
-
The above two, being relatively passive processes with the absence of specific dermoepidermal reaction, have collectively been termed as “transmigration.” Of note, by definition transepidermal elimination is an active process of elimination of dermal foreign materials, hence these two are not included under the nosology of transepidermal elimination.
- There is a third type of dermoepidermal interaction which is an active and unidirectional elimination process whereby dermal altered material and foreign components (e.g. calcium, collagen, elastin) are actively extruded out through the epidermis. This is called “transepidermal elimination”.
Without going into the detail of each example of transepidermal elimination, the sequence of pathological events can be generalized and summarized. It starts with the binding of foreign or altered dermal constituents to a receptor which is still unidentified. It incites a dermal reaction releasing some chemical mediators leading to epidermal hyperplasia and formation of multiple transepidermal perforating channels. The foreign substances get surrounded and phagocytosed by the epidermal cells of these perforating channels and are subsequently moved upward to the surface.[8] Recently, the receptor for advanced glycation endproducts has been suggested to play a role in the pathogenesis of acquired reactive perforating collagenosis by modulating the collagen–keratinocyte interaction and keratinocyte migration.[9]
Some authors have described yet another type of transepidermal elimination where necrotic and altered dermal material gets incorporated in the follicular lumen, followed by slow elimination to the surface. This process is the hallmark of perforating folliculitis, but may also be seen in infective and noninfective granulomatous conditions such as lupus vulgaris and Jorge Lobo's disease (through infundibular epithelium), respectively.[10],[11]
Of note, the process of transepidermal elimination has also been reported to occur through eccrine duct opening in one case of cutaneous leishmaniasis in human immunodeficiency virus (HIV) positive patient wherein amastigotes were found within the epithelial cells of secretory eccrine glands and ducts indicating the feasibility of elimination through eccrine duct opening.[12]
Prerequisites
There are two chief prerequisites for transepidermal elimination. These are:
Nature of the inciting dermal stimulus
Stimulus should not be very irritant, otherwise epidermal necrosis would occur. Neither should it be inert, or else there would be no dermal reaction. Hence, stimulus should be irritant enough to induce inflammation and reactive hyperplasia of epidermis without any major structural alteration or necrosis.[13]
Location of the dermal stimulus
According to the previous literature experiences, the foreign dermal stimulus cannot lead to transepidermal elimination unless that stimulus is located within a specific dermal–epidermal interaction zone that is “above the level of the hair papillae” in the dermis.[14] More superficial or deeper location of the stimulus will not result in transepidermal elimination.
Nosology
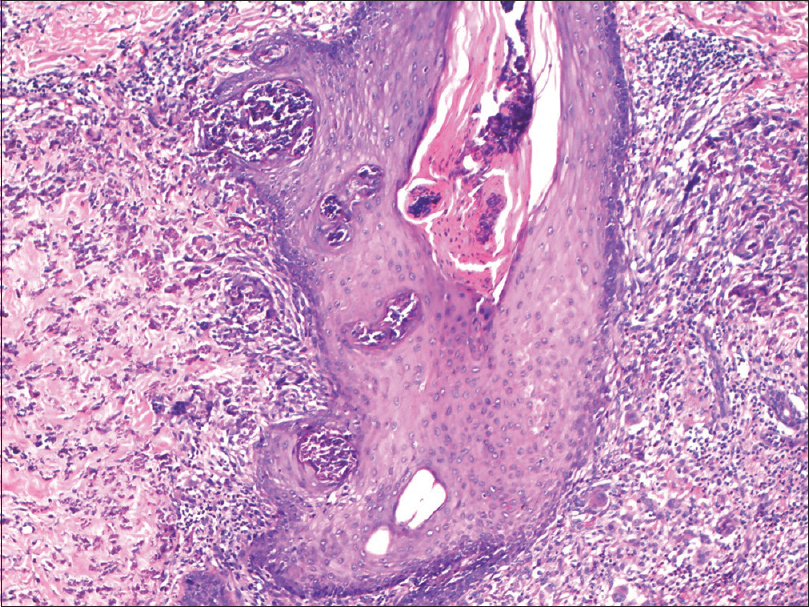
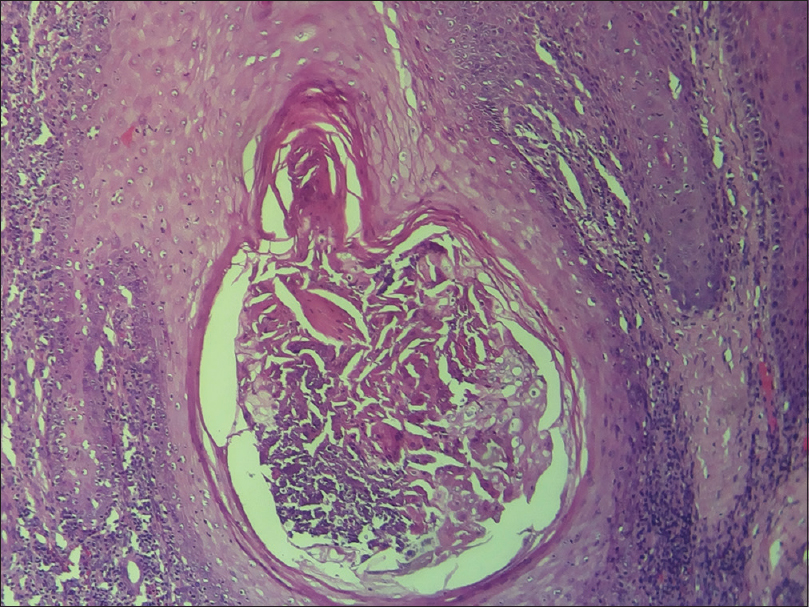
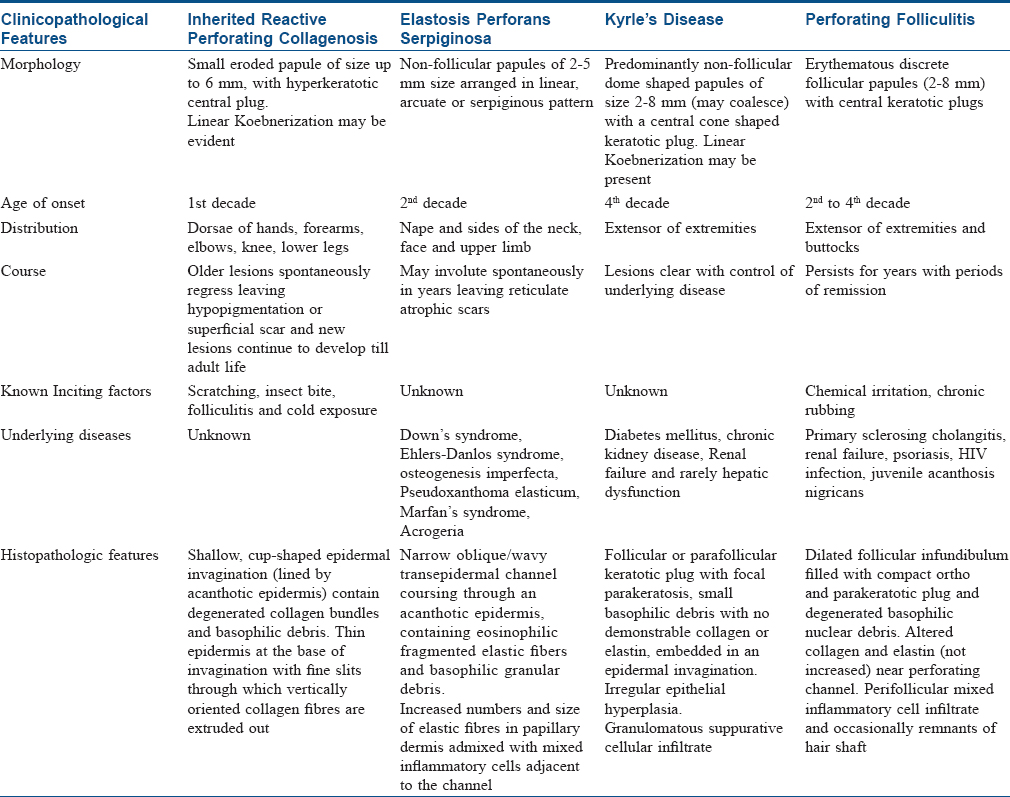
All perforating dermatoses exhibiting transepidermal elimination characteristically present with a common clinical morphology: umbilicated papules with central hyperkeratotic plug [Figure - 1] and unique histopathologic findings. Depending on the presence or absence of preexisting dermatosis, disorders of transepidermal elimination are broadly classified into two categories:[14] primary perforating dermatoses including elastosis perforans serpiginosa and reactive perforating collagenosis (inherited form), and secondary forms appearing in preexisting disorders. This extended classification has now been condensed to four classical entities based on the primary defect and nature of extruding dermal foreign substances (identified by proper staining and histopathologic examination): Reactive perforating collagenosis, Kyrle's disease, elastosis perforans serpiginosa and perforating folliculitis [Figure - 2], [Figure - 3], [Figure - 4], [Figure - 5], [Figure - 6], [Figure - 7] and [Table - 1].
 |
| Figure 1: Multiple umbilicated papules with central keratotic material in a case of acquired perforating dermatosis associated with diabetic mellitus |
 |
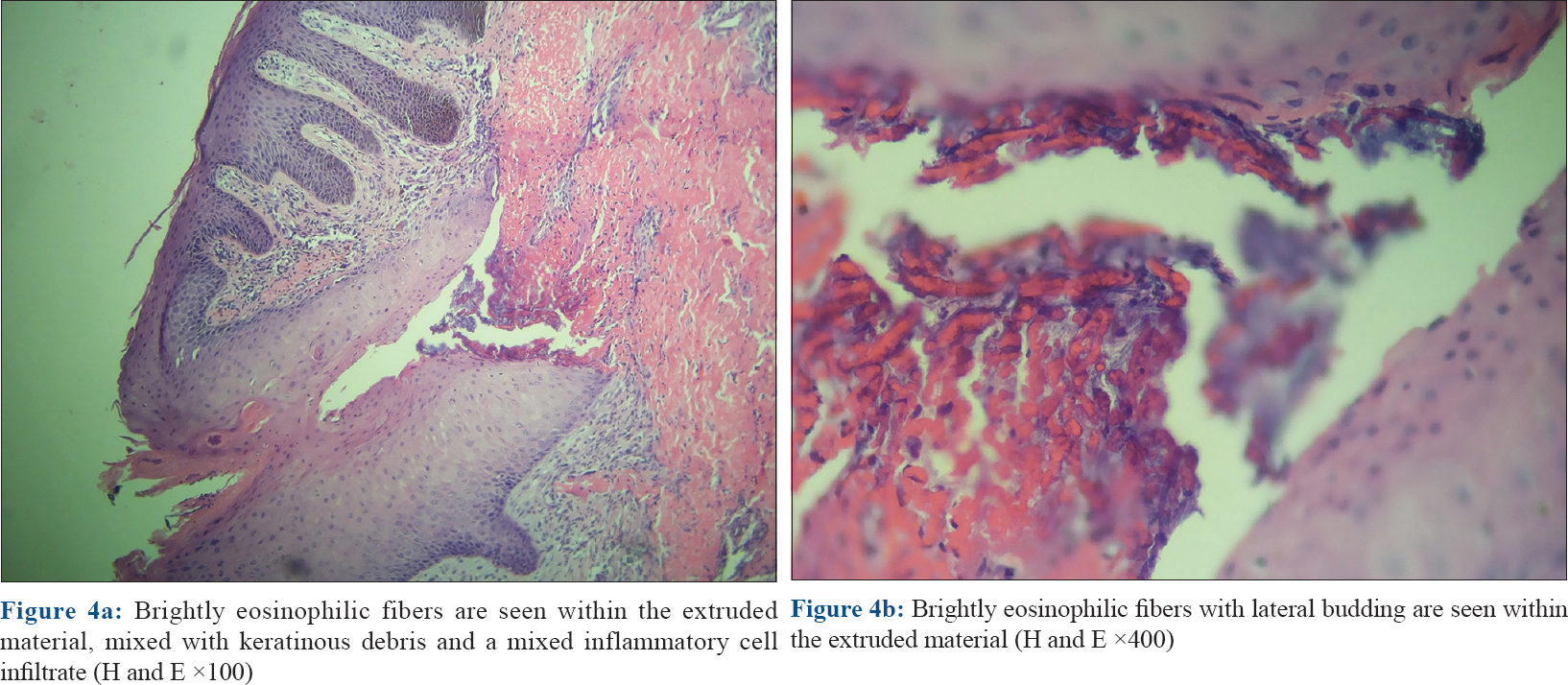
| Figure 2: A cup-shaped channel containing degenerated collagen bundles and inflammatory debris [hematoxylin and eosin (H and E) ~100] |
 |
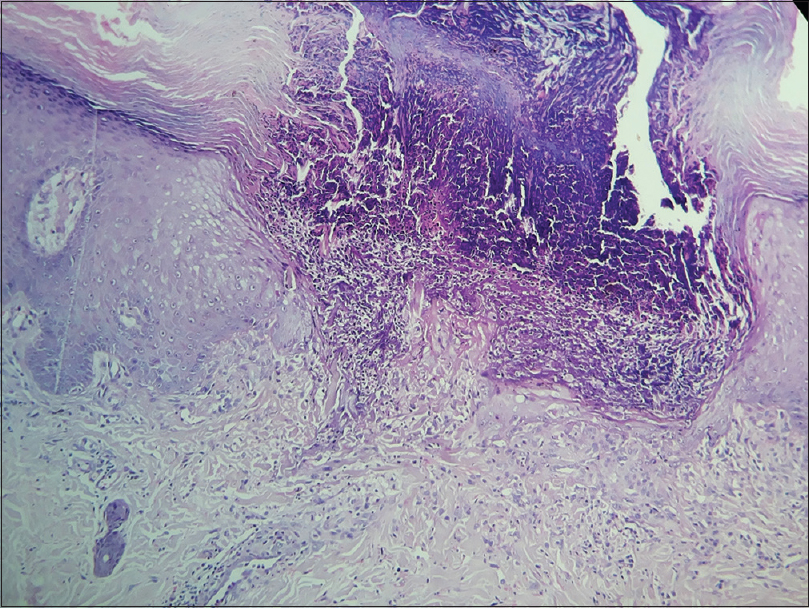
| Figure 3: |
 |
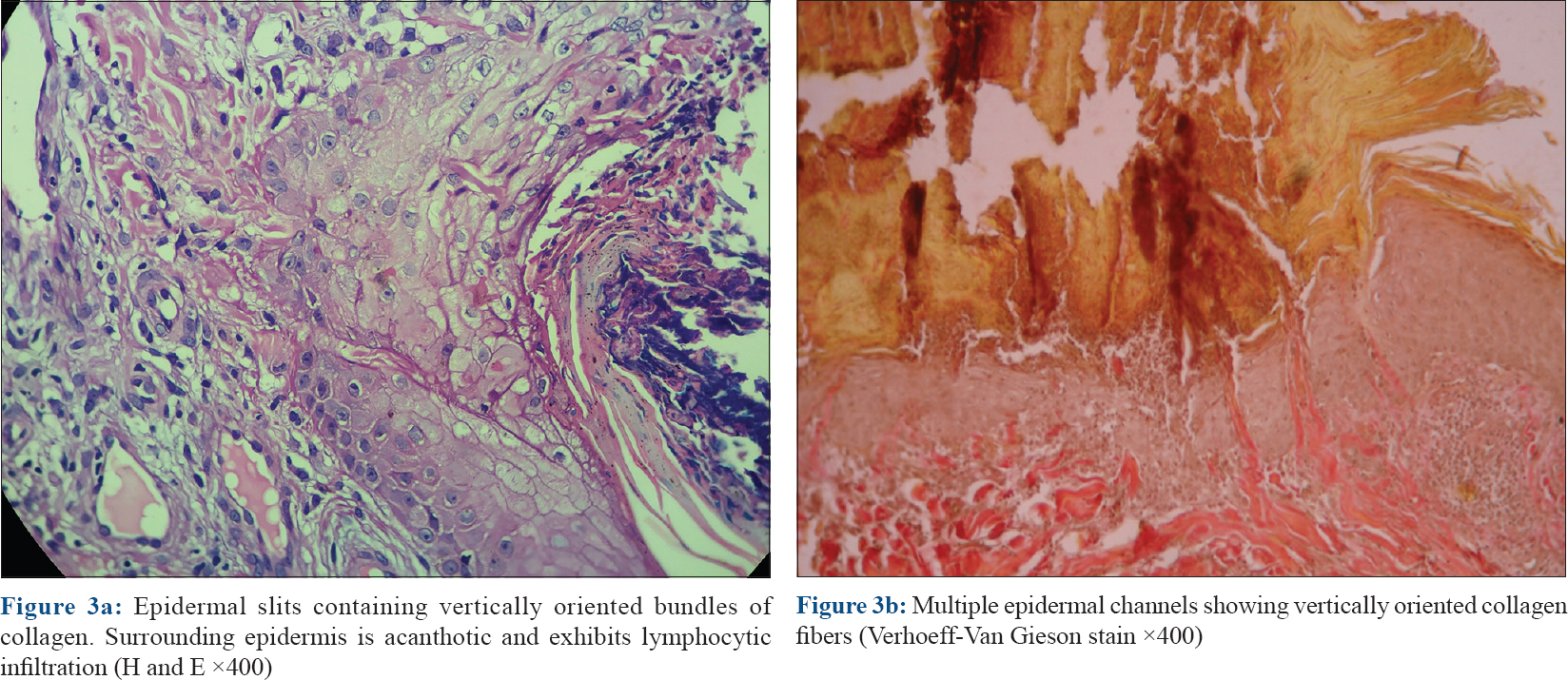
| Figure 4: |
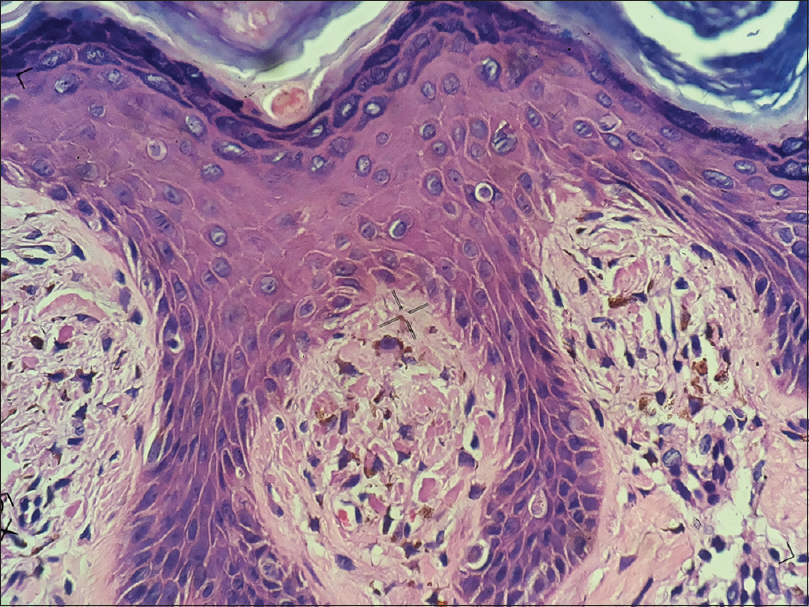 |
| Figure 5: Uniformly stained pink globules occupying the dermal papilla. Overlying epidermis is acanthotic. Similar eosinophilic globule seen at the junction of granular layer n corneal layer (H and E ×400) |
 |
| Figure 6: Short fragmented basophilic fibers mixed with inflammatory cells seen extruding epidermis (H and E ×400) |
 |
| Figure 7: Granulomatous infiltration engulfed by follicular unit in tuberculosis verrucosa cutis (H and E ×400) |
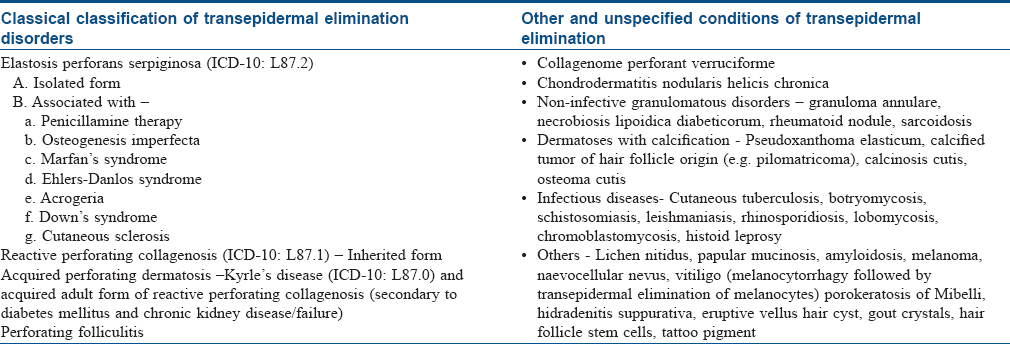
Clinical and histopathologic features of these four perforating conditions have been summarized in [Table - 2].[15]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Joseph D, Papali C, Pisharody R. Kyrle's disease: a cutaneous marker of renal disorder. Indian J Dermatol Venereol Leprol 1996;62:222-5.
[Google Scholar]
|
| 2. |
Polańska A, Bowszyc-Dmochowska M, Żaba RW, Adamski Z, Reich A, Dańczak-Pazdrowska A. Elastosis perforans serpiginosa: a review of the literature and our own experience. Postepy Dermatol Alergol 2016;33(5):392-95.
[Google Scholar]
|
| 3. |
Eng AM, Mandrea E. Peforating calcinosis cutis presenting as milia. J Cutan Pathol 1981;8(3):247-50.
[Google Scholar]
|
| 4. |
Dammert K, Putkonen T. Keratosis follicularis serpiginosa lutz; Elastoma intrapapillare perforans verruciforme miescher. Dermatologica 1958;116:143-55.
[Google Scholar]
|
| 5. |
Mehregan AH, Schwartz OD, Livingood CS. Reactive perforating collagenosis. Arch Dermatol 1967;96:277-82.
[Google Scholar]
|
| 6. |
Mehregan AH. Elastosis perforans serpiginosa: A review of the literature and report of 11 cases. Arch Dermatol 1968;97:381-93.
[Google Scholar]
|
| 7. |
Mehregan AH. Transepithelial elimination. Curr Probl Dermatol 1970;3:124-47.
[Google Scholar]
|
| 8. |
Bayoumi AH, Marks R. Transepidermal elimination: Studies with an animal model. Br J Exp Pathol 1980;61:560-6.
[Google Scholar]
|
| 9. |
Akoglu G, Sungu N, Karaismailoglu E, Aktas A. Expression of the receptor for advanced glycation end products in acquired reactive perforating collagenosis. Indian J Dermatol Venereol Leprol 2017;83:432-5.
[Google Scholar]
|
| 10. |
Desai CA, Khopkar U. Cutaneous tuberculosis with a difference: Documenting transfollicular elimination of granulomas. Indian Dermatol Online J 2016;7:297-9.
[Google Scholar]
|
| 11. |
Miranda MF, Costa VS, Bittencourt Mde J, Brito AC. Transepidermal elimination of parasites in Jorge Lobo's disease. An Bras Dermatol 2010;85:39-43.
[Google Scholar]
|
| 12. |
Puig L, Pradinaud R. Leishmania and HIV co-infection: Dermatological manifestations. Ann Trop Med Parasitol 2003;97 Suppl 1:107-14.
[Google Scholar]
|
| 13. |
Woo TY, Rasmussen JE. Disorders of transepidermal elimination. Part 1. Int J Dermatol 1985;24:267-79.
[Google Scholar]
|
| 14. |
Woo TY, Rasmussen JE. Disorders of transepidermal elimination. Part 2. Int J Dermatol 1985;24:337-48.
[Google Scholar]
|
| 15. |
Weedon D. Disorders of elastic tissue. In: Weedon D, editors. Weedon's Skin Pathology. 3rd ed. Edinburgh: Churchill Livingstone; 2010. p. 331-51.
[Google Scholar]
|
Fulltext Views
10,253
PDF downloads
3,880





