Translate this page into:
Pyogenic granuloma with onychomadesis following plaster cast immobilization
2 Department of Pathology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India
Correspondence Address:
Shikha Verma
Department of Dermatology and STD, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong - 793 018, Meghalaya
India
| How to cite this article: Thakur BK, Verma S, Mishra J. Pyogenic granuloma with onychomadesis following plaster cast immobilization. Indian J Dermatol Venereol Leprol 2016;82:239 |
Sir,
Onychomadesis is characterized by separation of the proximal nail plate from the matrix and has been associated with autoimmune diseases, medical illness, infection and drugs. We report a case of pyogenic granuloma with onychomadesis following plaster cast immobilization. We found only 12 previously reported cases of a similar nature indicating that it is a rarely reported condition. [1],[2],[3],[4]
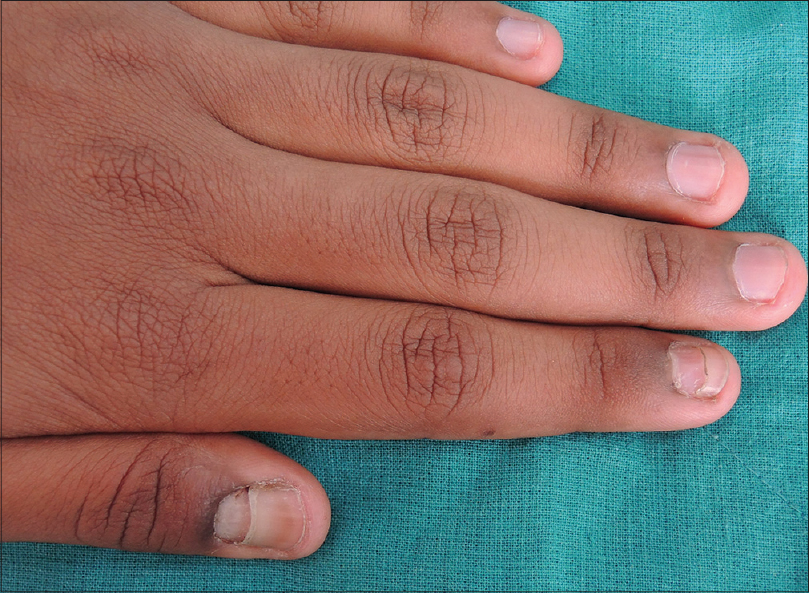
A healthy 14-year-old boy presented with a red nodule on the left thumb for 3 weeks and loss of proximal nail plate of the left index finger for 4 weeks. The patient had developed left distal radio-ulnar joint dislocation following trauma around 3 months back for which a plaster cast was applied from above the elbow up to the metacarpophalangeal joint for 3 weeks. During this period there was no pain, paresthesia or sudomotor change of the fingers of the left hand. One and a half months after the plaster cast was removed, he noticed bleeding from the proximal nail fold of the left index finger and thumb following trivial trauma. It was associated with increased sweating on the cuticular area of these digits. Within a few days, he observed protrusion of red nodules from the proximal nail fold of both left index finger and thumb. The patient was able to pull off the nodule on the index finger; however, he could not remove the thumb lesion. On examination, there was a well-defined erythematous fleshy, transversely elongated nodule on the left thumb involving the proximal nail fold. There was onychomadesis of both left index finger and thumb [Figure - 1]. There was no history of local trauma, drug intake or infection prior to development of the nodule. The routine blood investigations were within normal limits. ELISA for antibodies to human immunodeficiency virus was non-reactive. The nerve conduction and electromyographic tests were normal. The lesion was removed by curettage [Figure - 2] under local anesthesia and sent for histopathological examination which showed features of pyogenic granuloma [Figure - 3]. A final diagnosis of pyogenic granuloma with onychomadesis following plaster cast immobilization was made.
 |
| Figure 1: (a) Pyogenic granuloma of proximal nail fold with onychomadesis of left thumb and index finger, (b) left thumb-nail immediately following surgery |
 |
| Figure 2: Left thumb and index finger at 10 days after surgery |
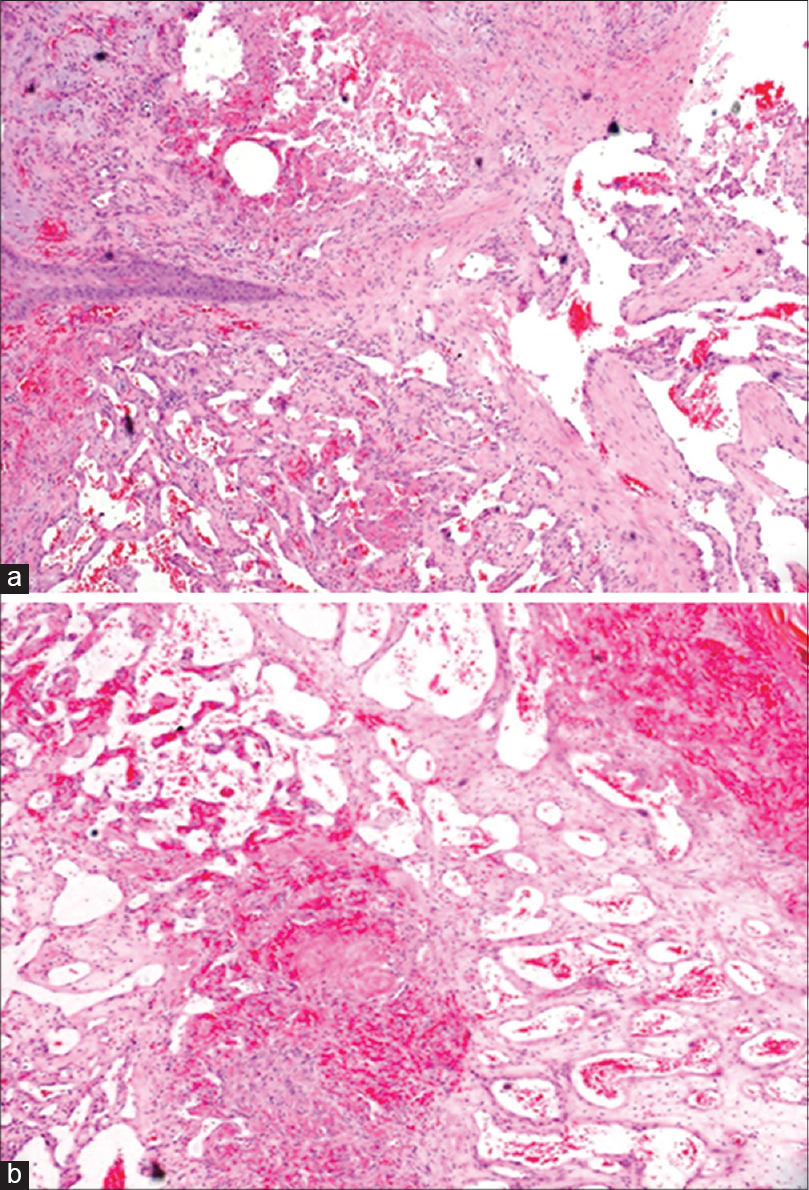 |
| Figure 3: Lobules of dilated and congested capillaries lined by plump endothelial cells in an edematous stroma consistent with pyogenic granuloma (a) H and E, ×400; (b) H and E, ×100 |
Pyogenic granulomas are benign eruptive vascular tumors which may involve the nail folds or be subungual and involve the nail plate. Peripheral nerve injury has been postulated as one of the causes of subungual and periungual pyogenic granuloma. [1] Nail changes are observed in reflex sympathetic dystrophy which represents a severe form of peripheral nerve damage. [5] In 2001, Tosti et al. first reported onychomadesis and pyogenic granuloma following plaster cast immobilization in a series of nine patients. [2] All patients complained of moderate paresthesia and pain of the immobilized hand while wearing the cast and developed painful inflammatory lesions on the finger nail 7-30 days after cast removal. The authors suggested mild peripheral nerve injury could be the cause of pyogenic granuloma and onychomadesis. However, no pain, paresthesia or increased sweating was noted in three other reported patients. [1],[3],[4] Our patient, too, had no pain or paresthesia while wearing the plaster cast but he developed increased sweating in the periungual area of affected nails after cast removal which suggests mild autonomic nerve injury, a finding not noted in previously reported cases. During surgery, we noticed that unlike usual pyogenic granulomas, this nodule was loosely adherent to the surrounding tissue, had a clear plane of separation and could be easily removed by curettage.
The literature suggests that pyogenic granuloma of proximal nail fold of fingers following plaster cast immobilization is always associated with onychomadesis. This point has not been emphasized in previous reports. The mechanism of onychomadesis following plaster cast immobilization is not clear. It is likely that plaster cast immobilization causes peripheral nerve injury which gives rise to a pyogenic granuloma from the nail matrix. The localized inflammation caused by the pyogenic granuloma probably inhibits nail matrix proliferation temporarily resulting in onychomadesis.
The condition may be rarely seen by dermatologists as patients are likely to report to their orthopedician. However, patients presenting with pyogenic granuloma of the proximal nail fold with associated onychomadesis should be asked about preceding plaster cast immobilization and examined for nerve injury. These lesions usually resolve spontaneously but persistent lesions can be easily removed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Piraccini BM, Bellavista S, Misciali C, Tosti A, de Berker D, Richert B. Periungual and subungual pyogenic granuloma. Br J Dermatol 2010;163:941-53.
[Google Scholar]
|
| 2. |
Tosti A, Piraccini BM, Camacho-Martinez F. Onychomadesis and pyogenic granuloma following cast immobilization. Arch Dermatol 2001;137:231-2.
[Google Scholar]
|
| 3. |
Pampín A, Sanz-Robles H, Feltes RA, López-Estebaranz JL. Onychomadesis and pyogenic granulomas after postoperative upper-limb immobilization. Actas Dermosifiliogr 2014;105:528-9.
[Google Scholar]
|
| 4. |
Badri T, Ishak F. Images in clinical medicine. Pyogenic granuloma of the finger. N Engl J Med 2012;366:e10.
[Google Scholar]
|
| 5. |
Tosti A, Baran R, Peluso AM, Fanti PA, Liguori R. Reflex sympathetic dystrophy with prominent involvement of the nail apparatus. J Am Acad Dermatol 1993;29(5 Pt 2):865-8.
[Google Scholar]
|
Fulltext Views
2,997
PDF downloads
1,263





