Translate this page into:
Penile rhinosporidiosis: An unusual presentation and review of literature
2 Department of Dermatology, Rita Skin Foundation, Kolkata, West Bengal, India
Correspondence Address:
Abhijit Saha
Flat No. 115, 1st Floor, Block B, Rishav Palace, 77/26 Ram Lal Dutta Lane, Bhadrakali, Uttarpara, Hooghly - 712 232, West Bengal
India
| How to cite this article: Seth J, Saha A, Mondal AK, Shome K, Samanta AB, Bindal A. Penile rhinosporidiosis: An unusual presentation and review of literature. Indian J Dermatol Venereol Leprol 2017;83:626 |
Sir,
Rhinosporidiosis is a chronic granulomatous infection caused by Rhinosporidium seeberi, a protistan parasite in the class Mesomycetozoea as per its recent taxonomic destination.[1] Nose and eyes being the most common sites, penis and urethra manage to secure much lower rank among the sites of occurrence. Being a disease of world-wide distribution, this menace has managed to intrude into several states of India quite effectively with Tamil Nadu and Kerala being at the top of the list. An increasing number of reports from different parts of West Bengal should sensitize us to know more about the modes of transmission and changing trends of the ecosystem in our state, if any.
A 32-year-old married farmer from Burdwan district, West Bengal, presented to the department of dermatology of Burdwan Medical College, Burdwan, with a pinkish slowly growing polypoid mass arising from glans penis near urethral opening for the last 12 months [Figure - 1]. He had no urinary complaints. There was a history of occasional bleeding following coitus. There was no history of exposure to any professional sex worker or any preceding trauma, and his partner was absolutely healthy. He had no other systemic complaints. Systemic examination was unremarkable. Routine investigations including routine urine microscopy and culture were within normal limits. Screening for human immunodeficiency virus and syphilis were negative. Cystourethroscopy was found to be normal without any urethral involvement. A wedge biopsy was sent for histopathological examination which turned out to be consistent with rhinosporidiosis. Section showed multiple round to oval sporangia of different stages of maturation surrounded by thick chitinous material with a background of chronic inflammatory infiltrate comprising mainly lymphocytes and eosinophils [Figure - 2] and [Figure - 3]. No special stain could be done due to the lack of facility. After the confirmation of diagnosis, the lesion was excised totally and diathermic cauterization of the base was done. The person is on regular follow-up for the last 3 months without any evidence of recurrence.
 |
| Figure 1: Polypoidal mass arising from glans penis near urethral opening and encroaching shaft of the penis |
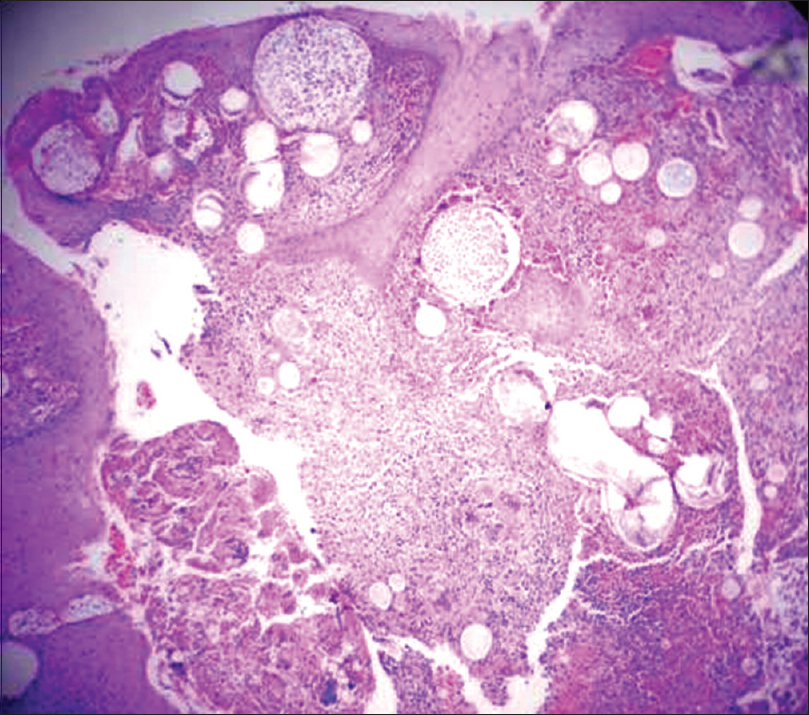 |
| Figure 2: Round to oval sporangia of different stages of maturation with a background of chronic inflammatory infiltrate (H and E, ×10) |
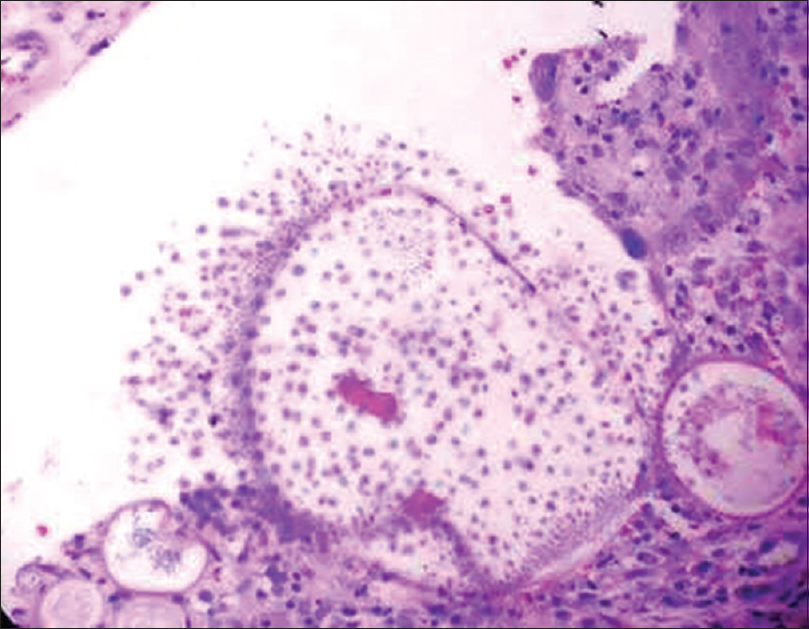 |
| Figure 3: Round to oval sporangia surrounded by thick chitinous material (H and E, ×400) |
The most probable mode of transmission is through traumatized epithelium. Other possible modes are autoinoculation and lymphatic or hematogenous spread. Spread through sexual intercourse is still a matter of controversy. We failed to find out any relevant information regarding the mode of infection in our case.
As nose and eyes are the most common sites of involvement of the infection, routes of transmission might be through air or water. This infection is more common in sand workers, paddy cultivators, who swim or bathe in stagnant water or who dig riverbed. These observations indicate that water and soil may serve as reservoirs of infection. Notably, it is not a contagious disease as person to person transmission is not documented.
Genitourinary rhinosporidiosis is very rare. The first such a case was published in 1941 from India as urethral involvement. Decades later Sasidharan et al. reported a series of 27 cases from India.[2] In 2008, Pal et al. documented five cases from West Bengal.[3] The most recent report was by Pandey et al. in 2014 where the patient, once again from West Bengal, presented with urethral polyp.[4] Our case from Burdwan is the newest addition to this series of patients from Bengal.
The only established mode of treatment is excision of the lesion with wide surgical margin and diathermy of the base. Recurrence rate is high due to incomplete excision and accidental spillage of sporangia to the adjacent tissue. Five cases described by Pal et al. were successfully treated with excision with diathermic coagulation without any recurrence.[3] The case described by Pandey et al. did not show any recurrence following total excision.[4]
Pal et al. dealt with a case of recurrent penile rhinosporidiosis presenting as protruding mass from urethral orifice.[5] The probable cause of recurrence was either reinfection or inadequate resection. However, after the second resection, there was no recurrence during 1-year follow-up period.
In most of the cases of urethral rhinosporidiosis, victims were men from rural background.[3],[4],[5],[6],[7] However, cases of urethral involvement in women were also documented by Sasidharan et al.[2] and Pal et al.[3]
The case described by Pal et al. mimicked penile malignancy, similar to our case.[3] Most of the authors failed to establish any possible mode of infection and definite risk facors.[3],[4],[5] Some of them concluded that taking bath in contaminated pools, followed by abrasion of urethra could be a reasonable explanation.[6],[7] Probably, this holds true for our case too.
The increasing trend of genitourinary rhinosporidiosis in West Bengal should alert us to keep rhinosporidiosis among the differentials in any genitourinary mass whether it is a polypoid or friable growth from the urethra, a penile mass simulating malignancy or condyloma lata or a painful nodule in the vulva. The only difficult part is initial clinical suspicion but with a higher index of suspicion diagnosis becomes easy because of its characteristic histopathological finding.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Arseculeratne SN, Sumathipala S, Eriyagama NB. Patterns of rhinosporidiosis in Sri Lanka: Comparison with international data. Southeast Asian J Trop Med Public Health 2010;41:175-91.
[Google Scholar]
|
| 2. |
Sasidharan K, Subramonian P, Moni VN, Aravindan KP, Chally R. Urethral rhinosporidiosis. Analysis of 27 cases. Br J Urol 1987;59:66-9.
[Google Scholar]
|
| 3. |
Pal DK, Moulik D, Chowdhury MK. Genitourinary rhinosporidiosis. Indian J Urol 2008;24:419-21.
[Google Scholar]
|
| 4. |
Pandey P, Shukla S, Kundu A, Sarkar P. Urethral polyp: An uncommon presentation of rhinosporidiosis. Indian J Dermatol 2014;59:95-6.
[Google Scholar]
|
| 5. |
Pal DK, Bhattacharyya N, Bag AK, Sinha L. Recurrent rhinosporidiosis of male urethra. Indian J Surg 2006;68:97-8.
[Google Scholar]
|
| 6. |
Chowdhury AR, Dey R, Bhattacharya P, Basu S. An unusual case of urethral polyp. Ann Trop Med Public Health 2012;5:530-1.
[Google Scholar]
|
| 7. |
Pal DK, Mukherjee B, Hati GC, Chowdhry MK. Rhinosporidiosis in male urethra. Indian J Urol 2003;19:162-3.
[Google Scholar]
|
Fulltext Views
2,372
PDF downloads
1,146





