Translate this page into:
Actinomycotic osteomyelitis
2 Department of Oral Pathology and Microbiology, Dr. D. Y. Patil Vidyapeeth's Dr. D. Y. Patil Dental College and Hospital, Pune, Maharashtra, India
3 Department of Oral Medicine and Radiology, Dr. D. Y. Patil Vidyapeeth's Dr. D. Y. Patil Dental College and Hospital, Pune, Maharashtra, India
Correspondence Address:
Supriya Kheur
Dr. D. Y. Patil Vidyapeeth's Dr. D. Y. Patil Dental College and Hospital, Pimpri, Pune - 411 018, Maharashtra
India
| How to cite this article: Ingle Y, Madalli R, Reddy MG, Kheur S, Ingle M. Actinomycotic osteomyelitis. Indian J Dermatol Venereol Leprol 2017;83:468-469 |
Sir,
Actinomycosis is a rare, chronic disease caused by a group of anaerobic, Gram-positive bacterium, Actinomyces israelii. A. israelii accounts for 52% of the infections, whereas Actinomyces viscosus, Actinomyces odontolyticus, Arachnia propionica and Actinomyces meyeri contribute to 40%, 5%, 2%, 2% and 1%, respectively.[1] It is a non-acid fast, filamentous branched bacterium. Cope in 1938 suggested that the infection may be anatomically classified as cervicofacial (i.e. lumpy jaw), thoracic or abdominal. The most common presentation is cervicofacial, which accounts for over half of the reported cases.[2] Although rarely seen in day-to-day dental practice, due to its aggressive and locally destructive nature, actinomycosis of the oral cavity is a highly significant condition.[3]
Mucosal discontinuity is needed to lead to infection. We report a case of actinomycotic osteomyelitis leading to extensive destruction of mandibular right anterior region following tooth extraction.
A 28-year-old man reported to the dental outpatient department in Yashwantrao Chavan Memorial Hospital, Pimpri-Chinchwad, Pune, Maharashtra, India, with the chief complaint of painful swelling on the lower right premolar and molar region. On taking a detailed past history, the patient explained that he was diagnosed for noma for which surgical intervention was done by a local doctor. Later, he got his mobile tooth 46 extracted and skin graft was placed elsewhere. After 15 days of extraction, swelling developed in the left premolar region for which he reported to the dental outpatient department in a medical hospital. On extraoral examination, a diffuse swelling extending from the lower right corner of the mouth to the left corner of the mouth was noticed without marginal induration. The swelling was tender on palpation. Intraoral examination revealed pieces of white necrotic bone (sequestrum) and swelling in the buccal mucosa [Figure - 1]. The mucosa over the swelling was reddish showing sinus tract with purulent exudate on the alveolar ridge at the site of tooth extraction. Right submandibular regional lymphadenopathy was seen. Radiographic examination revealed mottled bone appearance.
 |
| Figure 1: Ulcer on the anterior alveolar ridge with necrotic bony spicules |
The swelling was then incised under local anesthesia in aseptic conditions. Caseous material was observed with purulent discharge. Pus culture showed the presence of nonsporing Gram-positive rods. Biopsy was taken and the tissue was histopathologically analyzed. Hematoxylin and eosin stained sections revealed bone with empty lacunae indicating sequestrum. Numerous actinomycotic colonies consisting of club-shaped filaments with basophilic central core and eosinophilic peripheral portion were seen with some neutrophils [Figure - 2] and [Figure - 3]. The histological appearance of the biopsied material was consistent with that of osteomyelitis in association with infection by Actinomyces organisms. Based on this, a diagnosis of actinomycotic osteomyelitis was given. Incision and drainage was performed and amoxicillin along with clavulanic acid 625 mg orally twice daily was prescribed for 7 days. The patient was recalled after a week and continued the medication for another 2 weeks. The patient reported after 2 months with no complaints.
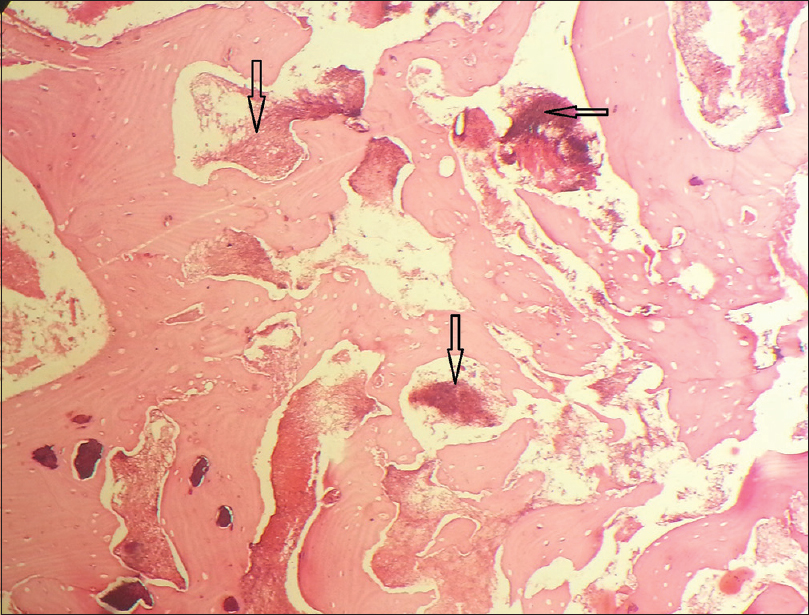 |
| Figure 2: Necrotic bone and actinomycotic colonies in the marrow spaces (H and E, ×100) |
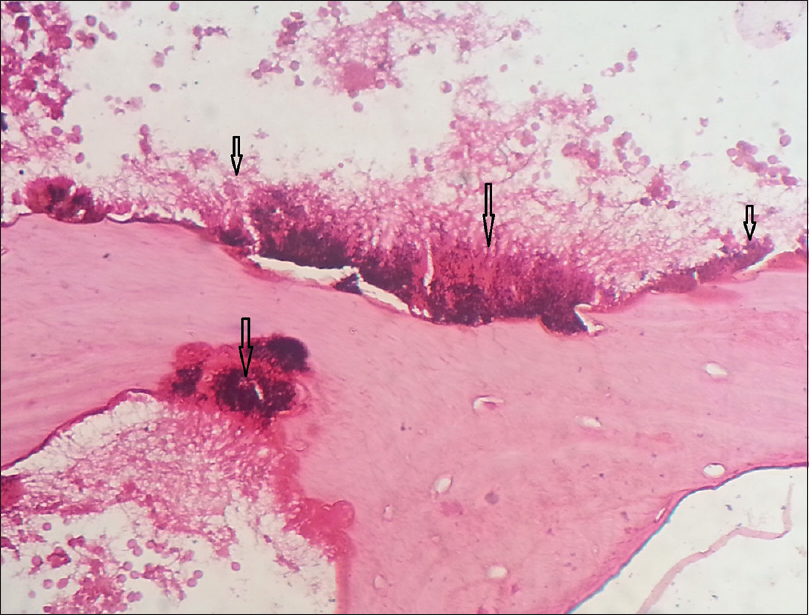 |
| Figure 3: Necrotic bone with empty lacunae and actinomycotic colonies (ray fungus) (H and E, ×400) |
Osteomyelitis due to Actinomyces has been reported infrequently. The spread of Actinomyces by hematogenous route with intraosseous granuloma formation and minimal subperiosteal bone reaction has been reported by Bala et al.[4] In cervicofacial actinomycosis which is the most frequent the mandible is more commonly involved than maxilla (4:1). It requires a break in the integrity of the mucous membranes and the presence of devitalized tissue to invade deeper body structures and to cause disease which occurs through oro-maxillofacial trauma, dental extractions, dental caries or most probably through any dental intervention as the causative organism Actinomyces is not virulent.[2]
Mandibular actinomycotic osteomyelitis is usually underappreciated by many clinicians in their assessment of head and neck infections. Most of the cases are traced to an odontogenic source with periapical tooth abscess and posttraumatic or surgical complication as the key antecedent events.[5] Hence, a biopsy should be performed on any persistent periapical lesion with osteomyelitis even though a chronic draining sinus or cervicofacial abscess does not exist. The most important clinical relevance is to send the discharge for microbial examination rather than only biopsy.
Even though the proper surgical incision and drainage and the administration of antibiotics caused the lesion to regress, sometimes, it can prove potentially fatal. Hence, this disease needs to be considered frequently in the diagnosis of head, neck and intraoral infections.
In the background of debilitating bacterial infections, a vigorous antimicrobial regimen should be followed before undertaking any surgical procedure. Actinomycotic osteomyelitis is a chronic specific suppurative osteomyelitis which is not refractory to treatment. In our case, the patient developed actinomycotic osteomyelitis after tooth extraction as a postprocedural complication. As actinomycotic osteomyelitis develops in patients with poor host immune response, the morbidity and mortality rate should be reduced with proper management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ozaki W, Abubaker AO, Sotereanos GC, Patterson GT. Cervicofacial actinomycoses following sagittal split ramus osteotomy: A case report. J Oral Maxillofac Surg 1992;50:649-52.
[Google Scholar]
|
| 2. |
Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck 1999;21:264-8.
[Google Scholar]
|
| 3. |
Crossman T, Herold J. Actinomycosis of the maxilla – A case report of a rare oral infection presenting in general dental practice. Br Dent J 2009;206:201-2.
[Google Scholar]
|
| 4. |
Bala S, Narwal A, Gupta V, Duhan J, Goel P. Actinomycotic osteomyelitis of mandible masquerading periapical pathology. J Oral Health Comm Dent 2011;5:97-9.
[Google Scholar]
|
| 5. |
Freeman LR, Zimmermann EE, Ferrillo PJ. Conservative treatment of periapical actinomycosis. Oral Surg Oral Med Oral Pathol 1981;51:205-8.
[Google Scholar]
|
Fulltext Views
5,560
PDF downloads
2,657





