Translate this page into:
A case of Marshall's syndrome (postinflammatory elastolysis)
2 Department of Dermatology, Medical Faculty, Balıkesir University, Balıkesir, Turkey
3 Department of Pathology, Gulhane School of Medicine, Ankara, Turkey
Correspondence Address:
Aslan Y�rekli
Department of Dermatology, Gulhane School of Medicine, Etlik, Kecioren, Ankara 06018
Turkey
| How to cite this article: Y�rekli A, Açıkgöz G, Can &, Çalışkan E, Yavan &. A case of Marshall's syndrome (postinflammatory elastolysis). Indian J Dermatol Venereol Leprol 2017;83:218-220 |
Sir,
Cutis laxa is a rare connective tissue disorder, which may be inherited or acquired. The disease is characterized by sagging and wrinkling of the skin and may also affect other organ systems. Marshall's syndrome is a type of acquired cutis laxa characterized by cutaneous involvement alone and occurs following inflammatory dermatoses such as Sweet's syndrome.
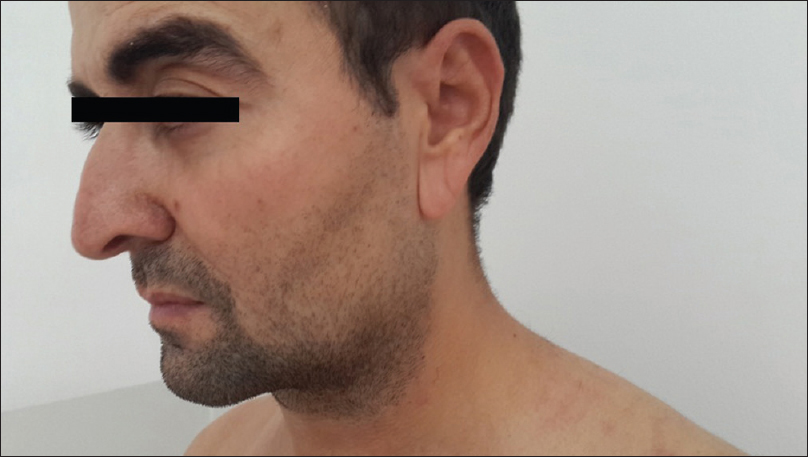
A 28-years-old man presented with tiny reddish elevated lesions on various parts of his body since six months [Figure - 1]. The patient also noticed sagging of his facial skin, coinciding with the onset of these papules. Dermatological examination revealed multiple erythematous papules on his trunk, along with sagging and wrinkling of the facial skin [Figure - 2]. This was more pronounced on the helices of his ears [Figure - 3] and the skin elasticity was decreased, resulting in an aged appearance. Skin biopsy from the asymptomatic erythematous papules on the trunk revealed a normal epidermis with dermal interstitial neutrophilic infiltrates. Special stains for elastin revealed fragmentation of elastic fibers. [Figure - 4]. Laboratory investigations were within the normal range.
 |
| Figure 1: Erythematous papules on the trunk |
 |
| Figure 2: 2 years before the onset of disease and the current appearance |
 |
| Figure 3: Wrinkling and sagging of the helices of both the ears |
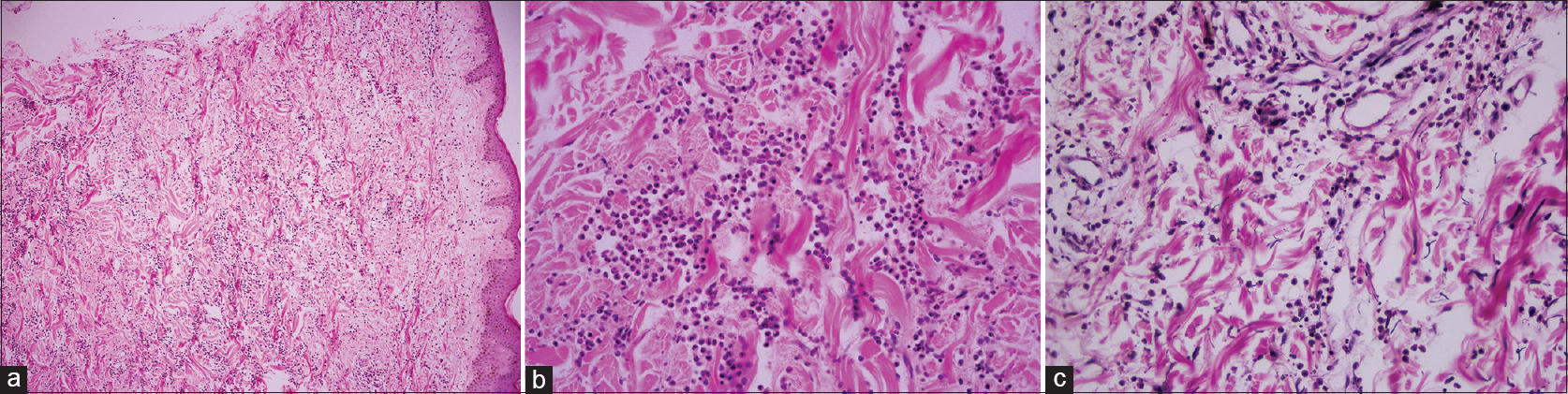 |
| Figure 4: (a) Intense neutrophilic dermal infiltrate in reticular dermis, epidermis is normal, (b) In high power field, there are dermal papillary microabscesses (H and E, ×400) (c) With special stains, elastin fibers show marked degeneration of fibers with a short and curled appearance (Verhoeff Elastic, ×400) |
In view of the clinical, laboratory and histopathological findings, we made a diagnosis of postinflammatory elastolysis, which is defined as acquired cutis laxa Type 2 (Marshall's syndrome). Though there is no curative treatment for elastolysis, the patient was prescribed topical corticosteroid for the papular lesions. During follow-up, all the treated lesions were found to have regressed in 6 months indicating that disease progression had stopped. No recurrence was observed after 1 year.
Cutis laxa is a disorder affecting connective tissues characterized by premature aging.[1],[2] It may be inherited or acquired. Inherited forms comprise autosomal dominant cutis laxa, autosomal recessive cutis laxa, Urban–Rifkin–Davis syndrome, macrocephaly-alopecia-cutis laxa-scoliosis syndrome, arterial tortuosity syndrome and X-linked cutis laxa.[3],[4] The acquired form is divided into two groups according to the clinical and histological features: Type 1 or generalized acquired elastolysis and type 2 or Marshall's syndrome.[5] A number of etiologic factors such as medications, malignancies, infections, connective tissue diseases, renal diseases, alpha-1 antitrypsin deficiency, mastocytosis, amyloidosis, dermatitis herpetiformis, interstitial granulomatous dermatitis, sarcoidosis and celiac disease have been described to be associated with acquired cutis laxa type 1. It tends to be more prevalent in adults.[2],[5] On the other hand, acquired cutis laxa type 2 (Marshall's syndrome) usually develops as a post-inflammatory phenomenon. Moreover, it tends to occur in infants and children.[4]
Marshall's syndrome was first described by Marshall, Heyl and Weber in 1966.[5] Factors that play a role in the pathogenesis of this disease are not exactly known but several assumptions have been made. The degradation of elastin fibers is central totheories about pathogenesis.[2],[5] Elastin fibers are degraded by the enzyme, elastase. One of the most important theories in pathogenesis is that elastase activity increases when neutrophils accumulate, as neutrophils are an important source of elastase.[2],[5] Another factor indicted in the pathogenesis is the dysfunction of elastase inhibitors such as alpha-1 antitrypsin. In patients with pulmonary involvement, this enzyme deficiency may be determined.[1],[2] Biopsy shows a dermal infiltrate of neutrophils, while the epidermis is usually unaffected. In our case, the elastic fibres seem to be fragmented by the neutrophils in the dermis, a feature described in this condition.[4],[5]
Anetoderma and mid-dermal elastolysis should be considered in the differential diagnosis. In anetoderma, the lesions are smaller and herniate on palpation. Mid-dermal elastolysis shows a different pattern of elastolysis in the mid-reticular dermis and generally does not affect the face.[4]
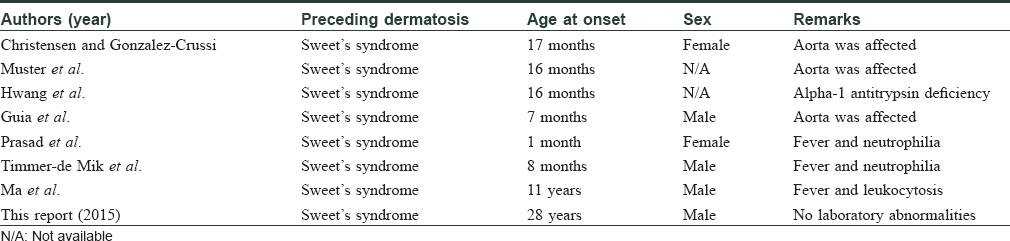
In conclusion, Marshall's syndrome is a rare disorder, the pathogenesis of which is still not fully understood. We were able to find seven previous reports of this condition [Table - 1].[5] There is no effective treatment for this rare condition. More studies are needed to elucidate the pathogenesis and find newer avenues of treatment for this unusual disorder.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Haider M, Alfadley A, Kadry R, Almutawa A. Acquired cutis laxa type II (Marshall syndrome) in an 18-month-old child: A case report. Pediatr Dermatol 2010;27:89-91.
[Google Scholar]
|
| 2. |
Hwang ST, Williams ML, McCalmont TH, Frieden IJ. Sweet's syndrome leading to acquired cutis laxa (Marshall's syndrome) in an infant with alpha 1-antitrypsin deficiency. Arch Dermatol 1995;131:1175-7.
[Google Scholar]
|
| 3. |
Timmer-DE Mik L, Broekhuijsen-VAN Henten DM, Oldhoff JM, DE Geer DB, Sigurdsson V, Pasmans SG. Acquired cutis laxa in childhood Sweet's syndrome. Pediatr Dermatol 2009;26:358-60.
[Google Scholar]
|
| 4. |
Ma EH, Akikusa JD, MacGregor D, Ng J, Su JC. Sweet's syndrome with postinflammatory elastolysis and Takayasu arteritis in a child: A case report and literature review. Pediatr Dermatol 2012;29:645-50.
[Google Scholar]
|
| 5. |
Çaliskan E, Açikgöz G, Yeniay Y, Özmen I, Gamsizkan M, Akar A. A case of Marshall's syndrome and review of the literature. Int J Dermatol 2015;54:e217-21.
[Google Scholar]
|
Fulltext Views
4,942
PDF downloads
1,862





