Translate this page into:
Generalized lichen planus developing at the healed sites of erythema multiforme in a human immunodeficiency virus-seropositive patient
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Correspondence Address:
Rashmi Kumari
Department of Dermatology, Venereology and Leprology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605 006
India
| How to cite this article: Behera B, Kumari R, Gochhait D, Thappa DM. Generalized lichen planus developing at the healed sites of erythema multiforme in a human immunodeficiency virus-seropositive patient. Indian J Dermatol Venereol Leprol 2017;83:485-489 |
Sir,
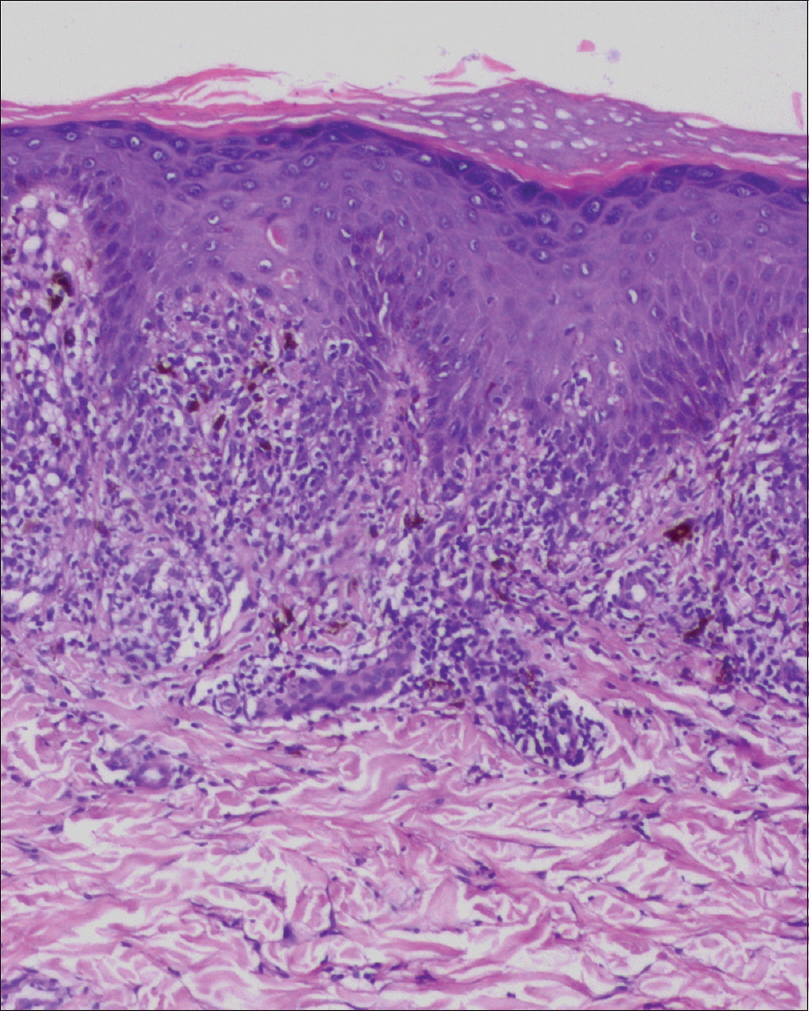
A 62-year-old man presented with 1-week history of skin rash all on the body, oral erosions and ocular discharge 2 days following ingestion of capsule amoxicillin 500 mg three times daily for cough. History of evening rise of temperature and weight loss of around 10% of body weight was present. The patient looked emaciated and had generalized lymphadenopathy. Cutaneous examination revealed multiple erythematous papules, plaques and target lesions distributed symmetrically all over the body including the palms and soles with a few lesions showing central necrosis [Figure - 1]. Mucosal examination revealed erosions on lips [Figure - 2], bilateral buccal mucosa and palate. Ophthalmic examination revealed conjunctival congestion and superficial punctate keratitis. A provisional diagnosis of amoxicillin-induced erythema multiforme was made and the patient was started on prednisolone 0.5 mg/kg/day orally. A skin biopsy taken from one of the target lesions showed orthokeratosis, apoptotic keratinocytes, lymphocyte exocytosis, basal vacuolar degeneration and moderate upper dermal and perivascular lymphohistiocytic infiltrate; consistent with erythema multiforme [Figure - 3],[Figure - 4],[Figure - 5],[Figure - 6]. On investigation, the patient was found to be positive for human immunodeficiency virus-1 by enzyme-linked immunosorbent assay method, and his CD4 count was 335/mm [3]. His chest X-ray features were suggestive of pulmonary tuberculosis and lymph node fine needle aspiration cytology showed reactive hyperplasia. Other investigations were within normal limits. All the erythema multiforme lesions healed over a 3-week period during which prednisolone was tapered and stopped. Two weeks after, the patient started to develop multiple violaceous plaques on the previously healed cutaneous lesions of erythema multiforme on the anterior [Figure - 7] and posterior [Figure - 8] aspects of the trunk and extremities and Wickham's striae in the oral cavity [Figure - 9]. Histology of one of the violaceous plaques showed wedge-shaped hypergranulosis, basal vacuolar degeneration, cytoid bodies and a subepidermal band-like lymphocyte infiltrate with a few histiocytes and plasma cells [Figure - 10]. A diagnosis of lichen planus was made and the patient was treated with topical clobetasol cream twice daily along with anti-retroviral therapy (zidovudine, lamivudine and nevirapine) and category-I anti-tubercular therapy (isoniazid, rifampicin, pyrazinamide and ethambutol).
 |
| Figure 1: Multiple erythematous papules, plaques and target lesions distributed all over the back, neck and upper limbs with a few showing central necrotic area. The arrows point that lichen planus developed at the same site of healed of erythema multiforme lesions |
 |
| Figure 2: Crusted erosions present on the lips |
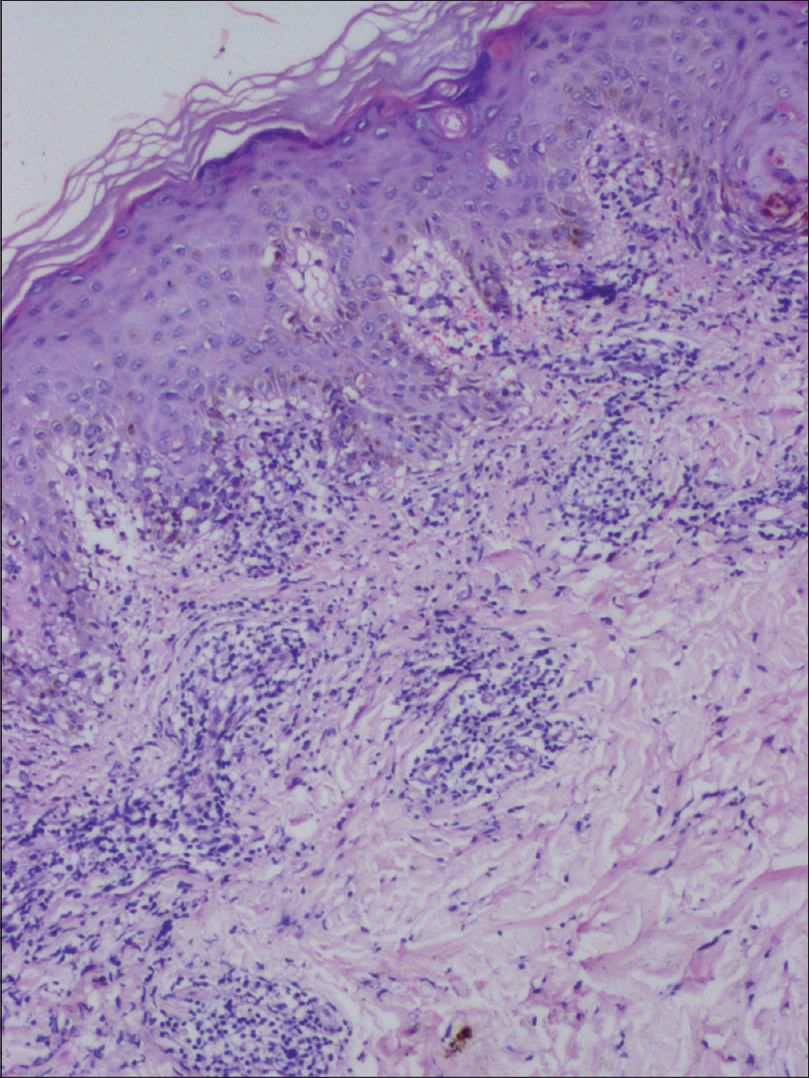 |
| Figure 3: Histology showing lymphocyte exocytosis, apoptotic keratinocytes, basal vacuolar degeneration and moderate dermal and perivascular lymphohistiocytic infiltrate (H and E, ×100) |
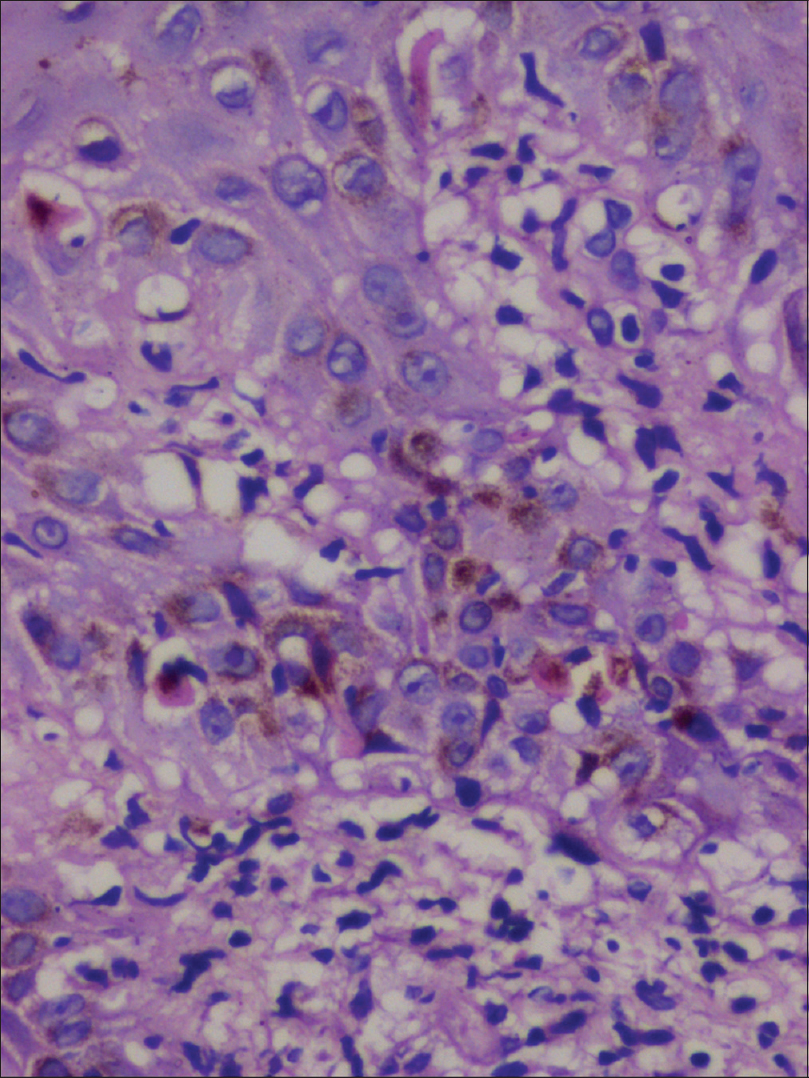 |
| Figure 4: Higher magnification demonstrating multiple apoptotic keratinocytes (H and E, ×400) |
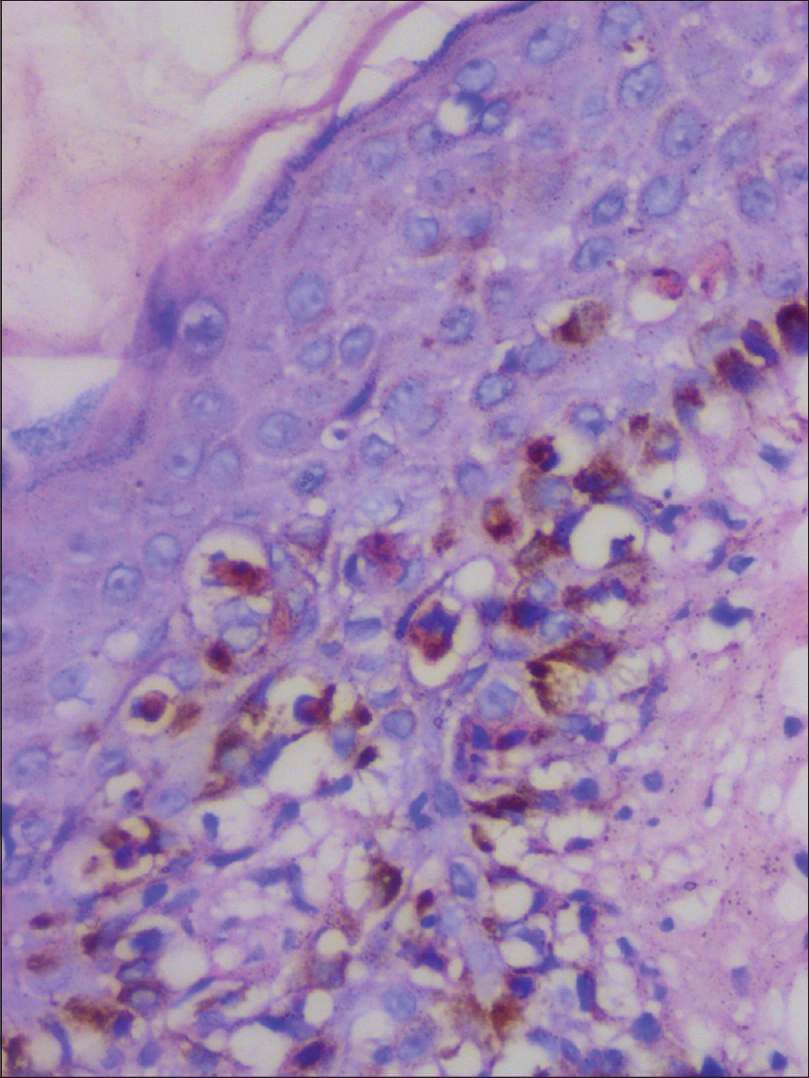 |
| Figure 5: Histology showing prominent basal vacuolar degeneration, basal tagging of lymphocytes, satellite cell necrosis and multiple apoptotic keratinocytes (H and E, ×400) |
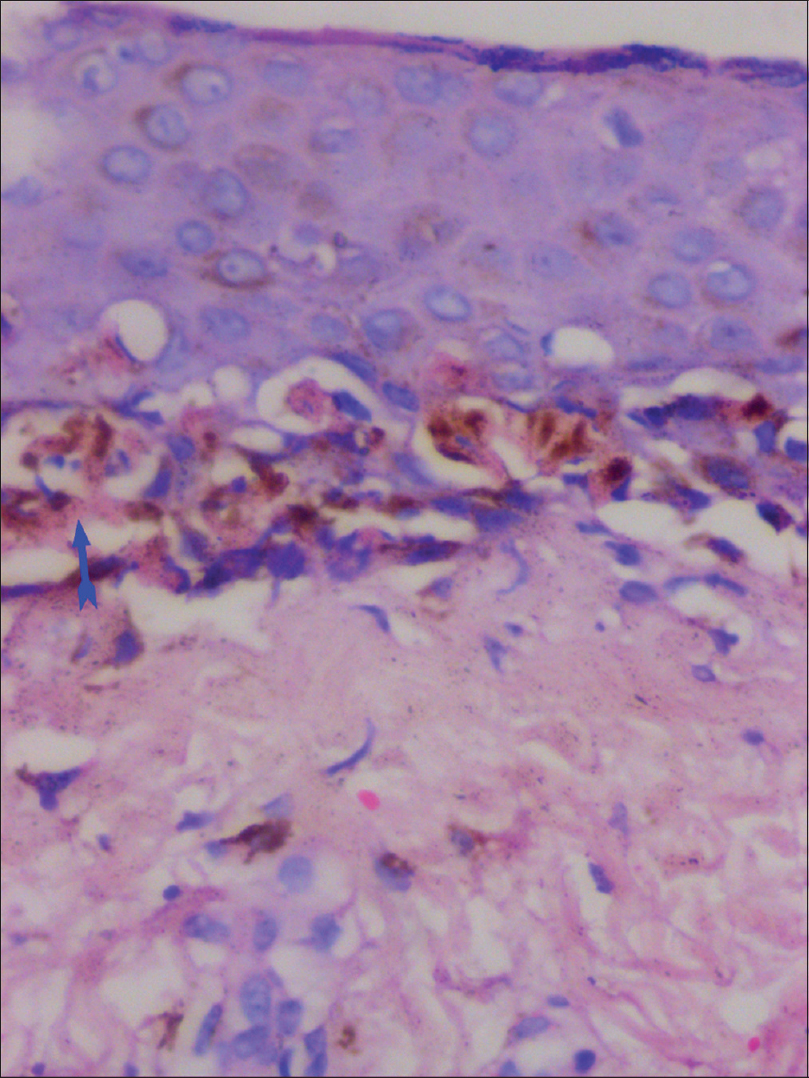 |
| Figure 6: Histology showing prominent basal vacuolar degeneration and confluent keratinocyte apoptosis (arrow, H and E, ×400) |
 |
| Figure 7: Multiple violaceous plaques present all over the anterior aspect of the trunk at the same site of healed lesions of erythema multiforme |
 |
| Figure 8: Multiple violaceous plaques present all over the posterior aspect of the trunk at the same site of healed lesions of erythema multiforme. Arrows to show that lichen planus developed at the same site of previously healed erythema multiforme lesions |
 |
| Figure 9: Wickham's striae on the dorsum of tongue (arrow) |
 |
| Figure 10: Histology showing orthokeratosis, wedge-shaped hypergranulosis, saw-tooth shaped rete ridges, basal vacuolar degeneration, cytoid bodies and subepidermal lymphocytic infiltration (H and E, ×100) |
Immunologically mediated reactions play a significant role in the development of both erythema multiforme and lichen planus.[1],[2] The term “Wolf's isotopic response” refers to the development of a new disease at the site of healed lesions of another unrelated disease.[3] The interval between the healed first disorder and development of the second unrelated disorder varies from days to years. The initial dermatosis described in Wolf's isotopic response is most commonly herpes zoster, and others being herpes simplex, varicella, vaccination site, burn scar, leishmania, etc.[4],[5] The second dermatosis may be classified as granulomatous reactions (granuloma annulare, tuberculosis, sarcoidosis, granulomatous vasculitis), malignant tumors (basal cell carcinoma, squamous cell carcinoma, Kaposi's sarcoma, angiosarcoma, lymphoma, etc.), leukemic infiltrates, dermatoses secondary to immunologic dysfunction (pseudolymphoma, lichen planus, etc.), infections (tinea, furuncle etc.), comedonal reactions and other miscellaneous conditions.[4],[5] The pathomechanism responsible for Wolf's isotopic response is not fully understood and various speculations include change in immunological status such as atypical delayed-type hypersensitivity reaction or immunosuppression, viral hypothesis, vascular hypothesis and neural hypothesis. One or more of these factors play role in the development of the second disease along “locus minoris resistentiae.”[5] In our case, the patient developed widespread lichen planus [arrows in [Figure - 8] at the same site of previously healed lesions of erythema multiforme [arrows in [Figure - 1]. Kalbarczyk [6] and Abraham et al.[1] reported development of generalized granuloma annulare on the healed lesions of erythema multiforme in three patients and speculated the reason to be of either Wolf's isotopic response or Koebner phenomenon.[1] The Koebner phenomenon is characterized by the development of typical skin lesions of an existing dermatosis at sites of injuries which was not in our case as the patient did not have any evidence of lichen planus before or at the onset of erythema multiforme. In our case, the occurrence of lichen planus at the healed sites of erythema multiforme is probably due to Wolf's isotopic response rather than an occurrence by chance. The appearance of erythema multiforme made the cutaneous sites more prone (locus minoris resistentiae) to develop lichen planus by a probable mechanism described below. In human immunodeficiency virus-infected individuals, there is an increase in the ratio of CD8+ to CD4+ cells and a decrease in the number of skin-directed CD4+ cells [7] and at the same time development of erythema multiforme is associated with an increase number of epidermal CD8+ cells.[8] The above two factors may have contributed to development of lichen planus at the healed sites of erythema multiforme due to increase in number of epidermal CD8+ cytotoxic T cells leading to keratinocyte damage.[2] In their case report of a postherpetic Wolf's isotopic response, Ise et al., found the presence of skin-resident memory T cells with immune-phenotype CD45RO+ CD8+ CD69+ within the lesional epidermis and postulated the possible role of CD8+ skin-resident memory T cells in the pathogenesis of lichenoid reaction.[9]
Erythema multiforme-like lesions have been described both during the acute human immunodeficiency virus illness and as a presentation of secondary syphilis in human immunodeficiency virus positive patient.[10],[11] In our case, prior history of drug intake and negative Venereal Disease Research Laboratory test ruled out both the conditions.
Review of the literature suggests acitretin as the first-line agent while oral corticosteroids as second-line therapy for treatments of lichen planus.[12] In our case, the patient was treated with topical clobetasol for lichen planus because of the coexisting pulmonary tuberculosis. We report this case to highlight the rare presentation of Wolf's isotopic response in which lichen planus developed on the healed lesions of erythema multiforme.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Abraham Z, Feuerman EJ, Schafer I, Feinmesser M. Disseminated granuloma annulare following erythema multiforme minor. Australas J Dermatol 2000;41:238-41.
[Google Scholar]
|
| 2. |
Rana S, Gupta R, Singh S, Mohanty S, Gupta K, Kudesia M. Localization of T-cell subsets in cutaneous lichen planus: An insight into pathogenetic mechanism. Indian J Dermatol Venereol Leprol 2010;76:707-9.
[Google Scholar]
|
| 3. |
Wolf R, Brenner S, Ruocco V, Filioli FG. Isotopic response. Int J Dermatol 1995;34:341-8.
[Google Scholar]
|
| 4. |
Ruocco V, Brunetti G, Puca RV, Ruocco E. The immunocompromised district: A unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol 2009;23:1364-73.
[Google Scholar]
|
| 5. |
Mahajan R, De D, Saikia UN. Wolf's isotopic response: Report of a case and review of literature. Indian J Dermatol 2014;59:275-82.
[Google Scholar]
|
| 6. |
Kalbarczyk K. Disseminated granuloma annulare in patients with erythema multiforme. Przegl Dermatol 1986;73:398-402.
[Google Scholar]
|
| 7. |
Yang C, Mosam A, Mankahla A, Dlova N, Saavedra A. HIV infection predisposes skin to toxic epidermal necrolysis via depletion of skin-directed CD4+T cells. J Am Acad Dermatol 2014;70:1096-102.
[Google Scholar]
|
| 8. |
Akkurt ZM, Uçmak D, Türkcü G, Yüksel H, Yildiz K, Arica M. Expression of interleukin-17 in lesions of erythema multiforme may indicate a role for T helper 17 cells. Cent Eur J Immunol 2014;39:370-6.
[Google Scholar]
|
| 9. |
Ise M, Tanese K, Adachi T, Du W, Amagai M, Ohyama M. Postherpetic Wolf's isotopic response: Possible contribution of resident memory T cells to the pathogenesis of lichenoid reaction. Br J Dermatol 2015;173:1331-4.
[Google Scholar]
|
| 10. |
Ma JH, Smith S, Gordon LA. Acute HIV infection presenting as erythema multiforme in a 45-year-old heterosexual man. Med J Aust 2015;202:273-5.
[Google Scholar]
|
| 11. |
Wu MC, Hsu CK, Lee JY, Chao SC, Ko WC, Sheu HM. Erythema multiforme-like secondary syphilis in a HIV-positive bisexual man. Acta Derm Venereol 2010;90:647-8.
[Google Scholar]
|
| 12. |
Asch S, Goldenberg G. Systemic treatment of cutaneous lichen planus: An update. Cutis 2011;87:129-34.
[Google Scholar]
|
Fulltext Views
4,159
PDF downloads
2,609





