Translate this page into:
Developmental retardation in postinflammatory elastolysis and cutis laxa
2 Department of Pathology, PGIMER, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Marg, New Delhi, India
Correspondence Address:
Neha Meena
Department of Dermatology, STD and Leprosy, PGIMER, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Marg, New Delhi - 110 001
India
| How to cite this article: Sharma PK, Meena N, Bhardwaj M, Dixit N. Developmental retardation in postinflammatory elastolysis and cutis laxa. Indian J Dermatol Venereol Leprol 2016;82:195-197 |
Sir,
An 11-month old boy presented to us with red-coloured itchy skin eruptions for two weeks. He was regularly immunized and born to non-consanguineous parents with an uneventful antenatal history. He had a history of jaundice at the age of 7 months and had developed a similar eruption 2 months ago which resolved spontaneously. Cutaneous examination revealed multiple, symmetrically distributed, discrete erythematous papules and excoriations over the cheeks, neck, upper chest, upper and lower extremities including the palms and soles. These papules coalesced to form well-defined round plaques with irregular margins, varying in size from 1 cm × 1 cm to 10 cm × 5 cm over the previously involved skin [Figure - 1]a. The rest of the skin appeared to be normal. Systemic examination revealed hepatomegaly. He also had fever and bilateral axillary lymph node enlargement. Fine needle aspiration cytology from the lymph node revealed reactive lymphoid hyperplasia. The routine blood investigations showed leukocytosis (46,000 cells/mm 3 ) with eosinophilia (38%). Alpha-1-antitrypsin could not be estimated. Hepatomegaly was confirmed on ultrasonography. Histopathology of a papule revealed orthokeratosis, acanthosis, focal thinning of the granular layer and focal mild spongiosis. The mid-dermis showed a mild to moderate interstitial infiltrate of neutrophils, lymphocytes, nuclear debris, occasional eosinophils and focal infiltration into the small blood vessels with perivascular edema [Figure - 2].
 |
| Figure 1: (a) Multiple edematous and erythematous well-defined round plaques with irregular margins on the face. (b) Plaques with collarette of scale and thin rim of erythema. (c) Loose skin folds in the axilla. (d) Generalized laxity of skin giving the appearance of an old man. |
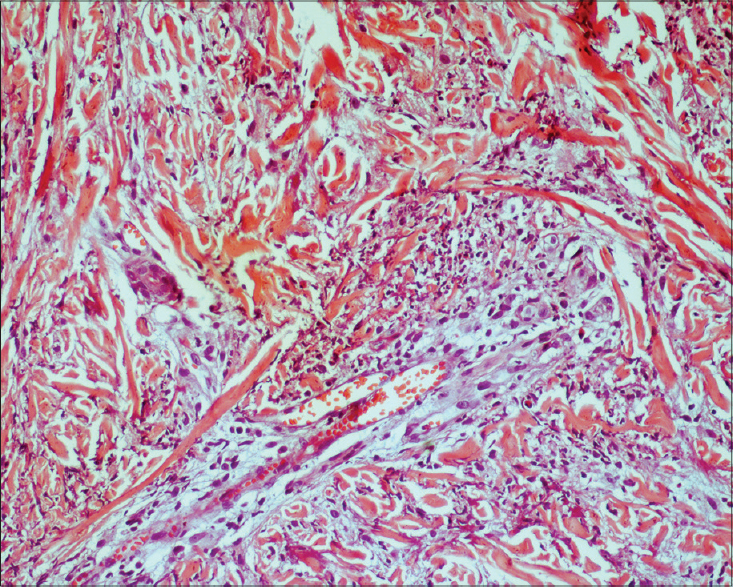 |
| Figure 2: A mild to moderate dermal interstitial infiltrate of neutrophils, lymphocytes, nuclear debris, occasional eosinophils and focal infiltration into small blood vessels (H and E, ×200) |
A follow-up examination at the age of 15 months revealed a decrease in erythema and edema over the plaques resulting in shiny, wrinkled and slightly pigmented skin. The annular plaques had an irregular border with central clearing and the margins were studded with erythematous papules. Some plaques showed a collarette of scale with a thin rim of erythema [Figure - 1]b. These plaques resolved within a month. The skin, which could easily be lifted up, appeared loose and wrinkled similar to that of an old man [Figure - 1]c. Repeat blood investigations showed a reduction in total leukocyte count to 12,000 cells/mm 3 and eosinophils to 7%. A repeat skin biopsy taken from lesional and non-lesional skin revealed an unremarkable epidermis and hypocellular dermis with thick bundles of collagen. There was elastophagocytosis with several histiocytes and giant cells interspersed between the collagen bundles [Figure - 3]a and b. There was a mild perivascular mononuclear infiltrate in the non-lesional skin. Verhoeff-van Gieson stain in both biopsies showed a reduction in elastic fibers, elastolysis and elastophagocytosis in the upper dermis.
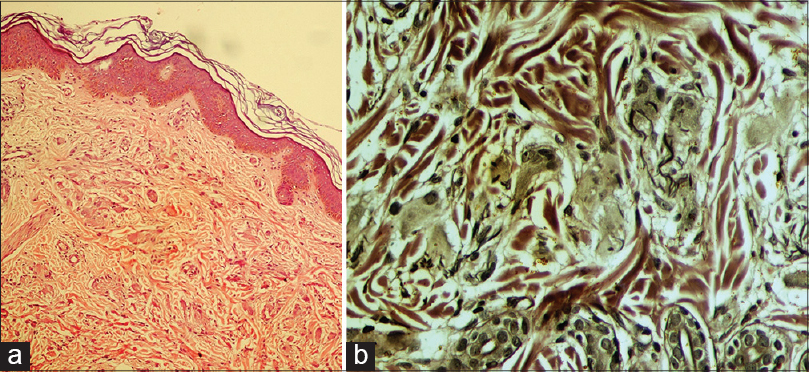 |
| Figure 3: (a) Several histiocytes and giant cells interspersed between hypocellular thick collagen bundles with elastophagocytosis (H and E, ×100). (b) Reduced elastic fibers, elastolysis and elastophagocytosis in the upper dermis (Verhoeff– Van Gieson, ×400) |
The developmental milestones were delayed after the onset of skin lesions. At the age of 23 months, there was no weight gain. He could sit without support and stand with support and dentition was delayed [Figure - 1]d.
Cutis laxa is a group of heterogeneous disorders that results from an abnormality in elastic tissue. It can be either inherited or acquired. Acquired cutis laxa type I is characterized by a generalized or localized inflammatory dermatitis which resolves to leave behind loose and wrinkled skin, with associated systemic involvement. [1] Acquired cutis laxa type II or Marshall syndrome is a postinflammatory elastolysis characterized by an acute onset of erythematous and edematous papules which coalesces to form annular plaques, as seen in our patient. [2],[3]
Histopathologically, stage I of acquired cutis laxa is characterized by fragmentation of elastic tissue. Stage II has a lymph-oneutrophilic infiltrate, stage III shows elastophagocytosis and stage IV is characterized by elastic tissue loss. [4] The elastases produced by inflammatory cells, decrease in elastase inhibitors and abnormal copper metabolism have been implicated in the pathogenesis of Marshall′s syndrome. [4],[5] Low levels of alpha-1 antitrypsin have also been reported. [6] Dapsone and oral prednisolone used in the past have had no effect on the disease outcome. [1],[5]
The interesting findings to note in our patient were a few papules on the palms and soles. He had jaundice and hepatomegaly 2 months prior to the onset of skin lesions. Hepatomegaly has been reported in an infant with acquired cutis laxa. [6] We were unable to find any previous report of delayed milestones and delayed dentition associated with post inflammatory elastolysis and cutis laxa.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
| 1. |
Dyer JA. Lipoid proteinosis and heritable disorders of connective tissue. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick′s Dermatology in General Medicine. 8 th ed. New Delhi: McGraw-Hill Companies, Inc.; 2012. p. 1624-8.
[Google Scholar]
|
| 2. |
Marshall J, Heyl T, Weber HW. Postinflammatory elastolysis and cutis laxa. A report on a new variety of this phenomenon and a discussion of some syndromes characterized by elastolysis. S Afr Med J 1966;40:1016-22.
[Google Scholar]
|
| 3. |
Fontenelle E, Almeida AP, Souza GM. Marshall′s syndrome. An Bras Dermatol 2013;88:279-82.
[Google Scholar]
|
| 4. |
El-Khoury J, Kurban M, Abbas O. Elastophagocytosis: Underlying mechanisms and associated cutaneous entities. J Am Acad Dermatol 2014;70:934-44.
[Google Scholar]
|
| 5. |
Haider M, Alfadley A, Kadry R, Almutawa A. Acquired cutis laxa type II (Marshall′s Syndrome) in an 18- month old child: A case report. Pediatr Dermatol 2010;27:89-91.
[Google Scholar]
|
| 6. |
Hwang ST, Williams ML, McCalmont TH, Frieden IJ. Sweet′s syndrome leading to acquired cutis laxa (Marshall′s syndrome) in an Infant with α1 -antitrypsin deficiency. Arch Dermatol 1995;131:1175-7.
[Google Scholar]
|
Fulltext Views
2,360
PDF downloads
1,570





