Translate this page into:
Occupational dermatoses: An Asian perspective
Correspondence Address:
Vinod Kumar Sharma
Room 4070, Teaching Block, 4th Floor, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Bhatia R, Sharma VK. Occupational dermatoses: An Asian perspective. Indian J Dermatol Venereol Leprol 2017;83:525-535 |
Abstract
Occupational dermatoses contribute to a significant portion of work-related diseases, especially in Asia, where a major portion of the workforce is in the unorganized sector. This review article is focussed on the frequency and pattern of occupational skin diseases reported across Asian countries and type of allergens implicated in different occupations. The literature was searched systematically using key words 'occupational dermatoses,' 'occupational skin disease' and name of each Asian country. Ninty five full-text articles were considered relevant and evaluated. Some of the dermatoses seen in industrial workers in Asian countries are similar to those in Western countries, including dermatoses due to chromate in construction and electroplating workers, epoxy resin, and chromate in painters, wood dust in workers in the furniture industry, azo dyes in textile workers and formaldehyde and chromates in those working in the leather and dyeing industries, dermatoses in domestic workers, chefs and health-care workers. Dermatoses in workers engaged in agriculture, beedi (tiny cigars) manufacture, agarbatti (incense sticks) production, fish processing, carpet weaving, sanitation and those working in coffee plantations and coal mines appear to be unique to Asian countries. Recognition of clinical patterns and geographic variations in occupational skin diseases will provide an impetus to further strengthen future research in these areas, as well as improving their management.Introduction
Occupational disease is any disease developing primarily as a result of exposure to risk factors arising from work activity. Occupational dermatoses account for approximately 30%–45% of all occupational diseases and are responsible for an estimated 25% of all lost workdays in the United States.[1] In Asia, the statistics regarding the magnitude of the problem are not available. Dermatoses in Asian workers are similar to those seen in western countries in occupations such as health-care, hairdressing manufacturing industries, food production, construction, machine tool operation, printing, metal plating, leather work, engine service and forestry. On the other hand, there are certain small-scale industries such as carpet weaving, silk industry, beedi manufacturing and coffee plantation which are unique to Asia. Workers engaged in these are at a risk of developing unique, albeit recognizable, work-related dermatoses. In light of the paucity of focused reviews on occupational dermatoses in Asian countries, we reviewed the available data on this subject with an emphasis on the causative agents/allergens. Knowledge about the prevalence of occupational dermatoses in Asia along with their causative agents will help in the early diagnosis and appropriate counseling of patients and has implications for future research on, and management of, these conditions.
Methods
The literature was searched systematically using PubMed and EMBASE databases for English language articles published up to the end of September 2015 using the following key words: “Occupational skin disease,” “occupational dermatoses” and name of each Asian country. Relevant studies in which skin diseases were attributed to occupation were included. Details which were specifically looked for included sample size, clinical features, patch test results (if mentioned) and impact on the quality of life. This review is focused on relevant data on occupational dermatoses obtained only from online databases.
Results
Two hundred and thirty abstracts were identified and screened. From these, 95 full-text articles considered relevant were evaluated. The important aspects of occupational dermatoses in Asians are summarized and presented.
Epidemiology: Recent trends
Occupational dermatoses is one of the major health problems with an estimated annual incidence of 1.89 million/year.[2] Unlike the West, where notification systems exist for occupational dermatoses, Asian countries do not have an established system of reporting these diseases; hence data regarding epidemiology is scant. The incidence of various occupational dermatoses is determined by the degree of socioeconomic and industrial development in an area, resulting in a lot of geographical variation. In Singapore and China, only 56 and 141 new cases, respectively, were reported in the Workplace Safety and Health Statistics Report in 2013.[3],[4] The prevalence rate of occupational dermatoses in Korea was 0.19/100,000 workers.[5] Skin diseases constitute 2.5% of all occupational diseases in Vietnam and 11% in Thailand, compared to 7.1% in Europe.[6],[7],[8] Self-reporting has been shown to be associated with higher incidence rates, as shown in a study from Taiwan in 1994, in which 84% of 18,942 Taiwanese workers responded to a postal questionnaire; the 12-month prevalence rate was 8.2% for upper extremity skin conditions and 56.7% of these dermatoses were considered by the respondents to be work related. Almost 45% reported that they did not seek a definitive diagnosis or therapy from a physician.[9] In a cross-sectional survey of small-scale industries in Nepal, 26% of workers had skin problems, the nature of which was not reported.[10] No concrete data is available from the Indian subcontinent, where occupational research is a more complex issue, due to issues such as child labor, poor industrial legislation, vast informal, unorganized sector, less attention to industrial hygiene and poor surveillance standards.
Occupational contact dermatitis is the most common type of occupational dermatoses. Mathias' criteria are validated for occupational contact dermatitis but have not been adopted uniformly.[11] It has been reported to be the second most common (20%) occupational disease in Singapore and fifth most common (8%) occupational disease in Hong Kong.[12],[13] The incidence of occupational contact dermatitis reported by factory workers in Singapore was 2.5/10,000 workers in 2002. In the Republic of Mauritius, 223 (1.5%) cases of occupational contact dermatitis were found from a total of 14,670 patients presenting to dermatology specialty clinics in the year 2000.[14] A Taiwanese tertiary referral clinic reported occupational hand dermatitis in 36.6% of the patients for the period 1987–1993 and none applied for workers' compensation.[15] The Contact and Occupational Dermatoses Clinic in Singapore has reported a steady decline in the incidence of occupational contact dermatitis, from 262.5 cases/year in 1984–1985 to 93.8 cases/year in 1989–1998 and 62.5 cases/year in 2003–2004. Occupational contact dermatitis constitutes 97.2% of cases of occupational dermatoses.[12] In Malaysia, occupational contact dermatitis comprised 87% of all the cases of occupational dermatoses (108) reported to the Ministry of Health between June 1997 and November 1998.[16]
Like in Western literature, irritant contact dermatitis has been reported to be more common than allergic contact dermatitis in Singapore (62% vs. 37%), Taipei (58.5% vs. 41.5%) and Taiwan (59% vs. 42%).[12],[15] In India, Pakistan and Thailand, occupational allergic contact dermatitis was found to be more common than occupational irritant contact dermatitis (57% vs. 24%, 50% vs. 49% and 76.3% vs. 24.2%, respectively).[17],[18],[19]
The impact of occupational contact dermatitis on daily living activities, interpersonal relationships and self-image was found to be significant in studies from India (n = 117) and Israel (n = 70).[17],[20]
Occupational dermatoses: Classification
Of all the occupational dermatoses, occupational contact dermatitis is the most common, accounting for 79%–95% of cases.[11] Contact urticaria, occupational marks, infectious dermatoses and neoplasia are other described causes. Occupational dermatoses in various occupations are discussed below.
Occupational dermatoses in agricultural workers
Majority of the Asian workforce is engaged in agriculture, which is considered to be one of the most hazardous industries by International Labour Organization but with no legal protection. Further, being largely uneducated, the working population, is unaware of the hazards associated with their occupation.
Plant-related dermatitis
Agriculture, horticulture, olericulture, floriculture, fruit packaging, hobby gardening and forestry are the various forms of farming.
Parthenium dermatitis is one of the most common causes of occupational dermatoses in India.[17]Parthenium hysterophorus is a weed found abundantly along roads and in fields. The incriminated allergen is a sesquiterpene lactone called parthenin. Exposure may be due to direct contact, or airborne. It causes itchy scaly plaques on the exposed sites involving the folds in airborne contact dermatitis, while in some cases, the pattern may change to lichenified plaques over sun-exposed distribution (chronic actinic dermatitis-like) or a mixed pattern [Figure 1a] and [Figure 1b].[20] Other plants in Compositae family reported to cause allergic contact dermatitis are chrysanthemums, namely Helianthus annuus (sunflower), Dahlia pinnata (pinnate dahlia), Mikania scandens and Holigarna ferruginea.[21],[22],[23] Occupational allergic contact dermatitis from the flowers of Walidda antidysenterica has been reported in florists.[24] In Sri Lanka, Compositae plants such as Tithonia diversifolia mainly cause allergic contact dermatitis, clinically manifesting as parthenium dermatitis.[25]
 |
| Figure 1a: Lichenified plaques involving face and neck (mixed pattern of parthenium dermatitis) |
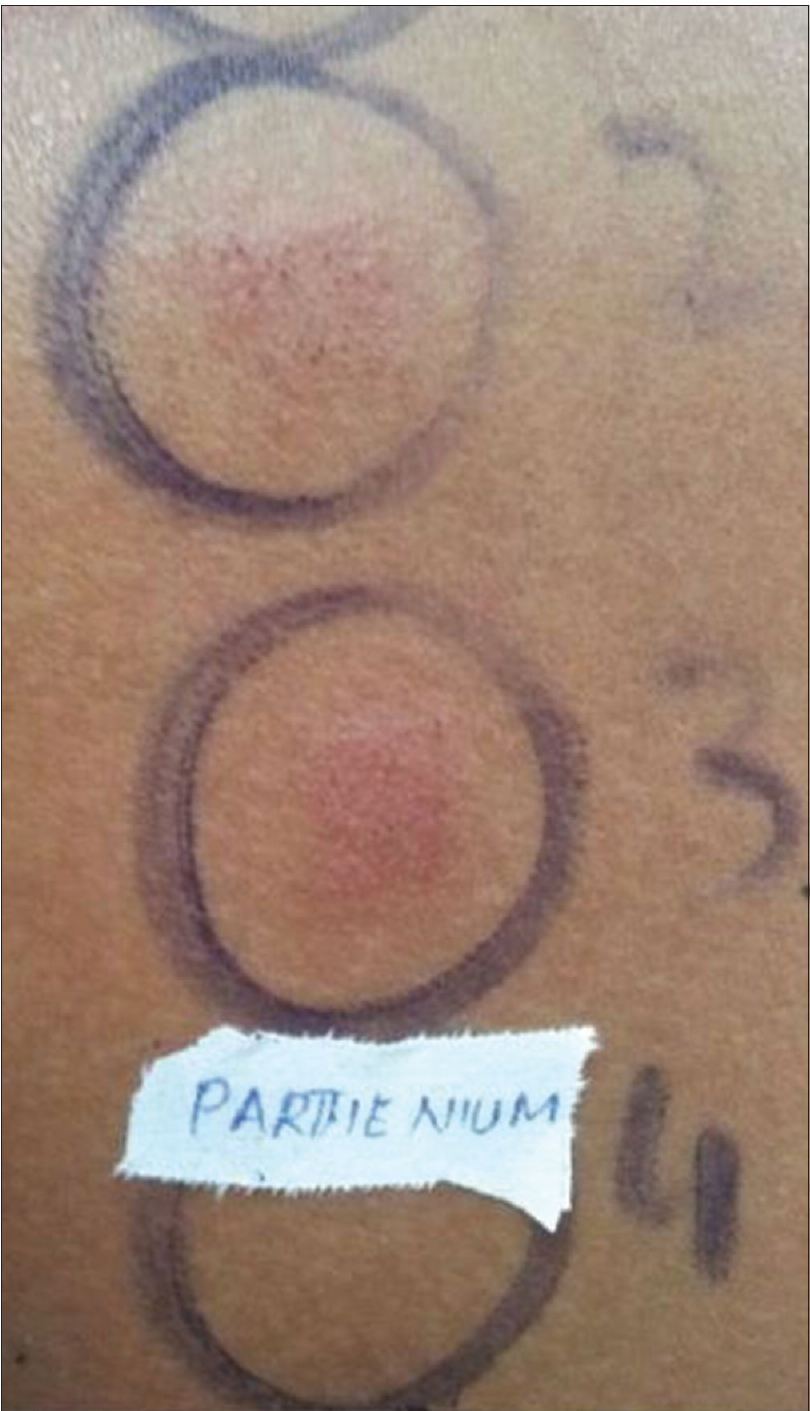 |
| Figure 1b: Positive patch test to parthenium extract (1:100, 1:200 in acetone) in the same patient |
In Japan, occupational allergic contact dermatitis is reported in farm workers secondary to tobacco leaves, mitsuba (Cryptotaemia japonica Makino) vegetable leaves and its stalks and okra (or lady's fingers, Hibiscus esculentus) leaves.[26],[27],[28] There is a recent report of airborne contact dermatitis due to Japanese cedar pollen.[28] In Taiwan, dermatitis is reported in 30% of fruit farmers.[29]
In the Philippines, tropical plants are found in abundance. Irritant contact dermatitis has been reported to develop as a result of contact with chemicals released (alkaloids, silicates) or mechanical irritation by trichomes and glochidia of plants such as Arena pinnata, Calotropis gigantea, Mangifera caesia, Capsicum annuum, Hierba mala, Dieffenbachia and Fleurya interrupta. Allergic contact dermatitis involving the perioral area has been reported with M. caesia.[30]
In Vietnam, workers involved in agriculture, farming and flower cultivation were found to suffer from dermatitis secondary to wastewater. In a nested case–control study in Vietnam, work involving wastewater exposure was associated with a significant increase in skin diseases (32 episodes/100 person-years at risk). In Cambodia, dermatitis was found in 6.1% of aquatic plant culture workers. However, unlike in Vietnam, a consistent association between occupation and skin diseases could not be established.[31],[32]
In Thailand, allergen thitsiol in the lacquer tree (Melanorrhoea usitata, Anacardiaceae family) is a common cause of allergic phytodermatitis.[33]
Pesticide-related dermatoses
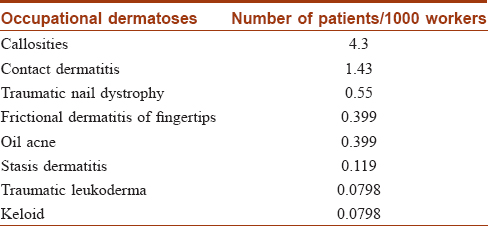
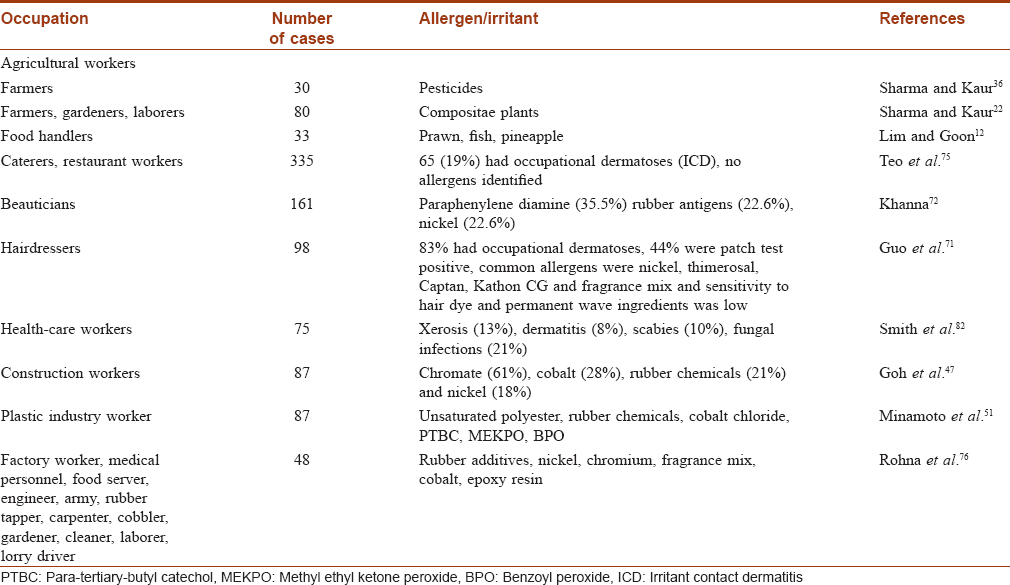
Pesticides are perhaps underreported as a cause of occupational dermatitis. Prevalence reported in a large study from Japan was 39 per cent [34] The exact prevalence of pesticide dermatitis in India is not known, but 26.7%–36.6% of farmers with dermatitis had a positive pesticide patch test.[35],[36] Pesticide dermatitis can occur due to solvents, impurities or the chemical itself. Contact with pesticides may occur during sowing of previously sprayed crops or during spraying itself, especially when protective measures are not followed. Sweating and use of leaky spray equipment are the additional risk factors. Diagnosis is often difficult because of constant changes in the pesticides used at a given time and place. Pesticides frequently identified in causing contact dermatitis are dithiocarbamates, propargite, benomyl, sulfur, captan, chlorothalonil, pyrethroids and chlorophenoxy and organophosphorus compounds. Alachlor is a rarely reported cause of occupational allergic contact dermatitis in agricultural workers in Korea.[37] However, depending on the type of crops, results of patch testing vary across regions as a number of pesticides are used in different parts of the world [Table - 1].[27],[30],[35],[36],[38],[39]
Cashew nut-related dermatoses
Anacardium occidentale, belonging to Anacardiaceae family, has been shown to contain a highly irritating chemical, anacardic acid in its fruit shells.[40] The phenols of this plant are also potentially allergenic. A cashew nut factory worker from India with fissuring and exudative hand dermatitis was patch test positive with 0.1% cashew nut shell oil as well as pericarp and kernel as such.[41] Miliaria, intertrigo and keratosis were commonly found in cashew nut workers in India.[42] There are reports of allergic contact dermatitis in cashew nut workers in Sri Lanka and the Philippines.[27],[31] Barrier creams and castor oil have been used effectively to protect workers from developing dermatitis.
Paddy field work-related dermatoses
Paddy (Oryza sativa) belongs to the grass (Gramineae) family. Paddy field workers are exposed to various irritants (mud, cow dung or other manure, fertilizers, pesticides and dust from the dried plant and grains during thrashing). In a study done in South India, out of 341 paddy field workers examined for skin diseases, 73% complained of itching that correlated with the work. Involvement of hands was as hyperkeratosis (26.4%), nail dystrophy (15.2%) and paronychia (8.8%). A positive patch test to O. sativa was reported to 10% paddy extract in four patients.[43]
Occupational dermatoses in industrial workers
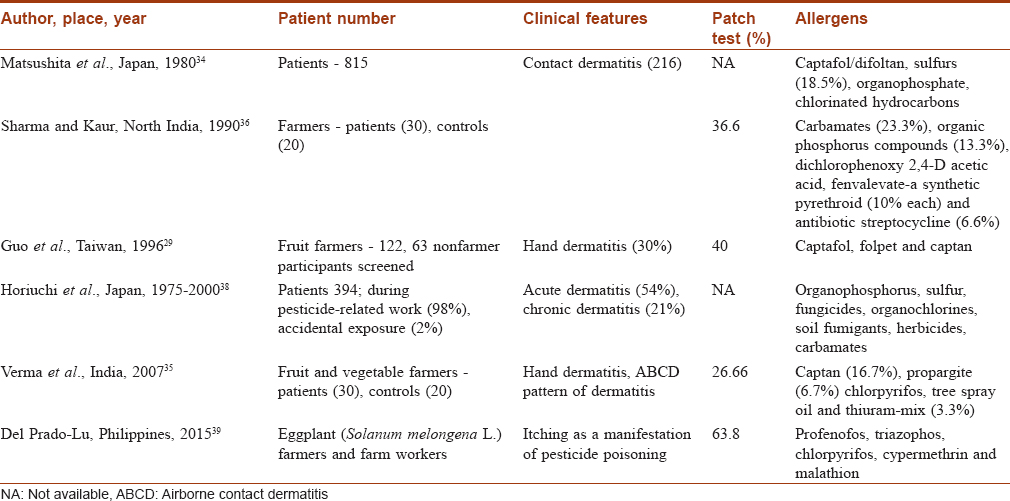
Progressive industrialization has led to an increased exposure to various chemicals, thus posing occupational hazards. The metal, engineering, construction, electronics and transport industries are the major sources of occupational dermatoses.[12] Chromate was found to be the most common allergen while cutting fluid was the most common irritant leading to occupational contact dermatitis.[12] In a survey on 25,050 employees working in ten industrial units (manufacturing rotating machines, tractors, leaf spring, footwear, antibiotics and dashboard instruments, gaskets; units involved in printing synthetic cloth and cotton and books and copper mines) around New Delhi by Mathur et al.,[44] the incidence of occupational dermatoses was very low [Table - 2][44]].
Dermatoses in construction industry workers
The construction industry employs 7.5% of the world's labor force.[45] In India, it is the second largest industry, after agriculture and consists of 44% of all urban unorganized workers.[45] In a study by Bhatia et al., construction workers included masons (27/32), laborers (2/32), plumbers (1/32) and tile layers (2/32).[17] Construction workers are exposed to multiple irritants and potential sensitizers such as cement, chalk, fly ash, hydrochloric acids, epoxy resin, rubber, leather gloves, adhesives, wood preservatives and phenol-formaldehyde-impregnated fiberglass. Most commonly, there is involvement of fingers and toes as oozy itchy scaly plaques [Figure 2a] and [Figure 2b].[17] Acute irritant reaction manifests clinically as cement burns [Figure 2c].
 |
| Figure 2a: Cement dermatitis on the dorsa of fingers distally |
 |
| Figure 2b: Irritant reaction leading to ulceration in a cement worker |
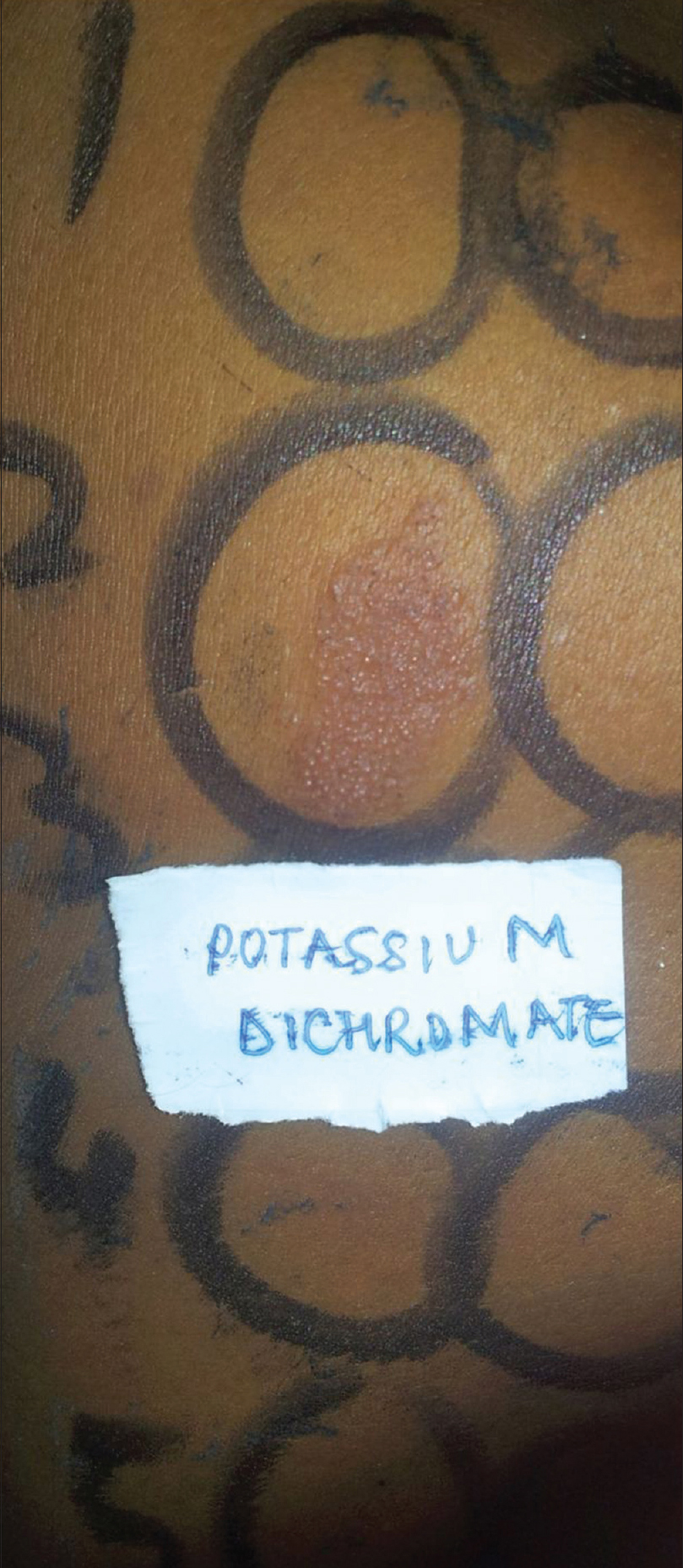 |
| Figure 2c: Patch test positive to potassium dichromate 0.5% |
In Singapore, allergic contact dermatitis was more common than irritant contact dermatitis among construction workers, the common allergens being chrome (94.5%), cobalt and rubber chemicals.[12] The prevalence rate of chromium sensitivity has been found to be 87.5% in India, 24.5% in Taiwan and 40% in Singapore.[17],[46],[47] In a study done in Kuwait, 112 construction workers with allergic contact dermatitis to cement were followed up for 2 years. Of these, 75% of the patients showed an exacerbation in clinical features during the humid months due to leaching of chromate ions.[48]
Addition of iron sulfate is known to decrease allergenicity of cement. However, it has not been implemented in most of the Asian countries.
Dermatoses in electroplating industry workers
In a study from Singapore, 38% of the chrome platers working in 17 chrome electroplating factories had occupational dermatoses. However, only two workers were found to be allergic to chromate and one to nickel.[49] Subacute hand and forearm eczema was seen in an isolated case who was sensitized to gold chloride in the course of gold plating.[50]
Dermatoses in plastic factory workers
Fiberglass, unsaturated polyester resin and hardeners are the usually implicated agents. Studies have reported skin problems in as many as 58.8% workers, mainly as dermatitis, developing mostly during lamination followed by grinding and cutting of glass fibre.[51] Allergens incriminated in development of allergic contact dermatitis in fiberglass plastic factory workers are unsaturated polyester resin, benzoyl peroxide, methyl ethyl ketone peroxide, styrene, formaldehyde, cobalt chloride and para-tertiary butylcathecol.[51] Significantly high risk of work related skin diseases has been found in cross-sectional studies done in Japan with (sample size = 148; odds ratio = 4.10–4.69) and Thailand (sample size = 178; odds ratio = 3.89).[51],[52]
Dermatoses in leather industry workers
A wide range of prevalence for occupational dermatoses has been reported among tannery workers in India, Korea, Bangladesh and Indonesia (2.6%–26.4%).[53],[54],[55],[56] Clinical manifestations found were dermatitis, calluses, paronychia, burn, physical trauma, vitiligo, joint deformity and oil acne.[56] Sensitizers found to be occupationally relevant were potassium dichromate (9.2%), N,N-diphenylguanidine (5.3%), benzidine (3.9%) and sodium metabisulfite (2.6%).[56]
Dermatoses in shoe manufacturing industry workers
In shoe production, there are many possible occupational exposures to a broad spectrum of allergens and irritants contained in adhesives, preservatives, acrylic resins, leather, rubber, dyes and glues. Occupational dermatoses in shoe manufacturing workers are rarely reported in Asia. Prevalence of occupational dermatoses in shoe manufacturing workers ranges from 13.6% (Thailand) to 29% (Indonesia) as callosities (9.5%) and occupational contact dermatitis (7.6%).[57],[58] Overall prevalence of occupational allergic contact dermatitis was 3%, incriminated allergens being dodecyl mercaptan, polyurethane-based adhesives, p-tert-butylphenol formaldehyde resin, triethylenediamine, epoxy resin, diphenylmethane diisocyanate, colophony, formaldehyde, phenyl glycidyl ether, ethylenediamine dihydrochloride and 2-mercaptobenzothiazole.[58]
Dermatoses in electronics industry workers
The electronics industry is the most established industry in Singapore and Taiwan. A study on 3070 electronics workers in Taiwan reported contact dermatitis of hands in 302 (9.8%) patients, associated with a personal history of atopy and metal allergy. Working in wafer bonding, cutting, printing, softening/degluing, impregnation and tin plating was associated with the development of occupational contact dermatitis. Irritant contact dermatitis was more common (35.5%) than allergic contact dermatitis (3.8%). The causative allergens were nickel, cobalt and phenylenediamine.[59] Tan et al. reviewed 149 workers from the electronics industry with occupational dermatoses and found that 40.9% had occupational allergic contact dermatitis. Allergens implicated were nickel and resins, followed by rubber chemicals and the constituents of flux and epoxy resin.[60] Flux is also a common irritant and is required to facilitate proper soldering.
Dermatoses in paint industry workers
Unlike the Western literature, data regarding occupational dermatoses in painters is scant in Asia, probably due to underreporting. Recently, in a series reported from India, seven painters were found to have occupational contact dermatitis presenting as crusted, oozy plaques predominantly involving the dorsa of hands.[17] Occupational allergic contact dermatitis was seen in 85% of the painters in varying proportions to epoxy resin, potassium dichromate, glue and colophony.[17] An epidemic outbreak of irritant contact dermatitis to tri-N-butyl tin oxide in paint was reported in Singapore.[61] In China, cases of occupational contact dermatitis to toluene diisocyanate were reported to develop at a concentration of 0.11 mg/m [3] in paint.[62]
Dermatoses in furniture industry workers
Working in a furniture industry places the workers at a risk of dermatitis secondary to wood dust and resins. Synthetic and natural resins, quinones, other ingredients in sawdust, preservatives in glues, acrylates and adhesives are the common allergens. The prevalence of occupational dermatoses was 3.8% in a study of 479 sanders in the furniture-making industry in Singapore.[63] Dimethylfumarate was recently found to be responsible for the epidemic of Chinese sofa dermatitis.[64] Reactions have been reported to Rengas woodin Singapore, Malaysia and Indonesia(belongs to Anacardiaceae family).[65] Urushiol is another allergen, found in the Japanese lacquer tree (Toxicodendron vernicifluum) of the Anacardiaceae family which can lead to occupational allergic contact dermatitis in carpenters, furniture makers and polishers.[66]
Dermatoses in automobile industry workers
It has been estimated that 50% of this sector is unorganized in India. Allergic or irritant dermatitis may develop depending on the type of work (molding and production of large engine blocks, etc., in ferrous foundries or vehicle parts' assembly or vehicle finishing). Oil acne/folliculitis, leukonychia and callosities may develop due to irritant oils/mechanical causes. Allergens to which these workers are commonly exposed are chromium, cobalt, nickel, epoxy resins and rubber allergens, while cutting oil is the major irritant incriminated. In a survey of 106 automobile repair workers in Vellore, India, 11 (10.6%) were found to have features of contact dermatitis.[67]
Dermatoses in textile industry workers
A large portion of India's earnings come from textile industries. A study involving 1300 textile industry workers in India reported occupational dermatitis in 100 (7.6%) workers, primarily involving the dorsa of hands. Patch test was positive in 81/100 patients. The most common causative allergens were azo dyes Red RC Base (48%) and naphthol (29%).[68] In textile dermatitis, disperse dyes are most often implicated. These are present in clothing including undergarments and occurrence of dermatitis is more common in the areas of friction and sweating, such as, suprapubic area, axillae and inframammary areas [Figure - 3].
 |
| Figure 3: Contact dermatitis to textile dye in undergarments |
Dermatoses in silk industry workers
Dermatitis has been reported commonly in silk reeling industry in Korea and India as fissuring and erosions on fingers (2.6%–51.8%).[69],[70] Silk workers are exposed to various allergens and irritants at different steps of silk manufacturing. While cocoons are immersed in hot water to loosen fibers, workers tend to put their bare hands in hot water to see whether the fibers are loosened to pick silk thread for unwinding. Acid/azo dyes used on the proteinaceous fibers of silk can also cause allergic contact dermatitis. Other potential allergens to which workers are exposed are chromium, formaldehyde and pesticides.
Occupational dermatoses in hairdressers/beauticians/masseurs
Hairdressers are exposed to diverse irritants and allergens. Dermatitis has been reported in 83% of hairdressers in Taiwan.[71] Positive patch test reactions were observed with para-phenylene diamine, shampoos, rubber allergens, nickel, ammonium thioglycolate, ammonium persulfate and detergents. Beauticians with atopic dermatitis were found to develop hand eczema more than nonatopics (P< 0.05).[72]
Occupational dermatoses in domestic workers/kitchen workers
Homemakers have been reported to be the common occupational group (68.2%) affected by dermatitis due to contact with irritants and allergens in addition to the trauma of rubbing and scrubbing.[73] Fingertip dermatitis, cumulative insult dermatitis and paronychia may be seen [Figure - 4]. Occupational irritant contact dermatitis has been found to be more common than occupational allergic contact dermatitis. Allergens implicated in a study from India were vegetables (48%).[17] In a study on 110 patients of chronic paronychia in Singapore, 48% of the patients were homemakers and the cause was found to be repeated mechanical insult due to domestic chores.[74] However, whether patch testing was done is not mentioned, hence any allergic component cannot be ruled out.
 |
| Figure 4: Cumulative insult dermatitis in a homemaker |
Dermatoses in kitchen workers/chefs
In a study on 457 chefs in Singapore, the 12-month prevalence of contact dermatitis was 10%, all cases being irritant contact dermatitis.[75] Workers involved in catering in Malaysia were reported to have fingertip dermatitis to onions.[76] In India, a study screened 273 workers, of which 206 had work-related dermatoses (callosities, pitted keratolysis, scalloped nails and paronychia).[77] Food-related contact urticaria and protein contact dermatitis are known secondary to a variety of allergens such as crustacea, shellfish, fruits and vegetables (red-leaved chicory), rice, wheat, eggs, cow's milk, buckwheat and gelatin.[78] Curcuma longa rhizome(turmeric) powder-induced allergic contact dermatitis has been reported in a miller in a spice shop in Singapore.[79]
Occupational dermatoses in paramedical workers
Dermatoses in pharmaceutical industry workers
Allergic and photoallergic contact dermatitis has been reported in workers in contact with ranitidinebase powder and carbimazole, respectively.[80]
Dermatoses in health-care workers
Working in health care involves regular exposure to a wide variety of contact irritants and allergens. One-fifth (23%) of dentists are reported to develop occupational contact dermatitis in Thailand.[81] The prevalence of contact dermatitis among nursing staff is reported to be 8% (Taiwan), 11.8% (Korea), 27.6% (Japan) and 70% (India).[82],[83],[84] Usually, there is an involvement of the dorsa of hands as erythematous scaly plaques with a sharp cutoff at the wrist [Figure 5a] and [Figure 5b]. Positive patch test reactions are reported with rubber gloves (50%), nickel (40%), cobalt chloride, fragrance mix and gentamycin (15% each), formaldehyde (12.5%), neomycin sulfate, epoxy resin and mercaptobenzothiazole (10% each), colophony, thiuram mix, nitrofurazone and p-tertiary butylphenol formaldehyde resin (7.5% each), polyethylene glycol 400 (7.5%), benzocaine, chinoform and paraben (5% each) and mercapto mix, woods alcohols and balsam of Peru (2.5% each).[84]
 |
| Figure 5a: Rubber glove dermatitis in a nurse |
 |
| Figure 5b: Patch test positive to rubber glove |
Miscellaneous
Dermatoses in beedi rollers
Beedis are tiny cigarettes filled with tobacco and tied with tendu leaves/Piliostigma racemosum leaves. In the traditional method of beedi rolling, the leaves are cut to size using scissors. Then, a metallic nail or bamboo stick with or without glue is used to roll the leaf after which the beedi is filled with tobacco. In a study from India, out of 91 beedi workers, callosities were seen in 51 (56.1%) on fingers and feet, and dermatitis in 29 workers. Use of scissors for cutting leaves and gum and artificial metallic nails for rolling beedis was found to cause callosities and localized nail changes which are considered to be occupational marks in beedi rollers.[85]
Dermatoses in agarbatti workers
The manufacture of agarbattis (incense sticks) is a traditional cottage industry in India. It involves raw materials comprising bamboo sticks, jigat powder and charcoal. Skin problems have been described due to exposure to phthalic acid esters used in the production of agarbattis, leading to blisters on hands.[86]
Dermatoses in carpet weaving industry workers
Informal small-scale industries involved in producing hand-weaved carpets are an important sector in India, China, Turkey, Iran and Pakistan. Noorbala found hyperkeratotic nodules and plaques on the hands and fingers among carpet handweavers.[87]
Dermatoses in laundry workers
Laundry workers in India and Sri Lanka have been reported to develop allergic contact dermatitis with an urushiol-containing black oleoresin extracted from the nut of Semecarpus anacardium on the nape of the neck.[26],[88] This is also known as “dhobie mark dermatitis.”
Dermatoses in betel sellers
Betel quid (seeds of the Areca catechu) chewing is widely prevalent in Asia. Betel sellers have been reported to have irritant finger dermatitis. Betel leaf contains eugenol, an irritant chemical that can cause perleche and cheilitis granulomatosa.[89]
Dermatoses in fishery workers
Traditional fishery is one of the main occupations in Maldives placing the workers at a risk of contact dermatitis to fish proteins as well as rubber gloves. A study on fishermen in Basrah, Iraq, showed significantly increased prevalence of marine stings, infections (bacterial, fungal and warts), photodamage (wrinkles, freckles) and contact dermatitis as compared to controls.[90]
Dermatoses in coffee plantation workers
In a study of 34 coffee plantation workers, 19 had erythema on photo-exposed areas. Nail changes as periungual telangiectasia, distal onycholysis, splinter hemorrhages and distal nicking were seen in some of the patients. The workers were exposed to chemicals such as paraquat, benzene hexachloride and Bordeaux, during the process of spraying pesticides.[91] However, the exact cause of such manifestations remains unknown.
[Table - 3] presents an overview of the various studies done involving different occupations from Asia.
Dermatoses in coconut tree climbers
Callosities and irritant dermatitis are reported in coconut tree climbers in India. It develops as a result of friction involved in gripping the tree while climbing.[92]
Dermatoses in sanitation workers
In a descriptive study involving 294 sanitation workers in China, it was observed that there was a significantly higher prevalence of certain dermatoses such as large pores, telangiectasias, senile warts, deep wrinkles and hair loss (P< 0.05) in sanitation workers compared with control population (administrative staff, n = 113).[93]
Dermatoses in coal miners
In a descriptive study in Pakistan, 41% of coal miners were found to have skin and nail dermatoses attributed to chemicals in the coal and rock. However, the nature of these was not further described.[94]
Dermatoses in photographers
Developing and fixation of photographs involves contact with chemicals such as hydroquinone, chromate, p-phenylendiamine, formaldehyde and acids as well as alkalis. In a cross-sectional study in Tehran involving 100 photographers, 37% were found to have skin diseases (contact dermatitis in 24%, nail hyperpigmentation in 3% and leukoderma in 2%). Skin disorders were more frequent in workers involved in manual printing than those whose occupation involved working with computerized printers.[95]
Occupational marks
Occupational marks are not a disease but develop as a result of mechanical contact which occurs in a peculiar way in different occupations leading to skin changes which are characteristic of that occupation. These are seen in plumbers, coconut tree climbers, musicians and tailors.
Conclusions
Dermatoses seen in industrial workers from Asia are similar to those in Western countries, albeit more common due to a lesser emphasis on preventive measures. These include dermatoses due to chromate in construction and electroplating workers; epoxy resin; chromate in painters; wood dust in furniture workers; azo dyes in textile workers; formaldehyde and chromates in leather workers; dyes, chromates, formaldehyde and pesticides in silk industry workers. Occupational dermatoses in domestic workers, chefs and health-care workers are similar to those seen in Western countries. In Asia, farmers very commonly suffer from contact dermatitis which has been attributed to parthenium and other plants, as well as to pesticides, with allergic contact dermatitis seen more frequently than irritant contact dermatitis. Dermatoses in the workers engaged in agriculture, beedi work, agarbatti manufacturing, coffee plantation, fish processing, carpet weaving, sanitation and coal mining are unique to the Asian countries.
Delineation of various dermatoses in these sectors and knowing the clinical patterns and geographic variation will further strengthen future research and management of occupational dermatoses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
U.S. Department of Labor, Bureau of Labor Statistics. Occupational Injuries and Illnesses Counts, Rates, and Characteristics, 1995. Washington, D.C.: U.S. Department of Labor, Bureau of Labor Statistics; 1998.
[Google Scholar]
|
| 2. |
Leigh J, Macaskill P, Kuosma E, Mandryk J. Global burden of disease and injury due to occupational factors. Epidemiology 1999;10:626-31.
[Google Scholar]
|
| 3. |
Workplace Safety & Health Statistics Report; 2013. Available from: https://www.wshc.sg/files/wshc/upload/cms/file/2014/WSH2013.pdf. [Last accessed on 2015 Jul 05].
[Google Scholar]
|
| 4. |
Pandita S, Panimbang F, George O, Shing Hong SL, Chan C, Hernandez J, et al. The current situation concerning occupational diseases and disclosure of government information in China. Asian Labour Update 2015;85:1-9.
[Google Scholar]
|
| 5. |
Song HS, Ryou HC. Compensation for occupational skin diseases. J Korean Med Sci 2014;29:52-8.
[Google Scholar]
|
| 6. |
Lehtinen S. Informal sector. Asian Pac Newsl Occup Health Saf 2010;17:48-53.
[Google Scholar]
|
| 7. |
Aekplakorn W, Suriyawongpaisal P, Methawikul T. The diagnosis and reporting of occupational diseases: The performance of physicians in Thailand. Southeast Asian J Trop Med Public Health 2002;33:188-92.
[Google Scholar]
|
| 8. |
Craecker WD, Roskams N, Beeck R. Occupational Skin Diseases and Dermal Exposure in the European Union (EU-25): Policy and Practice Overview; 2008. Available from: http://www.osha.europa.eu/publications/reports/TE7007049ENC. [Last accessed on 2015 Jul 05].
[Google Scholar]
|
| 9. |
Shao YH, Yeh WY, Chen CJ, Chen CW, Guo YL. Prevalence of self-reported work-related skin conditions in Taiwanese working population. J Occup Health 2001;43:238-42.
[Google Scholar]
|
| 10. |
Joshi SK, Dahal P. Occupational health in small scale and household industries in Nepal: A situation analysis. Kathmandu Univ Med J (KUMJ) 2008;6:152-60.
[Google Scholar]
|
| 11. |
Mathias CG. Occupational dermatoses. J Am Acad Dermatol 1988;19:1107-14.
[Google Scholar]
|
| 12. |
Lim YL, Goon A. Occupational skin diseases in Singapore 2003-2004: An epidemiologic update. Contact Dermatitis 2007;56:157-9.
[Google Scholar]
|
| 13. |
Hong Kong Government. Occupational Safety and Health Statistics Bulletin. Hong Kong: Labour Department; 2003. Available from: http://www.labour.gov.hk/eng/osh/pdf/archive/bulletin/Bulletin2003.pdf. [Last accessed on 2015 Jul 05].
[Google Scholar]
|
| 14. |
Republic of Mauritius Ministry of Health and Quality of Life. Health Statistics Annual Report 2000. Port Louis: Ministry of Health and Quality of Life; 2000.
[Google Scholar]
|
| 15. |
Sun CC, Guo YL, Lin RS. Occupational hand dermatitis in a tertiary referral dermatology clinic in Taipei. Contact Dermatitis 1995;33:414-8.
[Google Scholar]
|
| 16. |
Sirajuddin H, Roslinah A, Rampal KG, Kuppusamy I, Rohna R, Aziz M, et al. Notification of occupational and work-related diseases and poisonings in Malaysia, 1997-1998. Med J Malaysia 2001;56:25-31.
[Google Scholar]
|
| 17. |
Bhatia R, Sharma VK, Ramam M, Sethuraman G, Yadav CP. Clinical profile and quality of life of patients with occupational contact dermatitis from New Delhi, India. Contact Dermatitis 2015;73:172-81.
[Google Scholar]
|
| 18. |
Boonchai W, Thanomkitti K, Kasemsarn P. Occupational contact dermatitis in tertiary university hospital: A 5-year retrospective study. J Med Assoc Thai 2014;97:1182-8.
[Google Scholar]
|
| 19. |
Arif M, Haroon TS. Occupational contact dermatitis in Lahore, Pakistan. J Pak Assoc Dermatol 2001;11:20-6.
[Google Scholar]
|
| 20. |
Rabin B, Fraidlin N. Patients with occupational contact dermatitis in Israel: Quality of life and social implications. Soc Work Health Care 2007;45:97-111.
[Google Scholar]
|
| 21. |
Siddiqui MA, Singh R, Sharma RC. Contact dermatitis due to Parthenium hysterophorus. Indian J Med Res 1978;68:481-4.
[Google Scholar]
|
| 22. |
Sharma SC, Kaur S. Contact dermatitis from compositae plants. Indian J Dermatol Venereol Leprol 1990;56:27-30.
[Google Scholar]
|
| 23. |
Pasricha JS, Barua KN. Contact hypersensitivity to Mikania scandens – A recently introduced wild creeper of Assam and Meghalaya. Indian J Dermatol Venereol Leprol 1987;53:112-3.
[Google Scholar]
|
| 24. |
Srinivas CR, Kulkarni SB, Menon SK, Krupashankar DS, Iyengar MA, Singh KK, et al. Allergenic agent in contact dermatitis from Holigarna ferruginea. Contact Dermatitis 1987;17:219-22.
[Google Scholar]
|
| 25. |
Perera WD. Plant dermatitis. Sri Lanka J Dermatol 1995;1:2-3.
[Google Scholar]
|
| 26. |
Ohyama K, Uehara T, Nohara T, Nomura S, Arao T. Contact dermatitis due to tobacco leaves. Nihon Hifuka Gakkai Zasshi 1986;96:1677-80.
[Google Scholar]
|
| 27. |
Kanzaki T. Contact dermatitis due to Cryptotaemia japonica Makino. Contact Dermatitis 1989;20:60-1.
[Google Scholar]
|
| 28. |
Yokozeki H, Satoh T, Katayama I, Nishioka K. Airborne contact dermatitis due to Japanese cedar pollen. Contact Dermatitis 2007;56:224-8.
[Google Scholar]
|
| 29. |
Guo YL, Wang BJ, Lee CC, Wang JD. Prevalence of dermatoses and skin sensitisation associated with use of pesticides in fruit farmers of Southern Taiwan. Occup Environ Med 1996;53:427-31.
[Google Scholar]
|
| 30. |
Benezra C, Ducombs G, Sell Y, Foussereau J. Plant Contact Dermatitis. Toronto: B. C. Decker Incorporated; 1985. p. 68.
[Google Scholar]
|
| 31. |
Do TT, van der Hoek W, Nguyen DT, Phung DC, Vu HV, Do DL, et al. Skin disease among farmers using wastewater in rice cultivation in Nam Dinh, Vietnam. Trop Med Int Health 2007;12 Suppl 2:51-8.
[Google Scholar]
|
| 32. |
Anh VT, van der Hoek W, Ersbøll AK, Vicheth C, Cam PD, Dalsgaard A. Peri-urban aquatic plant culture and skin disease in Phnom Penh, Cambodia. J Water Health 2009;7:302-11.
[Google Scholar]
|
| 33. |
Kullavanijaya P, Ophaswongse S. A study of dermatitis in the lacquerware industry. Contact Dermatitis 1997;36:244-6.
[Google Scholar]
|
| 34. |
Matsushita T, Nomura S, Wakatsuki T. Epidemiology of contact dermatitis from pesticides in Japan. Contact Dermatitis 1980;6:255-9.
[Google Scholar]
|
| 35. |
Verma G, Sharma NL, Shanker V, Mahajan VK, Tegta GR. Pesticide contact dermatitis in fruit and vegetable farmers of Himachal Pradesh (India). Contact Dermatitis 2007;57:316-20.
[Google Scholar]
|
| 36. |
Sharma VK, Kaur S. Contact sensitization by pesticides in farmers. Contact Dermatitis 1990;23:77-80.
[Google Scholar]
|
| 37. |
Won JH, Ahn SK, Kim SC. Allergic contact dermatitis from the herbicide alachlor. Contact Dermatitis 1993;28:38-9.
[Google Scholar]
|
| 38. |
Horiuchi N, Oguchi S, Nagami H, Nishigaki Y. Pesticide-related dermatitis in Saku district, Japan, 1975-2000. Int J Occup Environ Health 2008;14:25-34.
[Google Scholar]
|
| 39. |
Del Prado-Lu JL. Insecticide residues in soil, water, and eggplant fruits and farmers' health effects due to exposure to pesticides. Environ Health Prev Med 2015;20:53-62.
[Google Scholar]
|
| 40. |
Oka K, Saito F, Yasuhara T, Sugimoto A. A study of cross-reactions between mango contact allergens and urushiol. Contact Dermatitis 2004;51:292-6.
[Google Scholar]
|
| 41. |
Pasricha JS, Srinivas CR, Krupashanker DS, Shenoy K, Subba PVR, Singh KK. Occupational dermatoses among the cashew nut workers in Karnataka. Indian J Dermatol Venereol Leprol 1988;54:15-20.
[Google Scholar]
|
| 42. |
Premi TH, Jayaprakash K. Histopathological observations of anacardic acid – A phytotoxin responsible for occupational dermatitis. Chem Sci Rev Lett 2014;3:162-5.
[Google Scholar]
|
| 43. |
Shenoi SD, Davis SV, Rao S, Rao G, Nair S. Dermatoses among paddy field workers – A descriptive, cross-sectional pilot study. Indian J Dermatol Venereol Leprol 2005;71:254-8.
[Google Scholar]
|
| 44. |
Mathur NK. Contact dermatitis caused by industrial agents. In: Pasricha JS, Sethi NC, editors. Contact Dermatitis in India. Mumbai: Lyka Lab Publishers; 1981. p. 50.
[Google Scholar]
|
| 45. |
Shah KR, Tiwari RR. Occupational skin problems in construction workers. Indian J Dermatol 2010;55:348-51.
[Google Scholar]
|
| 46. |
Wang BJ, Wu JD, Sheu SC, Shih TS, Chang HY, Guo YL, et al. Occupational hand dermatitis among cement workers in Taiwan. J Formos Med Assoc 2011;110:775-9.
[Google Scholar]
|
| 47. |
Goh CL, Gan SL, Ngui SJ. Occupational dermatitis in a prefabrication construction factory. Contact Dermatitis 1986;15:235-40.
[Google Scholar]
|
| 48. |
Kanan MW. Cement dermatitis and atmospheric parameters in Kuwait. Br J Dermatol 1972;86:155-9.
[Google Scholar]
|
| 49. |
Lee HS, Goh CL. Occupational dermatosis among chrome platers. Contact Dermatitis 1988;18:89-93.
[Google Scholar]
|
| 50. |
Goh CL. Occupational dermatitis from gold plating. Contact Dermatitis 1988;18:122-3.
[Google Scholar]
|
| 51. |
Minamoto K, Nagano M, Inaoka T, Kitano T, Ushijima K, Fukuda Y, et al. Skin problems among fiber-glass reinforced plastics factory workers in Japan. Ind Health 2002;40:42-50.
[Google Scholar]
|
| 52. |
Sripaiboonkij P, Sripaiboonkij N, Phanprasit W, Jaakkola MS. Respiratory and skin health among glass microfiber production workers: A cross-sectional study. Environ Health 2009;8:36.
[Google Scholar]
|
| 53. |
Rastogi SK, Pandey A, Tripathi S. Occupational health risks among the workers employed in leather tanneries at Kanpur. Indian J Occup Environ Med 2008;12:132-5.
[Google Scholar]
|
| 54. |
Lee JY, Kim YH, Kim HO, Kim CW. Occupational dermatoses in tannery workers. Korean J Occup Med 1991;3:104-10.
[Google Scholar]
|
| 55. |
Mohanta MK, Saha AK, Hasan MA. Prevalence and determination of occupational diseases of leather tannery workers. Univ J Zool Rajshahi Univ 2012;31:79-82.
[Google Scholar]
|
| 56. |
Febriana SA, Jungbauer F, Soebono H, Coenraads PJ. Occupational allergic contact dermatitis and patch test results of leather workers at two Indonesian tanneries. Contact Dermatitis 2012;67:277-83.
[Google Scholar]
|
| 57. |
Todd L, Puangthongthub ST, Mottus K, Mihlan G, Wing S. Health survey of workers exposed to mixed solvent and ergonomic hazards in footwear and equipment factory workers in Thailand. Ann Occup Hyg 2008;52:195-205.
[Google Scholar]
|
| 58. |
Febriana SA, Soebono H, Coenraads PJ. Occupational skin hazards and prevalence of occupational skin diseases in shoe manufacturing workers in Indonesia. Int Arch Occup Environ Health 2014;87:185-94.
[Google Scholar]
|
| 59. |
Shiao JS, Sheu HM, Chen CJ, Tsai PJ, Guo YL. Prevalence and risk factors of occupational hand dermatoses in electronics workers. Toxicol Ind Health 2004;20:1-7.
[Google Scholar]
|
| 60. |
Tan HH, Tsu-Li Chan M, Goh CL. Occupational skin disease in workers from the electronics industry in Singapore. Am J Contact Dermat 1997;8:210-4.
[Google Scholar]
|
| 61. |
Goh CL. Irritant dermatitis from tri-N-butyl tin oxide in paint. Contact Dermatitis 1985;12:161-3.
[Google Scholar]
|
| 62. |
Huang J, Wang XP, Chen BM, Ueda A, Aoyama K, Matsushita T. Immunological effects of toluene diisocyanate exposure on painters. Arch Environ Contam Toxicol 1991;21:607-11.
[Google Scholar]
|
| 63. |
Gan SL, Goh CL, Lee CS, Hui KH. Occupational dermatosis among sanders in the furniture industry. Contact Dermatitis 1987;17:237-40.
[Google Scholar]
|
| 64. |
Rantanen T. The cause of the Chinese sofa/chair dermatitis epidemic is likely to be contact allergy to dimethylfumarate, a novel potent contact sensitizer. Br J Dermatol 2008;159:218-21.
[Google Scholar]
|
| 65. |
Goh CL. Occupational allergic contact dermatitis from Rengas wood. Contact Dermatitis 1988;18:300.
[Google Scholar]
|
| 66. |
Kawai K, Nakagawa M, Kawai K, Konishi K, Liew FM, Yasuno H, et al. Hyposensitization to urushiol among Japanese lacquer craftsmen. Contact Dermatitis 1991;24:146-7.
[Google Scholar]
|
| 67. |
Philip M, Alex RG, Sunny SS, Alwan A, Guzzula D, Srinivasan R. A study on morbidity among automobile service and repair workers in an urban area of South India. Indian J Occup Environ Med 2014;18:9-12.
[Google Scholar]
|
| 68. |
Singhi MK, Menghani PR, Gupta LK, Kachhawa D, Bansal M. Occupational contact dermatitis among the traditional 'tie and dye' cottage industry in Western Rajasthan. Indian J Dermatol Venereol Leprol 2005;71:329-32.
[Google Scholar]
|
| 69. |
Ahn YS, Kim MG. Occupational skin diseases in Korea. J Korean Med Sci 2010;25:S46-52.
[Google Scholar]
|
| 70. |
Kanthraj GR, Krupashakar DS, Srinivas CR. Occupational dermatoses among the silk workers. Indian J Dermatol 1996;41:40-1.
[Google Scholar]
|
| 71. |
Guo YL, Wang BJ, Lee JY, Chou SY. Occupational hand dermatoses of hairdressers in Tainan city. Occup Environ Med 1994;51:689-92.
[Google Scholar]
|
| 72. |
Khanna N. Hand dermatitis in beauticians in India. Indian J Dermatol Venereol Leprol 1997;63:157-61.
[Google Scholar]
|
| 73. |
Kishore NB, Belliappa AD, Shetty NJ, Sukumar D, Ravi S. Hand eczema – Clinical patterns and role of patch testing. Indian J Dermatol Venereol Leprol 2005;71:207-8.
[Google Scholar]
|
| 74. |
Chow E, Goh CL. Epidemiology of chronic paronychia in a skin hospital in Singapore. Int J Dermatol 1991;30:795-8.
[Google Scholar]
|
| 75. |
Teo S, Teik-Jin Goon A, Siang LH, Lin GS, Koh D. Occupational dermatoses in restaurant, catering and fast-food outlets in Singapore. Occup Med (Lond) 2009;59:466-71.
[Google Scholar]
|
| 76. |
Rohna R, Ganesapillai T, Salbiah D, Zaiton I. Pattern of occupational allergic dermatitis in the dermatology clinic, Hospital Kuala Lumpur. Med J Malaysia 1999;54:128-31.
[Google Scholar]
|
| 77. |
Rai R, Ahmed T, Nair KR, Srinivas CR. Occupational dermatoses among kitchen workers in a chain of vegetarian hotel. Indian J Dermatol 2003;48:151-3.
[Google Scholar]
|
| 78. |
Committee for Japanese Guideline for Diagnosis and Management of Occupational Allergic Diseases. Japanese Guideline for Diagnosis and Management of Occupational Allergic Diseases 2013. Tokyo: Kyowa Kikaku; 2013.
[Google Scholar]
|
| 79. |
Goh CL, Ng SK. Allergic contact dermatitis to Curcuma longa (turmeric). Contact Dermatitis 1987;17:186.
[Google Scholar]
|
| 80. |
Goh CL, Ng SK. Allergic contact dermatitis to ranitidine. Contact Dermatitis 1984;11:252.
[Google Scholar]
|
| 81. |
Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U, Leggat PA. Occupational health problems of dentists in Southern Thailand. Int Dent J 2000;50:36-40.
[Google Scholar]
|
| 82. |
Smith DR, Guo YL, Lee YL, Hsieh FS, Chang SJ, Sheu HM. Prevalence of skin disease among nursing home staff in Southern Taiwan. Ind Health 2002;40:54-8.
[Google Scholar]
|
| 83. |
Smith DR, Choi JW, Yu DS, Ki M, Kubo H, Yamagata Z. A comparison of skin disease among nursing-home health care workers in Japan and Korea. Saf Sci Monit 2004;8:1-4.
[Google Scholar]
|
| 84. |
Jain A, Chander R, Mendiratta V. Contact dermatitis in nurses and paramedicals in a tertiary care hospital of Northern India. Indian J Dermatol Venereol Leprol 2010;76:566-7.
[Google Scholar]
|
| 85. |
Kuruvila M, Mukhi SV, Kumar P, Rao GS, Sridhar KS, Kotian MS. Occupational dermatoses in beedi rollers. Indian J Dermatol Venereol Leprol 2002;68:10-2.
[Google Scholar]
|
| 86. |
Chatterjee M, Macwan J. Occupational Health Issues of Self Employed Women-Report on Agarbatti and Masala Workers of Ahmedabad. Bombay: Self Employed Women's Association (SEWA), Ahmedabad, Study Commissioned by the Task Force on Health of the National Commission on Self Employed Women; 1988.
[Google Scholar]
|
| 87. |
Noorbala MT. Skin lesions in carpet hand-weavers. Dermatology 2008;14:5.
[Google Scholar]
|
| 88. |
Livingood CS, Rogers AM, Fitz-Hugh T. Dhobie mark dermatitis. JAMA 1943;123:23-6.
[Google Scholar]
|
| 89. |
Chiu CS, Tsai YL. Cheilitis granulomatosa associated with allergic contact dermatitis to betel quid. Contact Dermatitis 2008;58:246-7.
[Google Scholar]
|
| 90. |
Hamdi KA, Al-Malikey M. Frequency of skin diseases among sea fishermen in Basrah. Internet J Dermatol 2008;7:1.
[Google Scholar]
|
| 91. |
Narahari SR, Srinivas CR, Kelkar SK. LE-like erythema and periungual telangiectasia among coffee plantation workers. Contact Dermatitis 1990;22:296-7.
[Google Scholar]
|
| 92. |
Balachandran C, Srinivas CR, Shenoy SD, Edison KP. Occupational dermatosis in coconut palm climbers. Contact Dermatitis 1992;26:143.
[Google Scholar]
|
| 93. |
Yan Y, Wang X, Wu J, Xu L. Occupational skin diseases and prevention among sanitation workers in China. Afr Health Sci 2015;15:768-75.
[Google Scholar]
|
| 94. |
Ishtiaq M, Hussain H, Gul S, Jehan N, Ahmad I, Masud K, et al. Frequency of occupational health problems among coal miners. Gomal J Med Sci 2014;12:52-5.
[Google Scholar]
|
| 95. |
Attarchi MS, Mohammadi S, Asghari E. Evaluation of skin diseases and disorders in photographers. Indian J Occup Environ Med 2009;13:88-91.
[Google Scholar]
|
Fulltext Views
11,028
PDF downloads
3,900





